Introduction
Leeches in the Family Praobdellidae share the propensity of parasitism on mammalian mucous membranes in their life history (Phillips et al., Reference Phillips, Arauco-Brown, Oceguera-Figueroa, Gomez, Beltrán, Lai and Siddall2010). According to previous clinical reviews, praobdellid leeches mostly parasitize the upper airway in humans, with the nasal cavity being the most common site of infestation (Raza et al., Reference Raza, Shabbir and Anwar-ul-Haq2006; Saki et al., Reference Saki, Rahim, Nikaghlagh and Saki2009; Chen et al., Reference Chen, Chien, Yang, Li and Hwang2010). Leech infestation as a foreign body in the human respiratory tract has been reported mainly in Asia, the Mediterranean and Africa (Chen et al., Reference Chen, Chien, Yang, Li and Hwang2010). Based on the distributions of praobdellid species and the images shown in previous clinical reports, it is likely that Dinobdella ferox (Blanchard, 1896) along with Limnatis nilotica (Savigny, 1822) and Myxobdella africana Moore, 1939 have been the species frequently parasitizing humans in these regions. Regarding the distribution, D. ferox occurs in South, Southeast and East Asia (Sawyer, Reference Sawyer1986; Lai and Chen, Reference Lai and Chen2010). On the contrary, L. nilotica occurs in Middle East, Southern Europe and North Africa (Sawyer, Reference Sawyer1986; Bahmani et al., Reference Bahmani, Eftekhari, Mohsezadeghan, Ghotbian and Alighazi2012) and M. africana occurs only in Africa, mostly in the eastern countries (Sciacchitano, Reference Sciacchitano1967; Cundall et al., Reference Cundall, Whitehead and Hechtel1986; Sawyer, Reference Sawyer1986).
Among praobdellid leeches, D. ferox is the most reported and studied species. Cases of D. ferox infestation in the upper airway, the symptoms and subsequent complications (including recurrent unprovoked or intermittent epistaxis, increasing sneeze and cough, nasal obstruction, sensation of itch and of the existence of a moving foreign body in the nasal cavity, hemoptysis, hematemesis, and sometimes even anemia and dyspnea), as well as the clinical treatments of host patients have been documented in numerous reports and reviews (Chow et al., Reference Chow, Wong, Ho and Lau2005; Tseng and Ho, Reference Tseng and Ho2005; Chuang, Reference Chuang2008; Adhikari, Reference Adhikari2009; Saki et al., Reference Saki, Rahim, Nikaghlagh and Saki2009; Chen et al., Reference Chen, Chien, Yang, Li and Hwang2010; Verma et al., Reference Verma, Preetam, Sikka and Thakar2011; Chakraborty et al., Reference Chakraborty, Bhatia and Dey2015; Hsu et al., Reference Hsu, Kao and Yang2015). Moreover, the life history and behaviours of D. ferox have been investigated in several studies in the last century. Moore (Reference Moore, Harding and Moore1927) described the parasitic and free-living forms of D. ferox in India, and argued that these two forms implied intermittent, facultative parasitism in the life history of D. ferox. They also documented a method to remove D. ferox from domestic animals, in which a bowl of water or milk was held in front of the host animal's nostrils, and D. ferox can be captured and extracted when it emerged at the nostrils. Later, Keegan et al. (Reference Keegan, Toshioka and Suzuki1968) examined specimens of D. ferox from Japan, Vietnam and Taiwan, and described the small size and the coloration of juvenile D. ferox. The characterization documented by Keegan et al. included behavioural reactions and the searching pose of juvenile leeches shown in a picture. In addition, an experimental infestation was conducted in the nasal cavities of a rabbit with seven juvenile D. ferox in Keegan's study, in which the leeches were extracted from the host rabbit 30 days after the introduction of the leeches using the same technique described by Moore (Reference Moore, Harding and Moore1927), i.e. holding a dish of water up to the nose of the rabbit. Up to the end of the 20th century, however, D. ferox infestation was merely documented once more in a veterinary case report (Pryor et al., Reference Pryor, Bergner and Raulston1970), and the biology of D. ferox had been overlooked for decades.
At the beginning of this century, the host specificity of D. ferox, its growth curve in the parasitic period and the behavioural propensity of free-living individuals before and after the parasitic period were studied by Wang et al. (Reference Wang, Tong, Yang, Shen, Wu, Lu and Kuo2005). They found that, first, juvenile D. ferox were only able to parasitize mammalian hosts but not avian or amphibian hosts. Second, the growth curve of D. ferox was apparently correlated with host size; the mean biomass of D. ferox parasitizing host rabbits increased faster than those in host rats over a month. In addition to the symptoms and complications of the hosts, host mortality induced by D. ferox infestation was documented in their experiment. Moreover, as previously documented (Keegan et al., Reference Keegan, Toshioka and Suzuki1968), it was also shown in Wang's study that D. ferox before parasitizing preferred to stay around the water surface and were sensitive to airflow and vibration from hosts. In contrast, leeches after parasitizing preferred to stay on the bottom and were inactive to those clues from hosts.
Despite abovementioned studies on the behaviour, life history and host specificity, our knowledge of D. ferox in the parasitic period and its influences on hosts, especially humans, has remained limited. Although the symptoms and complications of human hosts have been documented and reviewed in previous clinical case reports (Chow et al., Reference Chow, Wong, Ho and Lau2005; Tseng and Ho, Reference Tseng and Ho2005; Adhikari, Reference Adhikari2009; Chen et al., Reference Chen, Chien, Yang, Li and Hwang2010; Verma et al., Reference Verma, Preetam, Sikka and Thakar2011; Hsu et al., Reference Hsu, Kao and Yang2015), systematic observation and record of symptoms and complications, in particular the chronology of the occurrence of symptoms (e.g. epistaxis and anemia), have never been conducted in human or any host species. Furthermore, since all D. ferox in previous case reports were removed forcedly from the human hosts, the occurrence of D. ferox detaching from a human host voluntarily without manual operation has never been documented. Nevertheless, Moore (Reference Moore, Harding and Moore1927) mentioned that D. ferox are attracted to water close to the host nostrils and can be induced to emerge from the host nostril. Through this technique, a parasitizing D. ferox can be captured and removed non-invasively (or even without any manual operation, see Keegan et al., Reference Keegan, Toshioka and Suzuki1968). However, how long it might take a parasitizing D. ferox before it is attracted to water has never been examined. Consequently, the factors determining the attraction of parasitizing D. ferox to water and the triggering of their emergence have remained unknown.
In this study, the author was infested voluntarily by juvenile D. ferox to investigate their behaviours and document the subsequent symptoms. In the parasitic period, the behaviours of D. ferox and the symptoms were recorded by the author immediately after their occurrence. Meanwhile, complete blood count examinations (CBC) and nasal endoscopy examinations (NE) were conducted regularly to observe and record the parasitizing leeches as well as to investigate its impacts on a human host systematically and chronologically
Materials and methods
General information of the juvenile D. ferox and the host
In May 2016, one juvenile D. ferox was collected from a shallow stream (25°11′28.0″N, 121°33′42.5″E) in Yangmingshan National Park in Taipei City, Taiwan. Five more juveniles were collected from a shallow stream (23°58′11.1″N, 121°28′46.0″E) in Tongmen Village of Jian Township in January 2017, and 10 more juveniles were collected from the same habitat (23°30′07.0″N, 121°27′15.7″E) in Chimei Village of Reisui Township in August 2017 (both townships are in Hualien County, Taiwan). All juveniles were highly responsive to warm and moist airflows as well as moving shadows. When detecting these cues, these juvenile D. ferox assumed a searching pose: standing on their caudal suckers, stretching their bodies into the air and slowly waving their heads to search for nearby potential hosts. One leech was selected from each collection for voluntary infestation. The body masses of the three selected juvenile D. ferox were 0.008, 0.003 and 0.004 g, respectively, and the lengths were 2–4 mm in resting pose and about 10 mm in searching pose (Fig. 1a and b). The voluntary host is a male of age 35, 1.74 M in height and 70 kg in weight, without any history of nasal allergies.
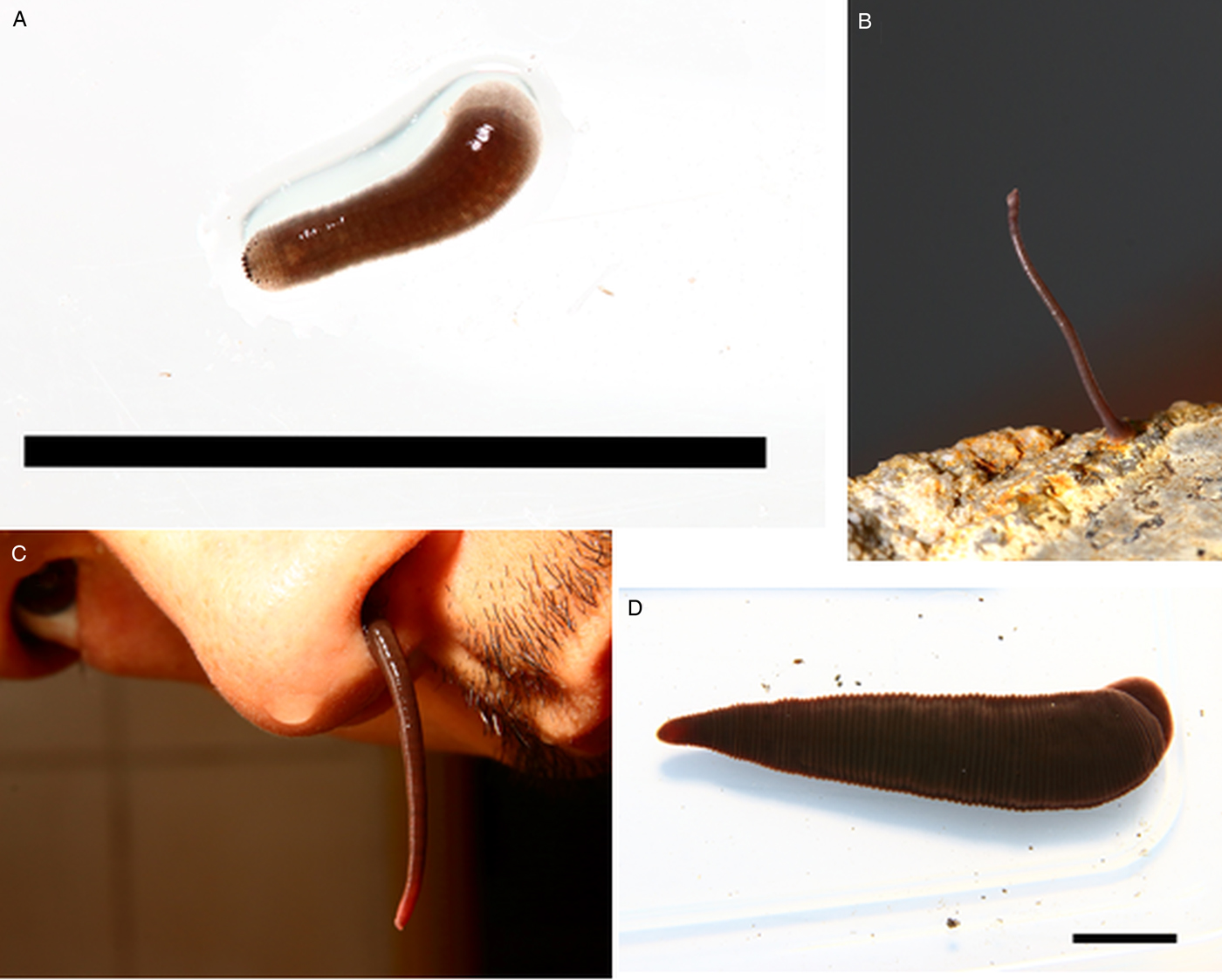
Fig. 1. Dinobdella ferox (Blanchard, 1896) in different periods of life history. A juvenile leech in rest pose (a) and in searching pose (b) before infestation, as well as an individual protruding the head out of the host nostril in the parasitic period (c) and an individual with genital pores resting in water after the parasitic period (d). The scales represent 1 cm in (A) and (D).
Voluntary infestations
Voluntary infestations were conducted of one leech at a time in three trials in 1 June 2016, 1 February 2017 and 30 August 2017, respectively. In these voluntary infestations, the juvenile D. ferox were introduced onto the skin below one of the host nostrils and were allowed to crawl freely. Each introduction was recorded in videos (see the Supplementary materials).
Systematic observations in the parasitic period
The CBC and NE were conducted regularly to assess the influences of D. ferox on the host. To document the condition of the host prior to D. ferox infestation, the first CBC was conducted in a local clinical laboratory within the 10 days before each voluntary infestation. Subsequent CBCs were conducted in the same laboratory about every 10 days after the introduction. On the other hand, NE was conducted by Dr Wan-Ju Jian in his ear, nose and throat (ENT) clinic weekly after the introduction to observe the parasitizing leeches, document their attachment sites and estimate their sizes. In addition to the CBC and NE, the author also documented the behaviours of the parasitizing D. ferox and the subsequent oropharyngeal and nasopharyngeal symptoms (e.g. moving in the nasal cavity, movements into the nasal vestibule, or emerging at the nostril) if they were visible with a mirror.
Finally, the technique described by Moore (Reference Moore, Harding and Moore1927) to remove a parasitizing D. ferox from a host was tested in the study to investigate the efficacy and when it is applicable. During the parasitic period of the first leech, the author had conducted the technique by sinking the nose and face into tap water of room temperature for nearly 30 s weekly. In this weekly procedure, the emergence of the D. ferox at the host nostril was recorded, thus providing information on the attraction to water.
Diet examination in the free-living period
After the parasitic period of the three tested D. ferox, freshwater insects, worms, freshwater snails, freshwater crabs and other available animal tissues were collected and provided as prey to the free-living leeches to compare these results with the previous studies on free-living praobdellid leeches (Moore, Reference Moore, Harding and Moore1927; Keegan et al., Reference Keegan, Toshioka and Suzuki1968; Wang et al., Reference Wang, Tong, Yang, Shen, Wu, Lu and Kuo2005; Nakano et al., Reference Nakano, Tomikawa, Sakono and Yoshikawa2017). Finally, these D. ferox were fixed and preserved in 95% ethanol, and would be donated and deposited in Academia Sinica in Taiwan in the near future.
Results
General information of the tested D. ferox and their parasitic periods
During the introduction of the voluntary infestations, each juvenile moved directly into the nearest nostril in 1 min following the warm airflows of normal breathing of the host. The parasitic period of each juvenile D. ferox lasted for 49 days, 75 days and 24 days, respectively (Fig. 2). The parasitic period of the first leech was terminated after the leech was manually extracted from the nostril by the host on the 49th day after introduction (Fig. 2a). In contrast, the parasitic period of the second leech ended naturally on the 75th day after introduction, on which the leech exited voluntarily from the host's nostril into water (Fig. 2b). The third leech was discharged with the snivel already on the 15th day after introduction and reintroduced immediately into the host nostril. Nevertheless, after the third leech was repeatedly discharged from the nostril during sneezing on the 23rd and 24th days after introduction, the leech was not reintroduced to the host nostril and the parasitic period of the third leech was terminated (Fig. 2c).

Fig. 2. The behaviours of three tested D. ferox and the host symptoms in their parasitic periods. Circles with dotted lines, triangles with dashed lines, and squares with solid lines represent the symptoms of blood stained in sputum, of blood stained in snivel and of epistaxis, respectively. The vertical reference lines in (a) and (b) indicate the day that the parasitizing leech started emerging at the host nostril, while the asterisks in (c) indicate the days that the parasitizing leech was discharged in snivel and sneezing by the host.
The body masses of the three D. ferox increased remarkably after the parasitic period. The body mass of the first leech increased from 0.008 to 1.66 g (ca 200 times, 20 750% increase, Fig. 1a–d) in 49 days, while the body mass of the second leech increased from 0.003 to 1.15 g (ca 380 times, 38 333% increase) in 75 days. In contrast, the body mass of the third leech increased from 0.004 to 0.07 g (ca 17 times, 1750% increase) in 24 days. Additionally, the first two D. ferox at the end of their parasitic periods presented their genital pores, while the third D. ferox presented no genital pores when it was discharged out of the nostril as the end of the parasitic period.
Systematic observations in the parasitic period
The behaviours of the parasitizing D. ferox and the subsequent symptoms were observed and recorded in detail by the voluntary host. The size of the parasitizing D. ferox increased sufficiently in and after the third week of the parasitic period such that presence and movements could be observed directly through the nostril in the mirror or even touched in the nasal atrium or vestibule by the host's fingertip. Furthermore, the first and the second D. ferox started protruded its head out of the nostril on the 27th and 35th days after introduction, respectively (Fig. 2a and b), and this head-protruding behaviour occurred frequently hereafter until the end of the parasitic periods of both leeches.
The oropharyngeal and nasopharyngeal symptoms included nasal obstruction and congestion, higher frequency of sneezing, occasional itching and mild stinging pain in the nasal cavity, sensation of a moving foreign body in the nasal cavity, rhinorrhea and bleeding-related symptoms such as blood-stained sputum and snivel and recurrent epistaxis (Fig. 2). Among these symptoms, itching, mild stinging pain, the sensation of a moving foreign body in the nose, rhinorrhea and recurrent epistaxis generally occurred after the end of the second week after introduction, while other symptoms occurred intermittently from the very beginning of the parasitic period. All these symptoms except the bleeding-related ones had occurred until the end of the parasitic period. Interestingly, the occurrence of the bleeding-related symptoms (i.e. blood-stained sputum and snivel and epistaxis) increased gradually from the beginning of the parasitic period and decreased right until after the parasitizing D. ferox started protruding its head out of the host nostril. Eventually, these symptoms ceased completely two to three weeks before the end of the parasitic period (Fig. 2a and b).
Since the bleeding-related symptoms ceased completely two to three weeks before the end of the parasitic period, the final CBCs were conducted accordingly. During the parasitic period of the first leech, blood-related symptoms ceased completely after the 37th day after introduction, and the final CBC was conducted around the 40th day after introduction (Table 1; Fig. 3). Similarly, during the parasitic period of the second leech, blood-related symptoms ceased completely after the 54th day after introduction, thus the final CBC was conducted around the 50th day after introduction (Table 1; Fig. 3). In contrast, the parasitic period of the third leech was terminated prematurely, and the final CBC for this infestation was conducted around the 20th day after introduction (Table 1; Fig. 3).
Table 1. The WBC differentials of the host in CBCs in the parasitic periods of the three D. ferox

The CBC around the 20th day after the introduction of the first leech was not conducted due to the lack of access to a CBC procedure on a personal trip. Otherwise, the CBC was conducted until the parasitizing leech finished its intermittent blood feeding completely.

Fig. 3. CBC examinations of the host prior and during the parasitic periods. Full circles with the solid line, open circles with the dotted line and full triangles with the dashed line indicate the first, the second and the third parasitic period, respectively. The area between the upper and lower reference dashed lines represent the normal range of the values for a male adult. The CBC around the 20th day after the introduction of the first leech was not conducted due to the lack of access to a CBC procedure on a personal trip abroad. Otherwise, the CBC was conducted until the blood feeding of the parasitizing leech was finished.
The influence of the parasitizing D. ferox on the human host was investigated empirically and systematically for the first time with CBCs. Quantities of red blood cell (RBC), haematocrit and haemoglobin remained in the normal range throughout all three parasitic periods (Fig. 3). In addition, other RBC-related tests (i.e. mean corpuscular volume (MCV), mean corpuscular haemoglobin (MCH), mean corpuscular haemoglobin concentration (MCHC)) as well as the white blood cell count (WBC) and the platelets of the host in CBC were barely influenced by D. ferox infestation (Fig. 3). The WBC differentials in CBC also remained in normal ranges (Table 1) during all three parasitic periods. The only abnormal value was the MCH on the first day after the first introduction, yet it was unlikely that a parasitizing juvenile leech could have caused such result within one day.
The NEs were conducted weekly after the introductions until the nasal leeches had grown in size that rendered NE inconvenient and unlikely. In spite of the fact that NEs were only conducted during the parasitic periods of the first and second leeches, they nevertheless showed that the sizes of D. ferox increased remarkably in the parasitic periods and that the attachment sites of parasitizing leeches in the host nasal cavity changed frequently (Table 2). Notably, the second leech was not observable in NE for two weeks during the parasitic period despite the fact that the leech was large enough to protrude out of the host nostril from the nasal turbinate (Table 2). Therefore, the attachment sites were not always identifiable by NE.
Table 2. The attachment sites and estimated sizes of the parasitizing D. ferox

The NE at ca 28 days after the introduction of the first leech was not conducted due to the lack of access to the ENT clinic on a personal trip. Otherwise, the NE was not conducted because the parasitizing leech was remarkably grown in size and rendered NE inconvenient and unlikely.
Finally, by immersing the nose and face in water at room temperature for nearly 30 s weekly in the parasitic period of the first leech, it is shown that Moore's (Reference Moore, Harding and Moore1927) method of removing a parasitizing D. ferox was effective only later in the parasitic period. The method was able to attract parasitizing D. ferox out of the nostril only after the leech started performing head protrusion behaviour (i.e. the 28th day after introduction in the parasitic period of the first leech). After the onset of head protrusion behaviour, D. ferox always emerged from the nostril when the host was washing his face or taking a shower. In addition to the presence of water near or in the host nostril, a dark environment could also induce the parasitizing leech to emerge. Examples included when the host turned off the light in the room before sleep, when the host went to see a movie in the theater, or even when the host was riding a scooter through a long, dark tunnel in the daytime.
Diet examination in the free-living period
After the parasitic period, all three D. ferox were kept alive for months (12 months for the first leech; 10 months for the second leech and two months for the third leech) to examine their diets. Tubifex worms, chironomid larvae, unidentified juvenile earthworms, freshwater snail Austropeplea ollula, unidentified dragonfly nymph, unidentified damselfly nymph, freshwater crab Candidiopotamon rathbunae, fresh corpse of earthworm Amynthas sp., fresh corpse of zebra fish Danio rerio, fresh corpse of goldfish Carassius auratus, pithed American bullfrog Lithobates catesbeianus, even raw chicken egg yolk and unfrozen raw pork liver were provided as prey to these free-living D. ferox. However, no foraging or feeding behaviours had been observed from them, and the diets of free-living D. ferox were unable to be evaluated in this study.
Discussion
Through voluntary infestation, this is the first study documenting the behaviours of parasitizing D. ferox and the chronology of host symptoms in the parasitic period. The life history of D. ferox was consistent with what was described previously (Moore, Reference Moore, Harding and Moore1927; Keegan et al., Reference Keegan, Toshioka and Suzuki1968; Lai and Chen, Reference Lai and Chen2010). Juvenile D. ferox could parasitize mammalian hosts, in which they fed on blood from the mucous membranes and grew rapidly. In this study, the body masses of the first two leeches increased remarkably from 0.008 to 1.66 g (ca 200 times) and 0.003 to 1.15 g (ca 380 times) and also presented their genital pores at the end of their parasitic periods. Furthermore, the second D. ferox exited the host voluntarily in this study, which led to the first infestation of D. ferox documented in human without manual interruption. In contrast, the body mass of the third leech increased just from 0.004 to 0.07 g (ca 17 times) and presented no genital pores when it was discharged out of the nostril as the end of the parasitic period.
This study revealed more details of the parasitic period of D. ferox. It is reported for the first time that the bleeding-related symptoms ceased completely weeks before the end of the parasitic period. Since these symptoms should have mainly resulted from the blood oozing after the feeding of parasitizing leeches on the host's mucus membranes, it is indicated that D. ferox stopped feeding weeks before it left the host. In addition, the first emergence of the leech at the nostril was found to coincide with the beginning of decrease in bleeding-related symptoms. Moreover, after the first head-protruding behaviour, a parasitizing D. ferox was lured out of the nostril by the presence of water. It avoided bright lit areas and habitats and thus was attracted by a dark environment. According to Moore (Reference Moore, Harding and Moore1927), a parasitizing D. ferox has to return to water thus the reproductive system may be fully developed in the free-living period. It is likely that D. ferox are able to mate with each other after full development of the reproductive system, and apparently D. ferox have to lay their cocoons in mud (Keegan et al., Reference Keegan, Toshioka and Suzuki1968). To a parasitizing D. ferox, water near or in the host nostril and a dark environment are signs of cooler and moister conditions or, even better, aquatic environments, which would reduce the potential for the leech to desiccate after leaving the host. Therefore, it is likely that the function of head protrusion is to determine whether the environment around the host nostril is suitable for the leech to transition to the free-living period.
The onset of head protrusions and the associated cessation of blood feeding suggested that the parasitic period of D. ferox could be at least separated into an early phase, an intermediate phase and a terminal phase. The early phase corresponds to the period before the first emergence at the nostril, in which the parasitizing D. ferox feeds frequently from different sites, grows rapidly and the host has bleeding-related symptoms. According to the result, the host experienced little discomfort in addition to bleeding-related symptoms in the first two weeks of the early phase, yet the nasal obstruction and congestion, higher frequency of sneezing, itching, mild stinging pain, the sensation of a moving foreign body in the nose and rhinorrhea along with recurrent epistaxis occurred more intensively in the later early phase. The first emergence at the nostril marks the beginning of the intermediate phase, in which the parasitizing D. ferox starts to be attracted by water and darkness. Based on the records in this study, the parasitizing leech decreased blood feeding gradually in this phase, and thus its growth is likely to be slower as a result. According to the NE records, the parasitizing leech still changed the attachment sites to fit its growing body in the intermediate phase. Finally, the terminal phase starts after the parasitizing D. ferox ceases its blood feeding completely. Based on the records in this study, the parasitizing leech protruded its head out of the host nostril frequently in this phase, even when there was no water nearby. Additionally, due to the increasing size of the parasitizing D. ferox, the host experienced severe nasal obstruction and congestion, the sensation of a moving foreign body in the nose and at the nostril, as well as higher frequency of sneezing, itching and rhinorrhea resulted from the protruding head of the leech in the intermediate phase and the terminal phase,
In this study, the first two parasitizing D. ferox reached the terminal phase and also developed their genital pores. This suggested that a parasitizing D. ferox might only exit from the host voluntarily when it presented the genital pores. However, despite the appearance of the genital pores, the internal reproductive system of D. ferox in the end of the terminal phase might still be rudimentary or underdeveloped as mentioned in previous studies (Walton, Reference Walton1955; Keegan et al., Reference Keegan, Toshioka and Suzuki1968) and thus required further development during the free-living period (Moore, Reference Moore, Harding and Moore1927). Further studies on the development of internal and external reproductive systems are needed to fully reveal the timing of the exiting in the terminal phase and the biological cues that might trigger its onset.
The duration of the parasitic period might depend on the host size. In this study, the parasitic period of the first leech lasted for 49 days (7 weeks) until the leech was removed manually, and the parasitic period of the second leech lasted for 75 days (ca 11 weeks) until the voluntary exiting of the leech. In comparison, the parasitic period of D. ferox in cow might last for half of a year (local cattle farmer, personal communication; see also Moore, Reference Moore, Harding and Moore1927), which was much longer than the parasitic period (7–11 weeks) in the human host in this study. In comparison, the parasitic period of D. ferox in a host of small size, such as a rat and a rabbit, lasted for merely 2–4 weeks, and was terminated because of the death of the host due to suffocation (Wang et al., Reference Wang, Tong, Yang, Shen, Wu, Lu and Kuo2005).
Although the technique to remove a parasitizing D. ferox was reported by Moore nearly a century ago (Moore, Reference Moore, Harding and Moore1927) and its effectiveness has been documented (Keegan et al., Reference Keegan, Toshioka and Suzuki1968), the duration of the parasitic period of D. ferox in which the technique is effective has never been investigated empirically and systematically. This study showed that the technique was only effective after the onset of head protrusion behaviour, i.e. when the parasitizing D. ferox could be observed easily and frequently at the nostril. In spite of not knowing the duration of the parasitic period of D. ferox in which this technique was effective, this technique has been practiced by doctors in Nepal (Adhikari, Reference Adhikari2009). In Taiwan, this technique was also reported by ENT doctors (Hsu et al., Reference Hsu, Kao and Yang2015) and practiced by veterinarians on pets infested by D. ferox (Chang et al., Reference Chang, Cheng, Tung, Yang and Lee2006). Interestingly, due to the smaller size of pet dogs or cats than a human host, the early phase of the parasitic period for D. ferox might be merely around two weeks (Yung-Huei Hsu, personal communication). Therefore, the owners became aware of the infestation either via the emergence of the leech at the nostrils of the pets or the symptoms preceding the emergence. In either case, the parasitizing leeches would already be in the intermediate phase of the parasitic period, which explained why Moore's method was generally effective.
By regularly-conducted CBC, this study also showed that no signs of anemia or other significant physiological impacts on the adult male host had been reported throughout the parasitic period of D. ferox. Such result is similar to a previous case report of a 27-year-old female in Taiwan (Hsu et al., Reference Hsu, Kao and Yang2015), but different from another case report of a 70-year-old female in Taiwan (Chuang, Reference Chuang2008). On the other hand, cases of leech infestation resulting in severe or even lethal anemia have been reported mostly in South Asia, the Middle East and East Africa (Turner, Reference Turner1969; Cundall et al., Reference Cundall, Whitehead and Hechtel1986; Aali, Reference Aali2002; Demiroren and Caliskan, Reference Demiroren and Caliskan2003; Ağin et al., Reference Ağin, Ayhan, Gülfıdan, Çevık and Derebaşi2008; Montazeri et al., Reference Montazeri, Bedayat, Jamali, Salehian and Montazeri2009). Even though the species causing the infestations was not always identified in those cases, the common praobdellid species in these areas are L. nilotica and M. africana rather than D. ferox.
In this study, the weekly conducted NE in the voluntary infestations revealed that the sizes of D. ferox increased remarkably in the parasitic period, and the attachment sites of the parasitizing leech in the host nasal cavity changed over time. Shigemi and Suzuki (Reference Shigemi and Suzuki2009) argued that a live leech moved around the nasal cavity to escape human immune reactions, thus a D. ferox infestation did not result in symptoms of foul-smelling purulent secretion and nasal stiffness with mucosal swelling, which were commonly induced by the immune responses of neutrophils against foreign objects. Similarly, the symptoms reported in NE along with the WBC count and the WBC differentials in CBC indicated minor immune responses of host nasal mucosa against the parasitizing D. ferox in this study.
The parasitizing D. ferox might be difficult to detect in NE according to the records in this study. In the early phase of the parasitic period, D. ferox were often too small and hiding too well to be observed or visualized completely. Furthermore, despite that the second leech in this study was large enough to visibly protrude out of the host's nostril from the nasal turbinate in the ENT clinic, the leech was still unable to be detected in NEs for two weeks. In addition to this study, a previous medical case (Chen et al., Reference Chen, Chien, Yang, Li and Hwang2010) also reported that NE was unable to diagnose the nasal leech infestation in a 74-year-old male, who had suffered from occasional epistaxis for 1 month, until computer tomography was used to locate the leech. In both cases, it is obvious that a parasitizing D. ferox, despite its size, was able to conceal itself well in the host nasal cavity.
In conclusion, this study documented for the first time the behaviours of parasitizing D. ferox and the subsequent symptoms through voluntary infestations of a human host. The first head protrusion behaviour coincided with a gradual decrease of feeding activities, and the parasitizing D. ferox would cease blood feeding completely weeks before voluntarily exiting the host. In addition, it was feasible to attract the parasitizing D. ferox to emerge from the nostril with water only after the first head protrusion behaviour. Parasitism of D. ferox did not impact the health of the adult male host significantly in this study, and the parasitizing leech might not be detected in NE. Overall, the results in this study provided valuable information on the behaviours of D. ferox during the parasitic period and will likely promote better diagnoses and treatments of D. ferox infestations in humans and mammalian pets.
Supplementary material
The supplementary material for this article can be found at https://doi.org/10.1017/S0031182019000751.
Author ORCIDs
Lai Yi-Te, 0000-0003-4906-1202.
Acknowledgements
The author thanks Dr Chi-Yun Kuo deeply for his kindly proof reading and valuable comments to this manuscript. Dr Wan-Ju Jian and members in his ENT clinic, as well as the medical examiner in Ho-Ping Health Center are appreciated for their medical suggestions and assistances. The comments and suggestions from two anonymous reviewers have remarkably improved the manuscript and were deeply appreciated. The generosity of those persons who had helped in this study will be kept in the memory by the author.
Financial support
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Conflict of interest
None.
Ethical standards
The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008. The principles outlined in the WMA Declaration of Helsinki were followed while the author himself was infested voluntarily with nasal leeches in this study. The author, who has studied leech biology for more than 15 years, has completely understood the potential risks of the infestation with the nasal leech. In the parasitic stage of the nasal leech, the author has the full ability to determine the discomfort of the symptoms, and was also able to determine with the doctor if the parasitizing nasal leech should be forcedly removed due to the health issue of the author through the regularly-conducted CBCs and NEs. In addition, since this study was conducted independently by the author in the leisure hours without any support of funding/grant, no ethics approval was able to be accessed.
Availability of data and material
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.








