INTRODUCTION
William Boog Leishman (Fig. 1) was the second surviving son of William Leishman MD, who became Professor of Midwifery at the University of Glasgow, and Augusta Selina Drevar. The family lived at several addresses in the centre of Glasgow, and they also had a country villa at Blairmore on Loch Long.

Fig. 1. Lieutenant General Sir William Boog Leishman KCB, KCMG, FRS.
The young Leishman enrolled at the University of Glasgow when he was just 14. He was not allowed to begin a medical degree until he was 16, so he spent 2 years studying Greek, Latin, Maths and Logic. He came top in his finals, but had to wait until his 21st birthday to be allowed to graduate in medicine. In 1887, he took a commission as surgeon on the Army's Medical Staff, then based at Netley, outside Southampton.
After his training at the Army Medical School, Leishman remained in the UK until 1890 when he was posted to India, taking his microscope with him. He had spent some time at Dum-Dum station, near Calcutta. Dum-Dum was considered to be a particularly unhealthy garrison. From 1894 to 1895 he took part in the Waziristan campaign, attached to the 2nd Battalion of the Border Regiment. He noticed that many of the men suffered from skin ulcers known as Delhi boils. In 1896, he took 3 months leave in Kashmir. His diary of ‘Three months in Kashmir’ has survived, providing some evidence of his attitudes and abilities at that time.
Leishman travelled with another doctor, C. Their trip was interrupted at an early stage when they met the servants of a captain in the 60th rifles. The captain was ill with a severe attack of typhoid. The two doctors could not leave the captain, but they were also unable to obtain any response to their request for medicines from Srinagar. As the possible typhoid treatments at the time included sulphurous acid, chlorine water, charcoal, eucalyptus oil and quinine it is not clear that the captain could have been saved had medicine been available.
During their enforced stop, and as they continued, C proved to be less resilient than Leishman. While Leishman was enjoying the challenges of walking and hunting in the mountains, reaching at least some of the summits without pausing, C found the distances and conditions difficult. Leishman took the time to write a full record of his observations each day, comparing the altitudes reached to the height of Ben Nevis and the roar of the Jhelum to the sound of a heavy sea on Blairmore beach. He sketched a number of scenes, including his tent, which he labelled ‘Fairy Knowe Junior’ after his parents’ home at Blairmore.
Leishman had joined the army shortly after a period of major reform. The low levels of fitness in the army had been exposed during the Crimean War, 1853–1856, when the telegraph kept the British public up to date with events at the battlefront. The news that most deaths of British army personnel were from disease, rather than from enemy action, caused public outrage. The Secretary of State for War, Lord Panmure, responded by sending Dr Robert Lyons and two assistants to report on the patients in the military hospitals; the investigations were to include ‘microscopical examination’ (Panmure, Reference Panmure1855).
Lyons reported that fever, classified as intermittent, remittent, simple continued, relapsing, typhous (sic) or typhoid, was the most prevalent disease. The atmospheric or miasmic theory of disease was still prevalent, and Lyons attributed morbidity to the fatigues of night duty and to the weather.
As a result of this and other investigations and reports on the health of the British Army, in 1860 the Army Medical School was established. Dr William Aitkin, who had been First Assistant to Robert Lyons, was appointed as chair of Pathology. By 1887, when Leishman attended, bacteriology and germ theory were included in the curriculum, and practical work was mainly water analysis and microscopy. In 1892, William Aitkin was succeeded by Almroth Wright. Wright was a civilian, and he made enemies within the army. He was, however, an excellent lecturer and charming to those within his group. He was especially interested in the body's response to infection, and his modern ideas on ‘Alterations in the coagulability of the blood and their bearing on disease’ were inspirational to new recruits from the medical schools.
KALA-AZAR
By this time the idea that diseases had specific, rather than general, causes was gaining acceptance, and Medical Officers were writing reports on their investigations of the organisms responsible for the diseases they observed. In 1880, both the typhoid bacillus and the malaria parasite were described, and from 1882 there were various reports on the possible causes of kala-azar, a form of malarial fever prevalent in Assam. In 1898, Ronald Ross was assigned to work on the transmission of malaria, and also on kala-azar. He did not have time for a full study of kala-azar, but he concluded that the previous authors had failed to clearly define the symptoms of kala-azar, and that this confusion could be the reason for the conflicting reports. Ross described three stages of the disease:
-
Phase 1: acute fever with enlargement of the spleen and liver;
-
Phase 2: acute enlargement of the spleen and liver, with a low fever;
-
Phase 3: cachexia, with no fever (Ross, Reference Ross1899).
Another important feature of the disease is its transmission from patients to others living in close proximity. He wrote that kala-azar is similar to malaria, but differs from ordinary malarial fever in its higher fatality, intractability to quinine, which was normally used to treat malaria, and its communicability. On pathological examination of patients he found very little evidence of parasites in the blood, but Ross considered that the parasites could enter a latent phase. He recommended that all Medical Officers be trained in microscopy to enable more accurate diagnosis, beyond the recording of symptoms.
In 1902, Ross received the Nobel Prize for Physiology or Medicine for his work on malaria. He was an influential figure, and he became an active supporter of Leishman's work.
In 1897, Leishman was appointed assistant to Almroth Wright at Netley. The fact that Leishman took a microscope with him to India suggests that he was already interested in research at that time, and Wright provided the atmosphere and support that he needed to develop.
At Netley Leishman had the opportunity to study patients sent home from India with suspected malaria. Like Ross he used microscopy to help him to make an accurate diagnosis, but he found it difficult to distinguish Plasmodium spp. using the well-known Romanowsky stain. He therefore developed an improved staining method that fixed and stained the sample at the same time. He hoped that the new stain would be valuable in making differential diagnoses of types of malarial fever (Leishman, Reference Leishman1901a ). Although this was a modification of an existing method, for Medical Officers struggling to diagnose malaria in the tropics, this was a huge advance. Colonel Harvey, Leishman's successor as Director of Pathology at the War Office, described it as, ‘as great an advance on previous methods of staining as the breech-loading gun was an advance on the muzzle-loader’ (Balfour et al. Reference Balfour, Harvey and MacPherson1926). In a second paper, he described a further development of the method, and the details of the stained cells (Leishman, Reference Leishman1901b ).
Leishman had observed a number of soldiers invalided home with a remittent fever, anaemia, muscular atrophy and enlargement of the spleen. He considered that the symptoms indicated a specific disease. As the patients had usually been stationed at Dum-Dum, he gave the disease the provisional name of ‘Dum-Dum fever’. In 1900, he examined a private who presented with all the features that he had described. Leishman examined the patient's blood, without finding any evidence of malaria. He took further samples after the death of the soldier and found many small bodies amongst the smears prepared from the spleen, and stained to highlight the chromatin. The regular pattern of the chromatin made it easier to distinguish the bodies from the blood cells as each of the bodies had two chromatin masses; one much larger than the other. These bodies are familiar to current parasitologists as the nucleus (the larger) and the kinetoplast (Fig. 2). At the time he could not identify the bodies, but he kept careful notes and drawings of his observations. It was only in 1903 that he found very similar bodies in the blood of a rat that had died of trypanosomiasis. He referred back to his sketches and slides from 1900 and published his results in May 1903, suggesting that ‘Dum-Dum fever’ was caused by a species of trypanosome (Leishman, Reference Leishman1903).
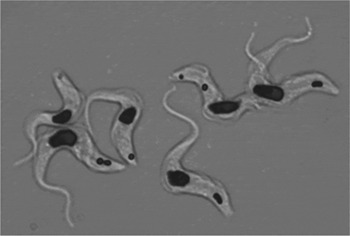
Fig. 2. Trypanosomes, showing the two chromatin masses (dark stain). Image kindly provided by Federica Giordani at the Wellcome Trust Centre of Molecular Parasitology.
He noted that the procedure that he had described could be used to search for similar bodies in smears prepared from patients diagnosed with kala-azar or sleeping sickness.
In July of the same year, Charles Donovan reported that he had earlier found bodies as described by Leishman. Ronald Ross examined Donovan's preparations and agreed they matched Leishman's observations. He concluded that Leishman had identified a novel organism (Ross, Reference Ross1903).
These papers sparked off further research and in July 1904 the Tropical Diseases Section of the BMA ran a symposium: ‘Discussion on the Leishman–Donovan Body’ (Leishman et al. Reference Leishman, Rogers, Donovan, Bentley, Christophers, Castellani, Phillips, Manson, Bruce, Low, Hutchinson, McLeod and Crombie1904). By that time reports had come in of cases in four districts of India, as well as from China, Tunis, Algiers, Arabia and Egypt. The symptoms reported were very similar to those of kala-azar, with dysentery as a frequent complication. Leishman–Donovan bodies had been found in cases of kala-azar, suggesting that Dum-Dum fever and kala-azar were the same disease. David Bruce, who had identified a trypanosome as the causative organism of nagana in cattle, agreed that credit for the discovery should go to Leishman. The new species was eventually named Leishmania donovani.
At the meeting Leishman also noted that very similar parasitic bodies had been found by the French scientists Laveran and Mesnil in cases of ‘Delhi boil’, a tropical ulcer. By 1907 it was recognized that the visceral disease, kala-azar, and the tropical sores were probably caused by different species of the genus, Leishmania. In a review in 1911, Leishman described three species, L. donovani, Leishmania infantum and Leishmania tropica, while accepting that they could possibly be only a single species (Leishman, Reference Leishman1911). It was difficult to separate the species by morphology alone.
Over 100 years later there are at least 20 species of Leishmania known to cause disease in man. Visceral leishmaniasis is still endemic in the Indian subcontinent and East Africa, and many different forms of the cutaneous disease are now recognized. Around 1·5 million people are infected each year. Even with the many more types of data now available the relationships between species are still difficult to resolve (Harkins et al. Reference Harkins, Schwartz, Cartwright and Stone2016).
Leishman was also interested in the details of the transmission of African relapsing fever which, such as kala-azar, had earlier been mistaken for malaria. The discovery of the transmission of the causative spirochaete by a tick had been published in 1905, but the development of the spirochaete within the vector was an outstanding problem of interest to a number of researchers. Leishman dissected the tissues of infected ticks, using staining and microscopy to study the structure of the spirochaete, now known as Borrelia duttoni, within the vector, Ornithodoros moubata. He published a preliminary report on his findings; it has taken another 100 years for the complexity of the genome required for persistence in the tick to become clearer.
Leishman's research on spirochaetes had to end as he began to spend more time on administration and management, particularly during the war years.
LEISHMAN, TYPHOID AND VACCINATION
By 1896, the same year in which Leishman had been unable to treat a case of typhoid in a fellow officer in Kashmir, Almroth Wright was beginning work on an anti-typhoid vaccine. Working at Netley with his assistant, David Semple, he tested the vaccine on a small number of army Medical Officers. They recorded the effects of different doses on the volunteers and the ability of the diluted serum to agglutinate typhoid bacilli as ‘sedimentation units’, noting that the number of sedimentation units was not a reliable indicator of immunity to infection. However, as they expected no adverse effects of vaccination, they recommended that those at risk of infection be vaccinated (Wright and Semple, Reference Wright and Semple1897). There was an opportunity for a trial of the vaccine in the same year, when there was an outbreak of typhoid fever in Maidstone, Kent. Semple proceeded to Maidstone with a supply of vaccine, but had to abandon the work due to an attack of Malta fever. Leishman took his place (Anon, 1897).
In 1898, Wright was appointed to the India Plague Commission, and he used this opportunity to seek further volunteers for anti-typhoid vaccination. Some vaccine was taken out to India from Netley and some was prepared in either Calcutta or Agra, so the doses were not well standardized. The results, in terms of cases of infection and of deaths, were compiled by the Medical Officers stationed with the troops. The differences between the inoculated and uninoculated groups were small, but the authors explained that the inoculated men were mainly those recently arrived in India, who were most susceptible to infection. Also, some inoculations were carried out during a typhoid epidemic, so some men may have been infected before inoculation (Wright and Leishman, Reference Wright and Leishman1900). It was also possible that some cases of ‘enteric fever’ may have been paratyphoid. (The vaccine did not protect against paratyphoid, so cases of paratyphoid may have confounded the results.) The officers of the Indian Medical Service were generally impressed by the overall outcomes, so they recommended that the trials be continued.
Wright obtained further results from troops inoculated in India, Egypt, Cyprus and South Africa, and from patients inoculated in an asylum in Dublin. In 1902, he published a comprehensive report in The Lancet (Wright, Reference Wright1902). The data were still not convincing to those with doubts as to the advisability of compulsory vaccination. There were also fears that a ‘negative phase’ might actually make those recently inoculated more susceptible to infection, so vaccination was suspended. Wright resigned his post at Netley to move to St. Mary's Hospital, London, and Leishman was appointed Professor of Pathology in his stead.
In May 1904, an anti-typhoid committee was established to carry out a thorough investigation of the vaccine and of the value of immunization. Wright was appointed to the committee, but he then resigned. There were several reasons for his disagreement with the committee, one of which was the decision of the committee to ask Karl Pearson, Professor of Applied Mathematics at University College, London, to review Wright's statistics. Pearson was provided with data for five different groups and he decided to test the association between inoculation and escape from infection and between inoculation and recovery separately for each group. On 5 November 1904 he published his results in the British Medical Journal (BMJ), including helpful notes on the Theory of Correlation. He concluded that, as there were irregularities in the results, there was a need for further investigation (Simpson and Pearson, Reference Simpson and Pearson1904). Wright replied the following week, accusing the Medical Advisory Board of hiding, ‘behind Professor Pearson's petticoats’. The argument continued until the end of December, with a new episode appearing in the BMJ each week.
Wright suggested that Leishman should carry out the further experimental work required. Wright and Leishman had already acknowledged the weaknesses in the early trials (Wright and Leishman, Reference Wright and Leishman1900), so Leishman began by designing a series of experiments to standardize the vaccine. This was first tested on himself and his co-workers. Having fixed the strength of the vaccine he carried out a series of tests on volunteers from the 2nd Royal Fusiliers, then at Aldershot. The volunteers were divided into four groups and their reactions to the first and second inoculations were recorded. Blood samples were taken for 26 days, beginning on the day following the first inoculation. Sera were tested for agglutination and other measures of effectiveness. They reported on the dose of vaccine that would produce ‘protective substances’ in blood without an excessive reaction to inoculation. They concluded that agglutinations can be used as a protective index. There was no evidence of a negative phase (Leishman et al. Reference Leishman, Harrison, Smallman and Tulloch1905). The optimum temperature for killing the bacteria and the best conditions for storing the vaccine were also checked. In the earlier work, the temperature had not been properly controlled, and some batches of vaccine had probably been rendered ineffective by the use of too high a temperature. The precise temperature required for sterility of an effective vaccine was found to be 53 °C.
The Anti-typhoid Inoculation Committee considered these interim results and agreed that voluntary inoculation could resume while further research was carried out. To determine the protective effect of the vaccine on troops posted overseas Medical Officers were given specific training for the task and one trained Medical Officer was assigned to each regiment proceeding on foreign service. The previously determined dose and period of 10 days between inoculations were adhered to and the trials were to continue for at least 3 years.
The trained Medical Officers were able to ensure that proper records were kept of all vaccinations, aiming to carry out the inoculations before the troops embarked for their foreign stations. They recorded all cases of enteric fever, carried out blood tests and identified the causative agent, if possible. Leishman collated the results. By 1909 he had the histories of 19 314 people exposed to typhoid; 10 378 were inoculated and 8936 had refused inoculation. The age distribution of the two groups was similar and they were living under the same conditions, so the uninoculated provided good controls.
The histories of the 258 cases of enteric fever were checked by a sub-committee of the Anti-typhoid Inoculation Committee and it was agreed that they were all genuine cases of typhoid fever. The case incidence among the inoculated was 5·39 per thousand and among the uninoculated it was 30·4. The committee recommended that anti-typhoid inoculation in the army should be extended, so the British Army became the first to adopt the vaccine on a large scale. Vaccination remained voluntary.
Initial recognition for Leishman's contribution to the development of the vaccine and in the organization of field trials came in an appointment by the Secretary of State for the Colonies, to the Yellow Fever Commission. Following his experience with the development of the typhoid vaccine, Leishman was fully aware of the need for careful planning and record keeping. He kept notes of how the pathological investigations would be defined and recorded, how cases would be labelled and on the controls needed. At the same time he continued to plan for the production and distribution of the typhoid vaccine in the event of a hurried mobilization. He arranged for further tests to be carried out on the average time of recovery from a single dose of vaccine. He also arranged for the maintenance of a reserve of vaccine and a scheme for the rapid expansion of manufacture.
The work on Yellow Fever came to a halt in 1914, at the outbreak of war, when Leishman was appointed Adviser on Pathology, Western Front. Leishman organized the requisitioning and dispatch of the typhoid vaccine, with strong support from Lord Kitchener, Secretary of State for War. He appealed to the War Office for support in the vaccination of territorials, noting that inoculation had been made compulsory in the US army and regretting the decision against compulsory vaccination in the UK (Leishman, Reference Leishman1914). In December 1914, he was asked by the Director General Army Medical Services, Sir Alfred Keogh, to delay his departure to the front to attend a meeting at the Royal Sanitary Institute on ‘Protective Inoculation against Typhoid Fever’. Both men were concerned to find low levels of inoculated men in some battalions. Leishman blamed ‘the propaganda started by the anti-inoculation people’. He went on to say that he would commit atrocities if he could get hold of them.
As before, accurate diagnosis was essential; so bacteriological evidence was collected during the war. This was easiest for those attached to the British Expeditionary Force (BEF) in France, but there were inevitable errors. Cases of enteric fever were invalided home to a typhoid convalescent depot, and checked to ensure that no carriers were sent back to the Front. In an address in 1921, Leishman expressed the view that efficiency in managing carriers had been an important factor in keeping incidence of enteric fevers low in the BEF (Leishman, Reference Leishman1921). Some comparative data on typhoid and paratyphoid during World War 1 are provided by Siler and Lambie (Reference Siler and Lambie1928). Their counts of cases and deaths from typhoid per thousand men mobilized in the French, German and British armies are shown in the chart above (Fig. 3).

Fig. 3. Typhoid in the French, German and British armies in the Great War. Data from (Siler and Lambie, Reference Siler and Lambie1928).
Both Leishman and Siler and Lambie acknowledge that record keeping was imperfect, and that some cases of paratyphoid were probably included. However, it is difficult to argue against the importance of the contribution made by Wright and Leishman to protecting the troops during the war.
IMPROVEMENTS TO ARMY MEDICAL SERVICES
In his role as Advisor in Pathology with the BEF Leishman had specific responsibility for the collection and analysis of data on enteric fevers and tetanus, but he had a very much wider overall remit for the medical services. The role expanded as new problems emerged, so that it came to encompass both practical administration and the collection of data.
At the practical level Leishman organized the distribution of laboratories and of pathologists, making recommendations on appointments of specialists, equipment and reagents. He provided advice on the supply and employment of sera and vaccines. He was initially also responsible for the co-ordination and inspection of both mobile and hospital laboratories and for the organization and collection of pathological specimens, but he had to delegate some of this work. He collaborated with the BEF's expert on military hygiene and was chairman of the advisory committee on dysentery and of the research committees on trench fever and nephritis. He also liaised with the pathologists working for the armies of the Allies.
He used the data gathered to improve medical services and to provide advice on best practice for those at the front. When it was found that cases of tetanus were much more common than had been expected he was able to secure additional doses of prophylactic serum. For combating communicable diseases such as dysentery preventive measures were important. Additional research on trench fever was carried out in London.
LEISHMAN AND THE MEDICAL RESEARCH COUNCIL
In 1904, while the Army Medical Advisory Board was considering a research programme on anti-typhoid inoculation, the Royal Commission on Tuberculosis published an interim report. They came to the conclusion ‘that it would be desirable not to begin the inquiry by taking evidence, that is to say, by collecting the opinions of others (although this might be desirable at a later stage), but to attack the problem laid before us by conducting experimental investigations of our own’. In promoting the use of public funds for scientific investigations the Commission laid the foundation for the Medical Research Council.
The next step towards the formation of the current MRC came in 1911 when the National Insurance Act made finance available ‘for the purposes of research’. The Medical Research Committee came into being in 1913, with Sir William Leishman as a member. In November 1913, the Committee produced their first ‘Scheme of Research’, but from 1914 to 1918 their focus was on the war effort. During the war the Committee played a crucial role in the integration and support of military and civilian expertise in pathology. In the autumn of 1918, Leishman was again a key figure in the joint response of the Committee and the War Office to the influenza pandemic.
In 1920, the Committee was reconstituted as the Medical Research Council and the National Institute for Medical Research was opened in April of that year. The UK was still recovering from the 1918/1919 flu pandemic, so it was perhaps for this reason that Leishman suggested that viruses should be the initial focus of research at the NIMR. He had a broad view of the approach required, arguing against any division between medical and veterinary research.
In 1918, Leishman became the first Director of Pathology at the War Office, and in 1923 he was appointed Director General Army Medical Services. This last post completed the gradual shift of Leishman's work from research and teaching to administration and leadership.
LEISHMAN AND HIS CONTEMPORARIES
It is interesting to compare here the contributions to science and medicine of Ross, Wright and Leishman.
Ross, the Nobel Prize winner, is perhaps the best known of the three men. After his careful and detailed work in India he joined the Liverpool School of Tropical Medicine. He continued to work on the prevention of malaria and also to develop mathematical models for the spread of the disease. He was a difficult employee, regularly threatening to resign, and, like Wright he had public and acrimonious rows with other scientists.
He was very interested in Leishman's work and they discussed the ‘Leishman–Donovan body’ in a series of letters. Ross helped Leishman to gain recognition for his discovery of L. donovani. They later worked together as members of the Yellow Fever Commission, and with Wright on Blackwater Fever. During World War 1 Ross was given a temporary commission in the Royal Army Medical Corps., acting as an itinerant consultant on malaria.
Wright was clearly an inspirational teacher and, following his work on the typhoid vaccine, he made a second significant contribution to medicine. He joined the BEF as a Consultant Physician, based in a military hospital at Boulogne. Once there he established a bacteriology laboratory, where he was assisted by Alexander Fleming. Together they studied the microbes driven into war wounds by projectiles and developed methods for the management of infected wounds. This work was summarized in an early War Office ‘Memorandum On The Treatment Of The Bacterial Infections Of Projectile Wounds’ (Burghard et al. Reference Burghard, Leishman, Moynihan and Wright1915). Fleming used the experience gained in his later work on penicillin.
Wright supported and promoted those within his circle. As he had many supporters himself he was able to promote his ideas at the highest levels. He asked Ross to join him in nominating Leishman for election to the Royal Society, admitting that he did not understand the politics. He was emphatic in explaining that Leishman had found the parasite years before he published his work. On the other hand, he could also be extremely offensive to those that he considered his inferiors. Giving evidence at a military tribunal he was asked whether he had anything else to add. He replied, ‘No Sir. I have given you the facts. I can't give you the brains.’
Leishman won respect and trust for his careful, thorough and well-presented work throughout the different phases of his career, and for his ability to listen to others. He was able to lead because he also respected his colleagues. His comments on ‘the anti-inoculation people’ were noted because his display of anger was unusual. His devotion to the prevention of disease was entirely characteristic, and he had the political skills to recognize when passion can be helpful.
The various forms of the disease caused by the group of parasites that he discovered were known well before Europeans arrived on the scene, but the cause was unknown. Army Medical Officers, equipped with microscopes, were in a good position to begin the search for the parasites, and the first sighting should probably be attributed to David Cunningham (Cunningham, Reference Cunningham1885). He was looking for the cause of the ‘Delhi boil’, and he noted that the parasites that he found in a sample from a patient could be seen most clearly when he used Gentian violet, because the dye was taken up by the nucleoid bodies. He recorded various stained masses within each cell, but he did not find a pattern. He recognized the importance of further investigation, but he failed to make this clear to the reader. Leishman was able to identify the new organism because he had already developed an improved stain that enabled him to see the two chromatin masses of a kinetoplastid. In addition to his technical skill in microscopy, he wrote beautifully clear descriptions of his results.
Leishman's combination of technical and communication skills also enabled him to progress in the work on an anti-typhoid vaccine. He checked each stage of the production process, accumulating the results that would finally convince those who were unconvinced by the early statistics. In doing so he ensured that, during the Great War, the incidence of enteric fever amongst the British troops was a tenth of that for the French army.
His good humour, resilience and generosity to others shine through his writing. In 1925, he gave an address to the War Section of the Royal Society of Medicine in which he gave advice to new researchers. He defined research as covering ‘any means by which we, of set purpose and on a deliberate plan, strive to add to the existing knowledge of the cause, the prevention and the treatment of disease’ (Leishman, Reference Leishman1925). The researcher, like the fly-fisherman, needs ‘absolute honesty and infinite patience’, the qualities that he displayed in his own research. He should probably have included the dexterity required for tick dissection!
Rather than continuing in research, Leishman moved on to make his contribution to planning, management and leadership in public service. In his address on research he also said, ‘It is impossible to take too much trouble over this planning of the inquiry, for, if every fallacy is not thought of beforehand and guarded against as far as possible, one may waste much effort and have to start afresh’ (Leishman, Reference Leishman1925). The same approach was essential to his teaching and to his organization of the pathology service during World War 1. He was said to be an excellent lecturer, dedicated to his students at the Royal Army Medical Corps, so that the RAMC was well prepared for the challenges it had to face at the outbreak of war.
As Adviser on Pathology with the BEF Leishman had both practical and political responsibilities, balancing competing interests to provide the best possible advice to the Medical Officers at the front. He studied and reported on new problems as they arose, searching for advances that would benefit the troops. After the war, in proposing that virology should be a research focus at the new National Institute for Medical Research he was looking ahead to the new challenges.
Leishman received many awards for his science and for his public service. In 1905, he was made Brevet Lieutenant-Colonel in recognition of his research work and in 1910 he was elected as a Fellow of the Royal Society. He was made a Knight Bachelor and then Knight Commander of the Order of St. Michael and St. George (KCMG) for his public service. He died in 1926, having suffered for some time from a peptic ulcer. He was buried, with full military honours, in Highgate Cemetery, London.
ACKNOWLEDGEMENTS
I would like to acknowledge assistance from Westminster School, the Wellcome Library and the Ross Collection at the London School of Hygiene and Tropical Medicine. I am also grateful to Isabel Vincent for proofreading and to Mike Barrett for the invitation to contribute to this special issue.
FINANCIAL SUPPORT
This research received no specific grant from any funding agency, commercial or not-for-profits sectors.






