Introduction
The World Health Organization (WHO) defined palliative care as the efforts of patients and families who encounter a life-threatening illness to relieve pain and symptoms from the diagnosis of the disease to death and to improve quality of life by providing psychosocial and spiritual support as early as possible. Palliative care accepts death as a normal part of life, aims for the patient to continue living as actively as possible until death and to live a peaceful death, and provides counseling services to the family after death in line with their needs during the grieving process (Worldwide Palliative Care Alliance, 2014).
The gradual increase in the old population and chronic diseases in the world has given palliative care an important place among medical practices. Sixty-nine percent of the general population is adults over 60 years of age, 6% is children and it is estimated that 20 million people need palliative care (Cruz-Oliver, Reference Cruz-Oliver2017). Today, advances in medicine prolong survival and delay death. While scientific and medical developments prevent many diseases or delay their emergence, the methods patients and caregivers resort to for survival also negatively affect the quality of life of patients and caregivers (Inci and Oz, Reference Inci and Oz2012). This philosophy of care not only reduced the length of hospital stay and extended the life of patients but also increased the family's role in care within home care (Cruz-Oliver, Reference Cruz-Oliver2017; Hawley, Reference Hawley2017). Caregivers are the first to evaluate the symptoms of patients, and they have a very important role in applying to hospital early, receiving treatment, and increasing quality of life (Ardahan and Yesilbalkan, Reference Ardahan and Yesilbalkan2010). However, when caregivers who are expected to fulfill all these responsibilities are not prepared for caregiving, this will cause both the patients’ and caregivers’ quality of life to get worse (Berry et al., Reference Berry, Dalwadi and Jacobson2017; Kehoe et al., Reference Kehoe, Xu and Duberstein2019).
Caregivers have a great role in palliative care. Caregivers of palliative care patients have undertaken to meet the needs of the patient in many areas such as treatment monitorization, coping with symptoms related to treatment, emotional, financial, and spiritual support, and personal and medical instrument care (Berry et al., Reference Berry, Dalwadi and Jacobson2017; Kehoe et al., Reference Kehoe, Xu and Duberstein2019). For this reason, caregivers can experience problems in different areas such as conflicts about social roles, tension in marital and family relationships, limitations in daily activities, distress, fatigue, functional sleep disorders, and deterioration in their physical health. In addition, they have stated that they often feel unprepared in caregiving, they do not have sufficient information about illness and care and they do not know how to realize their caregiver roles, how much care the patient needs and how to use the existing resources since they receive little support from health caregivers (Berry et al., Reference Berry, Dalwadi and Jacobson2017; Yilmaz and Sari, Reference Yilmaz and Sari2017; Egici et al., Reference Egici, Can and Toprak2019; Kehoe et al., Reference Kehoe, Xu and Duberstein2019). This situation increases the care burden of individuals and causes them to experience problems during the process of caregiving. Considering the difficult process of palliative care, the caregiver undertakes an extra burden with the responsibility of the patient. This burden can affect the caregiver in a negative way physically and psychosocially in time (Yilmaz and Sari, Reference Yilmaz and Sari2017).
Features associated with care and preparedness for caregiving such as length of care, intensity and type of care, experience, knowledge and training of the caregiver, and changes in the activities of the caregiver are reported as factors influencing the burden of the caregiver (Berry et al., Reference Berry, Dalwadi and Jacobson2017). The patient and the patient's family have the right to be informed fully about the medical facts related to the patient's state, the recommended medical interventions, options related to interventions, possible risks and benefits of each intervention, the course of the diagnosis and treatment, and the right to receive continuous care. Despite this, patients and their families are not informed sufficiently about the course and complications of the disease, recovery, and treatment (Akdemir et al., Reference Akdemir, Bostanoglu and Yurtsever2011). Informing the caregiver on these issues, teaching the necessary skills for caregiving and the methods to facilitate the patient's daily life activities will contribute to caregivers’ preparedness for caregiving. It is the responsibility of nurses to determine and support the preparedness of caregivers, especially those providing care to palliative care patients. In this context, the physical, psychological, or social burden experienced by caregivers due to the caregiving process will decrease.
While there are studies in the literature that evaluate preparedness for caregiving (Silver et al., Reference Silver, Wellman and Galindo-Ciocon2004; Kass, Reference Kass2017) and care burden (Egici et al., Reference Egici, Can and Toprak2019; Kehoe et al., Reference Kehoe, Xu and Duberstein2019) separately, the limited number of studies were found which evaluated the relationship of preparedness for caregiving with care burden (Scherbring, Reference Scherbring2002; Grant et al., Reference Grant, Sun and Fujinami2013; Fujinami et al., Reference Fujinami, Sun and Zachariah2015). For this reason, this study was conducted to evaluate the care burden and preparedness for caregiving of caregivers who were providing care to palliative care patients and the factors influencing these.
Methods
Type of the study
This study is a cross-sectional survey.
Population and sample of the study
The population of the study consisted of 232 individuals who were providing care to patients hospitalized in the palliative care unit of a state hospital in Erzurum between January and May 2019. The sample consisted of 200 (86% participation) individuals who were providing care to palliative care patients and who met the inclusion criteria of the study between these dates. In the power analysis conducted to find out sample size, based on the percentage measurement values, the sample size was calculated as n = 200 with 0.2277 effect size, 95% power, and 0.05 margin of error. With the power analysis conducted, the data collected were found to be sufficient.
Inclusion criteria
The caregiver's being older than 18 years of age, volunteering to participate in the study, having the cognitive and physical ability to answer the data collection tools and not having communication problems (such as hearing, speech, and understanding).
Data collection
The data were collected face-to-face by the researchers by using Caregiver Questionnaire Form, Burden Interview, and Preparedness for Caregiving Scale.
Caregiver Questionnaire Form
This form consists of a total of 29 questions such as age, gender, relation status, marital status, and income status of patient relatives.
Burden Interview (BI)
It was developed by Zarit et al. in 1980. Turkish validity and reliability of the scale adapted into clinic was conducted by Inci and Erdem (Reference Inci and Erdem2006). BI adapted to clinic is a 22-item scale. The lowest score one can get from the 4-Likert type scale is 0, while the highest score is 88. The items in the scale are generally directed to the social and emotional area, and a high score shows that the distress experienced is high. Cronbach's alpha coefficient of the scale is 0.95 (Zarit et al., Reference Zarit, Reever and Bach-Peterson1980). In the present study, Cronbach's alpha coefficient was found as 0.85.
Preparedness for Caregiving Scale (PCS)
The scale was developed by Archbold and Steward with the perspective of role theory in 1983. Turkish validity and reliability of the study were conducted by Ugur et al. in 2017. The scale has 8 items and no sub-dimensions. A 5-Likert type scale was used in the assessment. There are five choices for each question. The caregiver responds to questions ranging from 0 — Not prepared to 4 — Very prepared. The total score of the scale is obtained by adding up the responses to all items. The total score varies between 0 and 32. Cronbach's alpha coefficient of the scale was reported as between 0.67 and 0.92 (Archbold et al., Reference Archbold, Stewart and Greenlick1990; Schumacher et al., Reference Schumacher, Stewart and Archbold2007; Ugur et al., Reference Ugur, Elcigil and Aslan2017). In the present study, Cronbach's alpha coefficient was found as 0.82.
Data analysis
SPSS (Statistical Package for the Social Sciences) 25.0 program was used in data assessment. Shapiro–Wilk normality test was used to find out whether the data were normally distributed. The data were found to be normally distributed. In the statistical analysis of research data, descriptive statistical methods (number, percentage, average, standard deviation, minimum, and maximum value) and parametric tests [t-test in the comparison of two independent groups, one-way ANOVA in the comparison of three or more independent groups, and Tukey HSD Post Hoc test to find out which of the groups were different and relationship tests (Pearson correlation analysis)] were used.
Ethical principles of the study
The study was conducted in accordance with the Declaration of Helsinki. Approval was taken from a University, Faculty of Nursing Ethics Committee (2018-4/1 numbered and 11.06.2018 dated) and written permission was taken from the institutions that the study was conducted in for the study. In addition, written and verbal consent were taken from the individuals who participated in the study after the aim of the study was explained.
Limitations of the study
It should be taken into account that the present study had a limitation. This study was conducted at a single center with a relatively small sample. Therefore, the results obtained from this study are applicable only to the caregivers of patients hospitalized at the palliative care unit of a state hospital in Turkey and cannot be generalized to other caregivers. It is recommended that future studies should be performed in more than one center with larger populations and caregivers of patients with different chronic diseases.
Results
It was found that the average age of the caregivers in this study was 42.6 ± 14.4, 25% were 55 years of age and older, 57% were female, 63.5% were married, 23.5% were the sons of the patients, 28.5% were high school graduates, 56% were unemployed, 35% of the employed participants were working full time, 49.5% were living with their spouses and children, 58% were living with the patient they provided care for, 69.5% did not have chronic disease, 8% of those who had chronic disease had diabetes, 64.5% had income equal to expense, the medical diagnosis of 20% of the patients was stomach cancer, 84.5% did not have difficulty in meeting the expenses of the patient, 42% had provided care between 13 and 24 months, 47% provided care during the night, 61.5% had information about the patient care, 84.5% had been trained about the disease of the patient, and 72.5% of those trained had sufficient training (Table 1).
Table 1. Results about the socio-demographic features of caregivers who participated in the study (n = 200)

The care burden average score of caregivers in the study was found as 33.69 ± 13.03. Caregivers perceived care as a moderate burden. The preparedness for caregiving score average was found as 18.55 ± 6.83. It was found that caregivers were moderately prepared for caregiving (Table 2).
Table 2. Score averages of caregivers’ care burden and preparedness for caregiving scales

A strong positive correlation was found in the study between age and care burden. It was found that the care burden also increased as age increased (p < 0.01). In terms of the degree of relation to the patient, it was found that spouses were more prepared for giving care when compared with daughters, sons, and siblings (p < 0.01), it was found that retired caregivers had a higher care burden than caregivers who worked part time or full time (p < 0.05), caregivers who lived alone had a higher care burden than caregivers who were living with their spouse and children (p < 0.01), caregivers who were not living with the patient had a higher care burden (p < 0.05), and caregivers with chronic disease had a higher care burden than caregivers without chronic disease (p < 0.01). It was found that caregivers with asthma had a higher care burden (p < 0.05) (Table 3).
Table 3. Comparison of caregivers’ care burden and preparedness for caregiving scales average scores according to socio-demographic characteristics
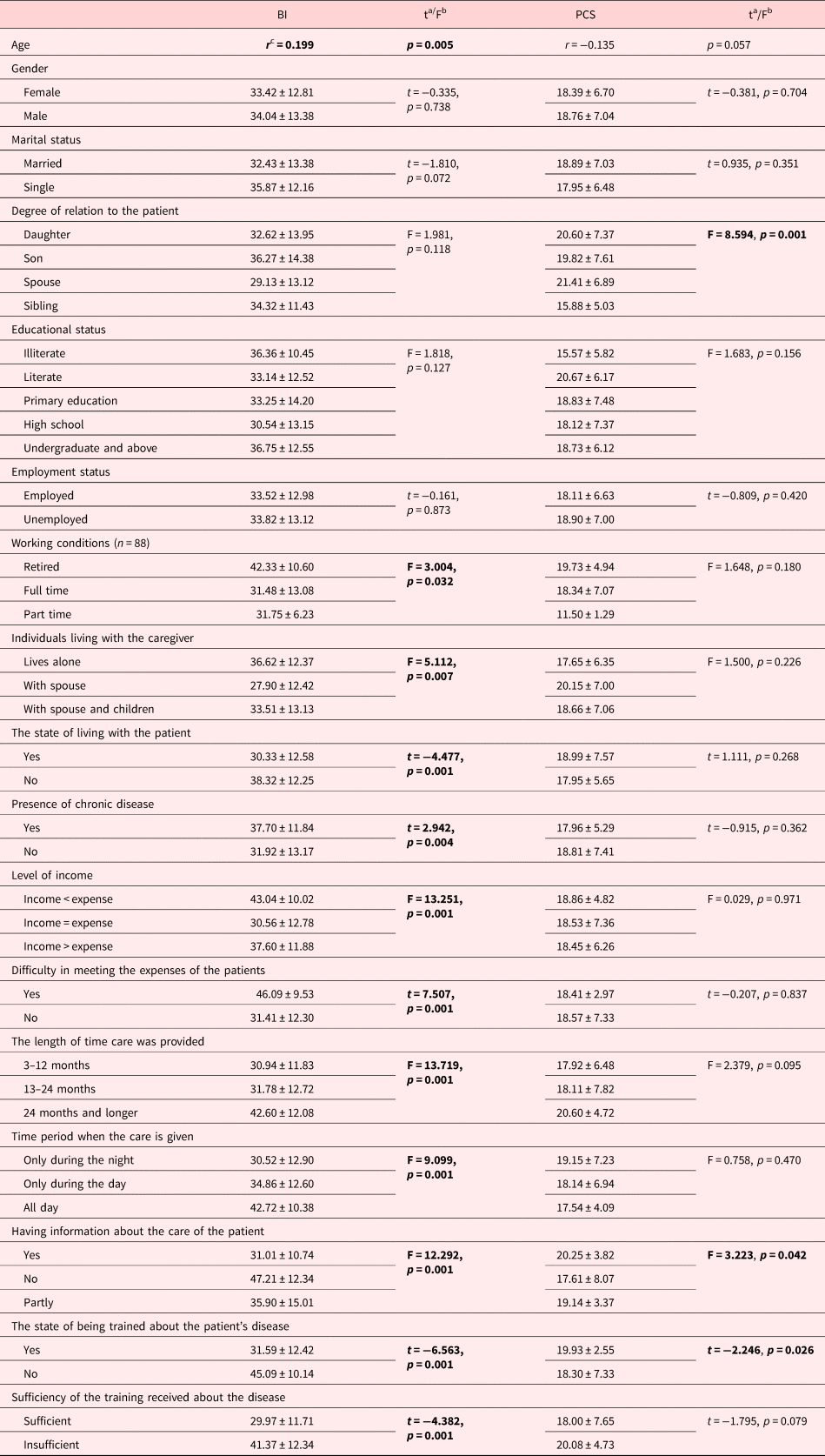
a Student's t-test.
b One-way ANOVA.
c Pearson Correlation. The bold value indicates p < 0.05.
In the study, it was found that caregivers whose income was lower than their expense and those who had difficulty in meeting the expenses of the patients had a higher care burden (p < 0.01) and caregivers who provided care for the patient for 24 months and more and during the day had a higher care burden (p < 0.01). It was found that caregivers who did not have information about patient care had a higher care burden (p < 0.01) and a lower preparedness level (p < 0.05); caregivers who were not trained about the patient's disease had a higher care burden (p < 0.01) and a lower preparedness level (p < 0.05); and caregivers who thought the training they received about the patient's disease was not sufficient had a higher care burden (p < 0.05) (Table 3).
In the study, a statistically significant negative association was found between BI and PCS (p < 0.01). It was found that as preparedness for caregiving level increased, care burden decreased and as preparedness for caregiving level decreased, care burden increased (Table 4).
Table 4. The association between caregivers’ care burden and preparedness for caregiving scales average scores

* Pearson Correlation, p < 0.01.
Discussion
The results obtained as a result of the analysis of research data were discussed in light of the related literature.
It was found in the study that the caregivers perceived the patients they cared for as a moderate burden. Other studies conducted in the literature have stated that caregivers perceive care as a moderate burden (Isik and Erci, Reference Isik and Erci2018; Jafari et al., Reference Jafari, Ebrahimi and Aghaei2018). The process of caregiving is an experience with different dimensions in terms of the caregiver. For example, in their study, Wells et al. (Reference Wells, Dywan and Dumas2005) stated that despite difficulties, patient relatives combined caregiving with positive feelings. Palliative care is also considered as fulfilling a moral duty by providing care to a patient and family members are evaluated as a privileged group for this purpose (D'Angelo et al., Reference D'Angelo, Punziano and Mastroianni2017). When considered in this respect, it is thought that caregivers do not consider caregiving as a big burden. In addition, it has been reported that caregivers who meet the needs of patients in hospital perceive a lower care burden (Cleary et al., Reference Cleary, Freeman and Hunt2006). The fact that the sample of this study consisted of caregivers who provided care to patients treated in hospital can have contributed to this result.
In the study, it was found that as age increased, care burden also increased. In other studies on the subject, it has been stated that the increase in the caregivers’ age increases the care burden and has a negative effect on the quality of care given (Strömberg and Luttik, Reference Strömberg and Luttik2015; Kalinkara and Kalayci, Reference Kalinkara and Kalayci2017). It can be thought that this is because with the increase in their age, physical health problems of caregivers also increase and they experience some problems with meeting the needs of the patients they provide care for.
In the study, it was found that retired caregivers had a higher care burden than caregivers who worked full time and part time. It is also stated in the literature that the employment status of caregivers is an important factor influencing care burden (Van den Heuvel et al., Reference Van den Heuvel, Witte and Schure2001; McCullagh et al., Reference McCullagh, Brigstocke and Donaldson2005). It is thought that the fact that unemployed caregivers are with the patient all the time and have limited time to allocate to themselves and decreased social life contributes to this result.
It was found that caregivers who lived alone had a higher care burden than caregivers who were living with their spouses and children. In the literature, it is stated that individuals living with their spouses and children had a higher care burden due to their familial responsibilities (Tanrikulu, Reference Tanrikulu2019). However, the results of our study are different from the literature. This difference in our study can be resulting from the lack of social support brought by living alone.
It was found that caregivers who did not live with the patient had a higher care burden. Unlike our study, Conde-Sala et al. (Reference Conde-Sala, Garre-Olmo and Turró-Garriga2010) and Vahidi et al. (Reference Vahidi, Mahdavi and Asghari2016) reported that caregivers who lived with their relative they provided care for had significantly a higher care burden when compared with caregivers who did not live with their relative they provided care for. It is thought that the reason why caregivers who did not live with the patient had a higher care burden is because of their routines change, their social activities are restricted and they can work less as a result of the fact that they have to accompany the patient for a specific time in the hospital environment and as a result of the difficulties caused by staying in the hospital.
In the study, it was found that caregivers with chronic disease had a higher burden when compared with caregivers without chronic disease. It was also found in Ozdemir et al.'s (Reference Ozdemir, Sahin and Kucuk2009) and Kalinkara and Kalayci (Reference Kalinkara and Kalayci2017) studies that caregivers with chronic disease had a higher burden and worse health condition. In addition, it has been stated in the literature that when the caregiver's health is not good, the physical strength spent for care will increase and this situation will also increase burden (Karabuga-Yakar and Pinar, Reference Karabuga-Yakar and Pinar2013). It is thought that taking responsibility for both his/her own illness and also the patient's illness increases the care burden perceived by the caregiver.
In the study, it was found that the caregivers who had a lower income than expense and those who had difficulty in meeting the patient's expenses had a higher care burden. Similarly, in Shankar et al. (Reference Shankar, Hirschman and Hanlon2014) and Mashayekhi et al.'s (Reference Mashayekhi, Pilevarzadeh and Rafati2015) study, it was found that caregivers with a low level of income had a higher care burden. In the literature, it has been reported that special care needs for dependent individuals cause an increase in care costs and consequently burden care (Jeong et al., Reference Jeong, Myong and Koo2015). It is thought that the psychological burden caused by not being able to meet the needs of the patients economically during the care process increases the care burden.
It was found that caregivers who provided care to patients for 24 months and during the day had a higher care burden. Studies conducted have found that it was important for how long caregivers continued their caregiving roles and that care burden increased as caregiving time increased (Pinquart and Sörensen, Reference Pinquart and Sörensen2007; Salama, Reference Salama2012). Naturally, daily time allocated for providing care to the patient affects burden care (Grant et al., Reference Grant, Sun and Fujinami2013; Pehlivan et al., Reference Pehlivan, Ozgur and Yildiz2018).
It was found that caregivers who did not have information about patient care, those who were not trained about the patient's illness and those who thought the training they received was not sufficient had a higher care burden. It is well-known that palliative care support develops the feelings of security and compliance in the continuity of care. It is important for caregivers to be informed in time in order to make them feel like the part of a health team, to help them in planning care and participating in care services (Tuna and Olgun, Reference Tuna and Olgun2010; Reigada et al., Reference Reigada, Pais-Ribeiro and Novella2015). Thus, it is stated that caregivers who are sufficiently informed about the patient's disease and care will have increased psychosocial adaptation and those who are prepared for care will have decreased care burden (Corvin et al., Reference Corvin, Chan and Tezak2017; Pehlivan et al., Reference Pehlivan, Ozgur and Yildiz2018).
It was found in the study that caregivers were moderately prepared for caregiving. It was found in Henriksson and Årested (Reference Henriksson and Årestedt2013) and Gonzalez et al.'s (Reference Gonzalez, Polansky and Lippa2014) study that caregivers had the moderate level of preparedness for caregiving score average (Henriksson and Årestedt, Reference Henriksson and Årestedt2013; Gonzalez et al., Reference Gonzalez, Polansky and Lippa2014). The results of our study were found to be similar to studies conducted in the literature.
In our study, it was found that the caregivers who were spouses of the patients were more prepared for caregiving. Due to the patriarchal family structure and traditional lifestyle in our country, women in the house such as spouses, daughters, and daughters-in-law are considered to be responsible for the care of family members (Tanrikulu, Reference Tanrikulu2019). Considering this aspect, it is thought that caregivers do not consider caregiving as a big burden and they are more prepared for care.
It was found that caregivers who were informed about the care of the patient and those who were trained about the patient's illness had higher preparedness levels. Similarly, it was found in Gonzalez et al. (Reference Gonzalez, Polansky and Lippa2014) and Holm's (Reference Holm2016) studies that training given to caregivers increased their preparedness levels (Gonzalez et al., Reference Gonzalez, Polansky and Lippa2014; Holm, Reference Holm2016). In the literature, the necessity of caregivers’ being informed about medical facts related to the state of the patient, medical interventions, options for interventions, possible risks and benefits of each intervention, facilitating methods while fulfilling the patient's daily life activities, and simple nursing practices are emphasized. It is reported that by this way, the caregiver who is informed about the care and illness of the patient will participate in the care of the patient and this will contribute to the caregiver's preparedness (Tuna and Olgun, Reference Tuna and Olgun2010; Henriksson and Årestedt, Reference Henriksson and Årestedt2013).
In our study, it was found that as the preparedness level increased, care burden decreased and as the preparedness level decreased, care burden increased. After individuals with chronic diseases need home care, family members find themselves in an unprepared caring role. For this reason, it is very important to find out the needs of the caregivers and to plan appropriate interventions in the early stages of the disease so that a good care is provided to the patient, the caregiver adapts to his/her role and problems experienced are reduced (Grant et al., Reference Grant, Sun and Fujinami2013; Henriksson and Årestedt, Reference Henriksson and Årestedt2013). Studies conducted have also found that caregivers’ preparedness for caregiving has a positive effect on care burden and increases patients’ quality of life and the quality of care provided (Scherbring, Reference Scherbring2002; Grant et al., Reference Grant, Sun and Fujinami2013; Henriksson and Årestedt, Reference Henriksson and Årestedt2013; Ugur et al., Reference Ugur, Elcigil and Aslan2017).
In the study, it was found that caregivers perceived the patients they provided care for as moderate burden. It was found that care burden increased as age increased and caregivers who were retired, those who were living alone, those who were not living with the patient, those who had chronic disease, those who had income lower than expense, those who had difficulty in meeting the expenses of the patient, those who had provided care for the patient for 24 months and longer, those who provided care for the patient all day, those who were not informed about the care of the patient, those who were not trained about the illness, and those who thought their training was no sufficient had a higher care burden. In addition, it was found that caregivers were moderately prepared for caregiving. It was found that caregivers who were the spouses of the patient, those who were informed about the care of the patient and those who were trained about the illness had a higher preparedness level. It was found in the study that care burden decreased as the preparedness level increased and care burden increased as preparedness for caregiving decreased. The study results indicated that preparedness increased in direct relation to a decreased level of care burden among caregivers of patients hospitalized in palliative care service. Nurses will contribute to decreasing care burden by finding out the preparedness levels of caregivers providing care for palliative care patients, training them with information and skills for the care in order to increase their preparedness, finding out the problems of caregivers, helping the caregiver in realizing his/her strength, guiding the caregiver to suitable resources, and informing the caregiver about possible physical and emotional problems. Thus, nurses will plan nursing interventions by considering the factors that affect the care burden and preparedness of caregivers.
Acknowledgments
The authors are grateful to all participants who agreed to participate voluntarily in this study.







