Introduction
Congenital heart disease comprises a broad field with many different diagnoses and wide-ranging anatomical variations of all kinds. This enormous variation is probably responsible for the relative lack of guidelines and consensus documents on the subject, especially when compared with structural ‘adult’ heart disease.
Nevertheless, guidelines and consensus documents are important because their intention is to optimize decision-making based on a critical review of the literature, including the most recently published papers, and on the personal experience of professionals in the field. This consensus document on the common arterial trunk (CAT) has been compiled by task force members of the European Association for Cardio-Thoracic Surgery (EACTS) and the Association for European Paediatric and Congenital Cardiology (AEPC). Task force members were chosen according to their specific expertise with the goal of being able to encompass the full spectrum of CAT. The members of the task force have given a full disclosure of any conflicts of interests and relations with industry. There are no known conflicting interests or relations with industry that might have influenced the recommendations in this document.
The authors of this document have strictly adhered to the Methodology Manual for EACTS Clinical Guidelines that was published in 2015. Reference Sousa-Uva, Head and Thielmann1 The task force has performed a complete review of the existing literature, and all available data were carefully weighed to determine their usefulness to construct recommendations and statements. There are no randomized or prospective studies on CAT, and most of the available literature consists of retrospective patient series (with a few multicenter studies being the exception). High-level evidence is therefore not readily available and most evidence is level C (Table 1).
Table 1. Levels of evidence.

Because this is a consensus paper, recommendations are often not backed by strong evidence. Therefore, the task force has chosen to limit the number of recommendations (Table 2) and instead to make statements intended to assist and facilitate clinical decision-making.
Table 2. Classes of recommendations.

The task force has aimed for completeness by including all relevant topics related to the management of CAT. In rare cases of CAT, ventricular hypoplasia is present, which precludes the construction of a biventricular circulation. Forms of CAT with hypoplasia of 1 of the ventricles are sometimes named here when relevant, but, because the management is typically completely different, they are not topics of this consensus document.
Background
CAT, also known as persistent truncus arteriosus or truncus arteriosus communis, is a rare form of congenital heart disease characterized by a common ventriculo-arterial junction, connecting to a single artery that gives rise to the aorta and the pulmonary and coronary arteries. There is a single arterial valve [truncal valve (TrV)] between the cardiac ventricles and the common truncal artery. The TrV typically overrides an outlet type of ventricular septal defect (VSD). Atrial septal defects type 2 (ostium secundum type) are frequently found.
Development of CAT is thought to be related to abnormal development of neural crest cells or to their aberrant interaction with second heart field cells, but its exact aetiology is still not known. CAT is closely associated with the 22q11.2 deletion syndrome, and mutations in genes encoding NKX and GATA transcription factors may also be related to the development of CAT. Reference Ta-Shma, Pierri and Stepensky2
Associated cardiovascular anomalies are common in CAT. The TrV is frequently malformed and regurgitant. Obstruction is rare but not completely absent. The valve is most often bi-, tri- or quadricuspid, and the valve leaflets may be dysplastic and fibrotic in some instances. The coronary arteries do not rise from an aorta but from a CAT and are therefore considered anomalous. The position and course of the coronary arteries are frequently abnormal. The origin of the pulmonary arteries (PAs) can vary, and, in some instances, 1 PA does not arise from the common artery.
A right aortic arch is commonly found with CAT, and an interrupted aortic arch (IAA) is present in 15–20% of all patients with CAT. IAA is mostly type B, and ductal patency is needed for perfusion of the lower half of the body. Apart from CAT with IAA or severe narrowing of the transverse arch, a ductus arteriosus is extremely rare in all other forms of CAT. Reference Collet and Edwards3–Reference Calder, Van Praagh and Van Praagh5
Without surgical treatment, CAT is usually fatal. Delay of surgery may lead to an early onset of pulmonary vascular obstructive disease. In the last few decades, treatment of CAT has improved considerably, and current surgical mortality should be no more than 5–10% for solitary CAT. The majority of patients will need reinterventions, usually of the right ventricular outflow tract (RVOT) (conduit replacement/revision) and TrV.
Methodology
The task force has chosen to categorize this manuscript into the following chapters: Genetics and morphology, prenatal diagnosis and management, preoperative management and surgery (including reoperations and percutaneous reinterventions), postoperative management in the intensive care unit (ICU), assessment during long-term follow-up and current outcomes of CAT treatment.
We performed a systematic review of non-randomized data in the literature. Publications older than 25 years—except for literature on cardiac morphology and nomenclature—and case reports were excluded from analysis. Exceptions to this rule are mentioned separately. Existing documents on the management of CAT have been consulted when necessary. 6 Expert opinions were sought on controversial or uncertain issues for which we were unable to find sufficient evidence in the current literature. A critical appraisal of the available evidence was carried out and summarized in tables wherever possible; potential limitations of the reviewed publications were carefully provided. Consensus was sought to derive from the analysed data recommendations or statements to aid in practical and clinical decision-making.
Peer review was performed by reviewers selected by the EACTS Guidelines Committee, in collaboration with the Editor- in-Chief of the European Journal of Cardio-Thoracic Surgery. After the document was revised and finally approved by both the EACTS and AEPC, the manuscript was subsequently submitted for publication to the European Journal of Cardio-Thoracic Surgery and to Cardiology in the Young.
Genetics of common arterial trunk
CAT is one of the rarest forms of congenital heart disease, with an overall incidence of 0.03–0.056/1000 live births, accounting for 0.21–0.34% of all cases of congenital heart disease. 6,Reference Lindinger, Schwedler and Hense7 In Europe, the average recorded prevalence is 1 per 10 000 pregnancies (including live births, stillbirths and terminations of pregnancy). 6,Reference Lindinger, Schwedler and Hense7 Many foetuses that spontaneously abort in the first trimester of pregnancy have a major congenital heart disease. Half of first trimester spontaneous abortions (50%) are associated with a major chromosomal abnormality; the nature of the congenital heart disease will not have been recognized in this group. The incidence of CAT is higher antenatally, both because of documented in utero deaths and also because of termination of pregnancy in a significant minority of cases. Reference Volpe, Paladini and Marasini8,Reference Boudjemline, Fermont and Le Bidois9
Even in the absence of a prenatal diagnosis, it is to be expected that a neonate will have clinical signs within the first 6 weeks of life; therefore, few cases are missed diagnostically, although a few may die before they reach a paediatric cardiology unit. Hence the postnatal incidence of CAT is likely to be broadly correct.
Studies of both the recurrence risk of CAT and of other congenital heart disease suggest a higher risk for CAT than for the majority of other causes of major congenital heart disease. Reference Pierpont, Gobel, Moller and Edwards10–Reference Ferencz, Correa-Villasenor and Loffredo14
Simple CAT (with no associated cardiac malformations except for a VSD) has a low recurrence risk of 1.6%. In contrast, complex CAT, which includes other cardiac defects, most commonly a right aortic arch, IAA, abnormal coronary artery origin and persistent left superior caval vein, has a higher recurrence risk of up to 13.6%. The overall risk of recurrence is 6.6%. Reference Pierpont, Gobel, Moller and Edwards10,Reference Yamagishi, Rickert-Sperling, Kelly and Driscoll11
22q11.2 deletion syndrome
The 22q11.2 deletion syndrome (also known as DiGeorge syndrome, velocardiofacial syndrome or CATCH22) accounts for the majority of genetic causes of CAT. The 22q11.2 deletion syndrome has an overall incidence of 1:4000. It is the most common microdeletion syndrome and the major genetic cause of CAT.
Confirmation of the diagnosis of the 22q11.2 deletion would have been difficult before the mid-1990s when fluorescence in situ hybridization was introduced, allowing rapid, accurate diagnosis both pre- and postnatally. The immune deficiency associated with the 22q11.2 deletion syndrome could not be confirmed prior to 1965, when it became possible to examine lymphocyte subsets. Reference Iserin, de Lonlay and Viot15
Of children with the 22q11.2 deletion, 80% have congenital heart disease, of which 10% is CAT; 35% of patients with CAT have a 22q11.2 deletion. Reference Momma, Ando and Matsuoka16–Reference Marino, Digilio and Dallapiccola21 Although the majority of cases of 22q11.2 deletion arise de novo, because there is decreased reproductive fitness in patients with the syndrome, a significant number of parents are affected, albeit much more mildly than their offspring, with CAT. The overall carrier frequency for a parent is between 6 and 28%; therefore, it is recommended that parents of an affected child be offered testing for the 22q11.2 deletion. Reference Digilio, Angioni and De Santis22 The recurrence risk in de novo cases of the 22q11.2 deletion in future pregnancies is negligible.
Other chromosome abnormalities associated with common arterial trunk
Array comparative genomic hybridization (aCGH) is now routinely used in some developed countries for chromosome analysis pre- and postnatally in babies identified with congenital abnormalities, but it is not universal.
Microdeletions of 8p23.1 and 18q11.2 are also associated with CAT. A deletion of 8p23.1 harbours the gene GATA4 and 18q11.2, the gene GATA6. These are important transcription factors in cardiac development. Other c3hromosomal disorders with documented CAT include trisomy 13 and rarely trisomy 21. Mosaic trisomy 8 Reference Sherer, Dalloul, Pinard, Sheu and Abulafia23 has been identified and may be missed on blood chromosome analysis. Other microdeletions have also been rarely associated with CAT (Table 3).
Table 3. Chromosome abnormalities identified in patients with common arterial trunk.

CAT = common arterial trunk.
Single gene disorders associated with common arterial trunk
A number of syndromes have been associated rarely with CAT: These include CHARGE syndrome 2° mutations in CDH7 and possibly very rarely in SEMA3E syndrome and Matthew Woods syndrome 2° mutations in STRA6.
Autozygosity mapping using next generation sequencing in a consanguineous population in Saudi Arabia has identified mutations in NRP1 and PRKD1, both autosomal recessive disorders. Reference Shaheen, Al Hashem and Alghamdi24
Other single gene disorders include GATA4, GATA6, Reference Chao, McKnight, Cox, Chang, Kim and Feldman25 TBX1, TBX20, Reference Huang, Wang and Xue26 NKX2-5 and PLXN-D1 Reference Ta-Shma, Pierri and Stepensky2 (Tables 4 and 5).
Table 4. Single gene mutations identified in patients with isolated common arterial trunk.

AD = autosomal dominant; AR = autosomal recessive.
Table 5. Single-gene disorders associated with other congenital abnormalities.

AD = autosomal dominant; AR = autosomal recessive.
Ultrarare single gene disorders are likely to be recognized now that whole exome and, in the future, whole genome sequencing are offered much more routinely. It is likely that those babies that die soon after diagnosis may be identified with new gene mutations in previously unrecognized disorders.
There is also an increased prevalence of CAT in foetuses of mothers with diabetes.
Recommendations
All (newborn) children with CAT should be referred to a clinical geneticist for genetic screening of the patient and family members. All babies/foetuses should be tested by aCGH.
All parents of babies with an abnormality on aCGH should be offered either aCGH to see if they are a carrier of the same dele- tion/duplication or a karyotype if a chromosome translocation is suspected as the underlying cause (evidence level A).
If the result of the aCGH test is normal and there are no other concerns about the baby’s clinical condition, then at present no further testing can be recommended. If there has been a previous baby with a congenital heart disease (any type) or if there are any other congenital abnormalities, testing for single gene disorders by either a single gene test, such as CDH7 for CHARGE, or a clinical exome using either next generation sequencing or whole genome sequencing (evidence level B) should be recommended (Table 6). The identification of an underlying aetiology for CAT may be important in guiding patients regarding their present and, possibly, future reproductive options.
Table 6. Recommendations for genetic testing in patients with common arterial trunk.

aCGH = array comparative genomic hybridization.
a Level of evidence.
b Class of recommendation.
Morphology of common arterial trunk
Historical note and definition
CAT was first described in 1798 by Wilson; Reference Wilson27 the first pathomorphological autopsy diagnosis was established by Buchanan in 1862. Reference Buchanan28
CAT is defined as ‘A single arterial trunk that leaves the heart by way of a single arterial valve and that gives rise directly to the coronary, systemic and 1 or both pulmonary arteries’. Reference Crupi, Macartney and Anderson29 According to the segmental sequential analysis, there is a single outlet ventriculo-arterial connection (Fig. 1).
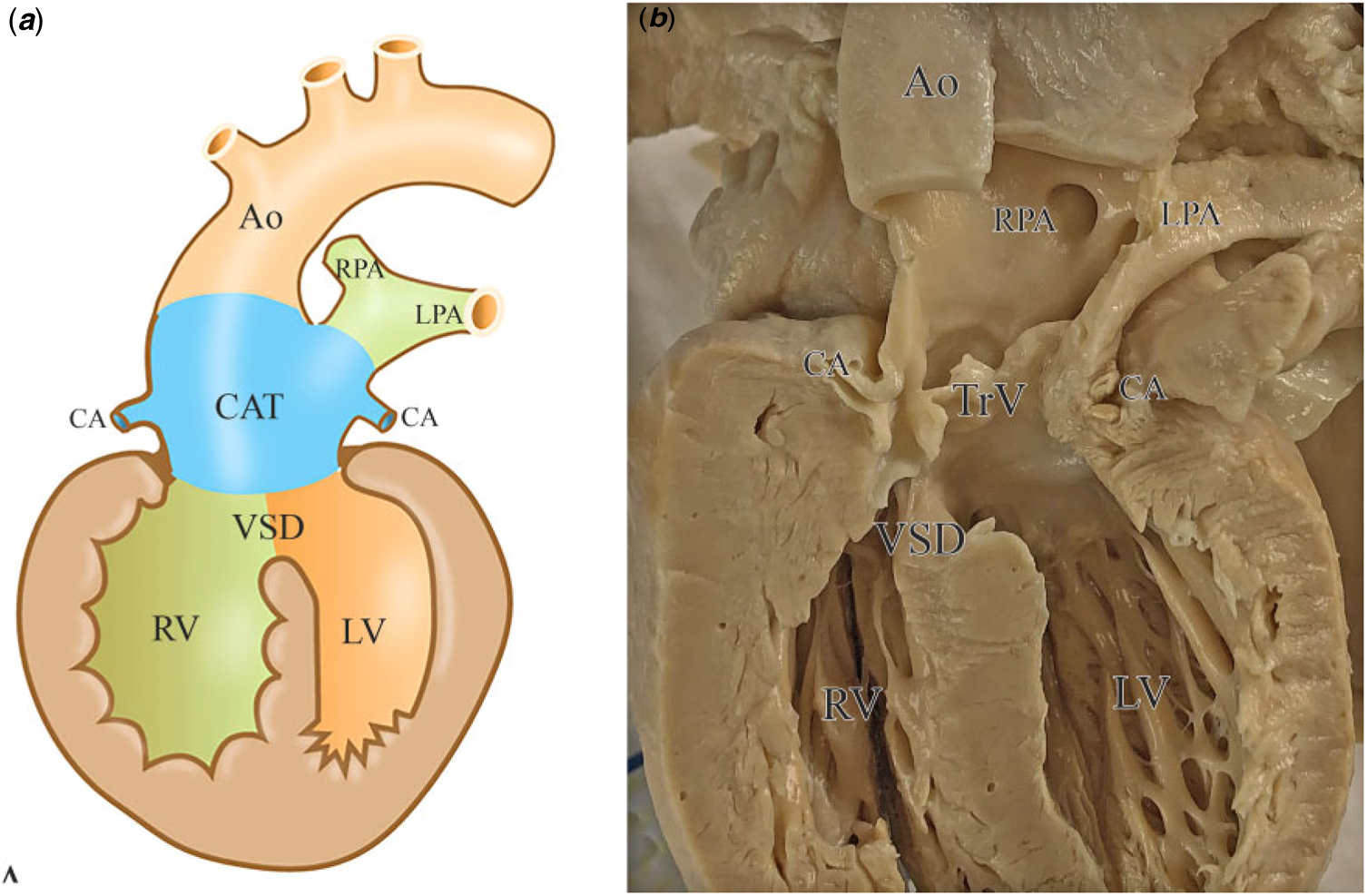
Figure 1. Morphology of the common arterial trunk. Schematic drawing (a) and morphological specimen ( b) of the CAT. There is a single-outlet ventriculo-arterial connection with deficient septation at the level of the outflow tract (location of the ventricular septal defect), the level of the arterial valve (truncal valve) and the level of the great arteries. The CAT gives access to the systemic, pulmonary and coronary circulation. Ao = aorta; CA = coronary artery; CAT = common arterial trunk; LPA = left pulmonary artery; LV = left ventricle; RPA = right pulmonary artery; RV = right ventricle: TrV = truncal valve; VSD = ventricular septal defect.
Initially, several controversies existed on the morphological diagnosis, mainly relating to whether or not cases with pulmonary atresia and an aortopulmonary window should be included. Because the latter malformations relate to a different anatomical spectrum and developmental background, both pulmonary atresia and aortopulmonary window (defect limited to the level of the intrapericardial trunks distal to the arterial valves Reference Anderson, Chaudhry and Mohun30 ), are not included in the diagnosis. Likewise, using the terms pseudotruncus, which refers to pulmonary or aortic atresia, and hemitruncus (anomalous origin of 1 PA from the ascending aorta), is discouraged. Reference Bartelings and Gittenberger-de Groot31,Reference Jacobs and Anderson32
Embryology
Morphogenetically, the main features of CAT can be attributed to a deficiency of the aortopulmonary septal complex, leading to the lack of aortopulmonary septation at three levels: the level of the great arteries, the valvular level and the level of the outflow tract. The latter results in the presence of a subarterial VSD. Reference Bartelings and Gittenberger-de Groot33 The deficiency of septation can vary, and the intrapericardial part of the arterial trunk can still be separated to some extent, particularly in the case of pulmonary arterial dominance. Reference Anderson, Webb, Brown, Lamers and Moorman34
The aortopulmonary septal complex is formed by a contiguous contribution of neural crest cells, which migrate to the heart from the crest of the neural tube during early development, and of second heart field cells, another population of cardiac progenitors that contribute to formation of the outflow tract. Reference Kirby, Gale and Stewart35–Reference Poelmann, Gittenberger-de Groot and Biermans37 During normal development, the initially unseparated vascular part of the outflow tract is referred to as the aortic sac. For adequate separation of the different levels of the embryonic outflow tract, development of the aortopulmonary septal complex and proper fusion of the outflow cushions are necessary. Reference Anderson, Mohun and Spicer38 Neural crest cells migrating to the heart become positioned not only at the level of the aortic sac, but also in the condensed mesenchyme of the septal outflow tract cushion at the orifice level as well as below this level. Reference Gittenberger-de Groot, Bartelings, Bogers, Boot and Poelmann39 Separation of the aortic sac thus extends to the arterial orifice level (i.e. putative arterial valve) and into the myocardial outflow tract, giving rise to the above-mentioned defects at three levels in case of impaired septation. The function of the neural crest cells depends on proper signalling with their environment. Deficiency of neural crest-related genes such as PAX3, retinoic acid, SEMA3C and LRP2, among others, causes CAT combined with aortic arch anomalies in animal models. Reference Conway, Henderson, Kirby, Anderson and Copp40–Reference Feiner, Webber and Brown43 Although deficiency of neural crest cells has been shown to cause CAT in many studies (reviewed in Reference Gittenberger-de Groot, Bartelings, Bogers, Boot and Poelmann39 ), as described above, these cells are not the only cell types that are crucial for proper formation of the aortopulmonary septal complex. Outflow tract septation is likely the result of a complex interaction between neural crest cells and cells derived from the second heart field. The transcription factor TBX1, which is related to the 22q 11.2 deletion syndrome (DiGeorge syndrome) in humans, is a critical regulator of second heart field development and is associated with multiple forms of outflow tract anomalies in animal models, including CAT. Reference Parisot, Mesbah, Théveniau-Ruissy and Kelly44
Classification of the common arterial trunk
Over the past decades, several CAT classification systems have been developed (Fig. 2). The first was proposed by Collet and Edwards in 1949 (Fig. 2a), Reference Collet and Edwards3 who initially defined four types of CAT. Types 1 to 3 referred to the mode by which the left and right PAs (RPAs) arise from the CAT. Type 4 of the Collet and Edwards classification is no longer considered a CAT subtype because it refers to cases with no pulmonary trunk and both PAs, with aortopulmonary collateral circulation. In addition, the classification does not consider aortic or pulmonary dominance caused by, for example, obstructive lesions in the aorta and non-confluent PAs. Van Praagh et al. Reference Van Praagh and Van Praagh4 therefore revised the classification system in 1965 (Fig. 2b) to include cases with a single PA supplying 1 lung, with arteries arising from the arterial duct/collateral arteries usually supplying the other lung (type A3), as well as cases with hypoplasia, coarctation, atresia or absence of the aortic isthmus, leaving the descending systemic circulation dependent on its blood supply from a large patent arterial duct (type A4). Cases with VSD were referred to as type A and those without, as type B. In 1976, Calder et al. Reference Calder, Van Praagh and Van Praagh5 provided an overview of clinical, haemodynamic and angiocardiographic findings, together with pathological data using this classification system. In this large study, all cases had a VSD. A minor simplification of the classification system was made by members of the Society of Thoracic Surgeons-Congenital Heart Surgery Database Committee and the EACTS in 2000: they combined type A1 and A2 (Fig. 2c). Reference Jacobs45
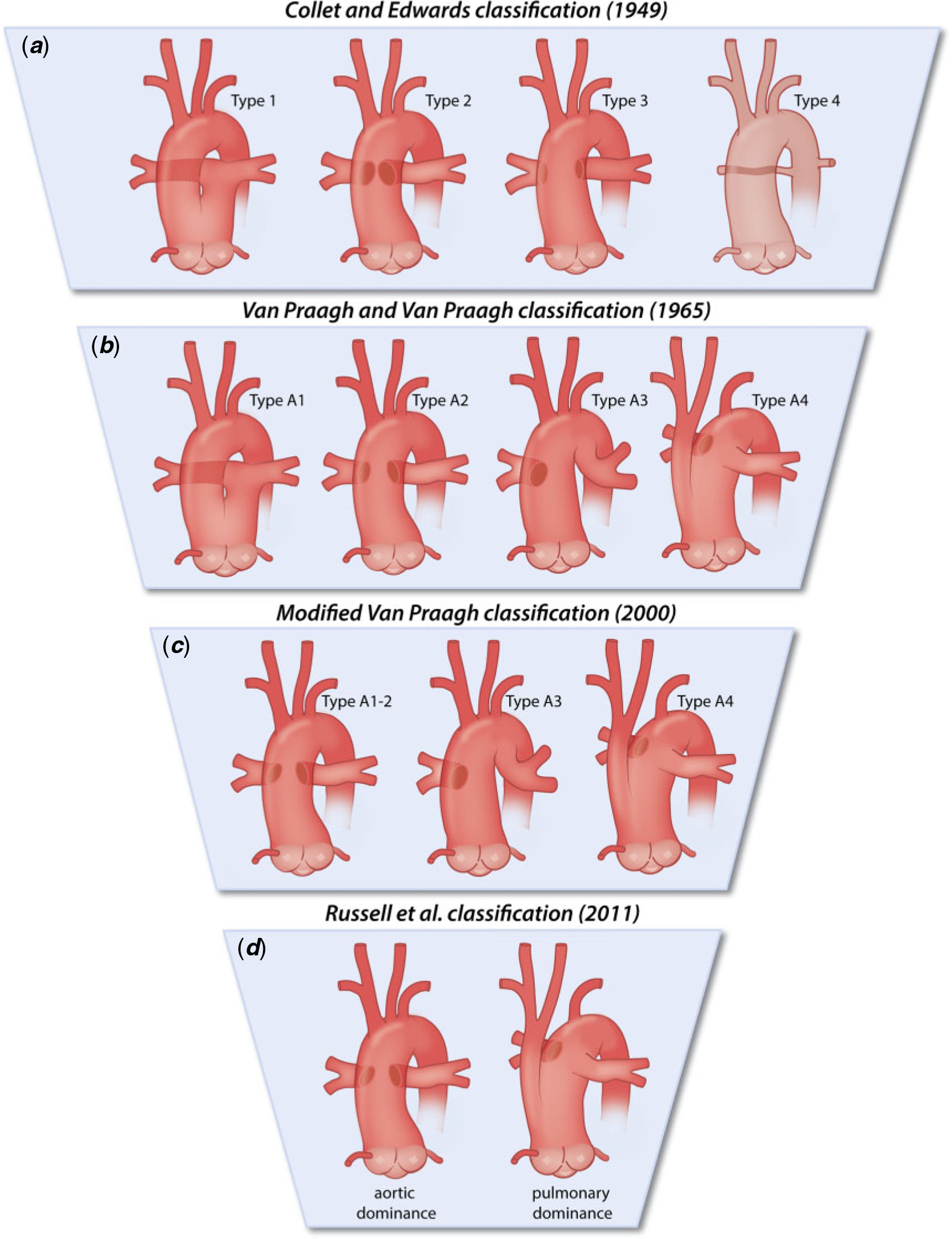
Figure 2. Historical overview of classification systems for common arterial trunk. ( a ) Collet and Edwards. Reference Collet and Edwards3 The left pulmonary artery (LPA) and right pulmonary artery (RPA) arise from the common arterial trunk (CAT) by interposition of a short pulmonary trunk (type 1), or the LPA and the RPA arise from the CAT with separate orifices, either with their orifices positioned close together (type 2) orwidely spaced (type 3). Type 4, in which both pulmonary arteries (PAs) and the pulmonarytrunk are absent and the pulmonary circulation is supplied by the aortopulmonary collateral circulation, is no longer considered the CAT. ( b ) Van Praagh and Van Praagh. Reference Van Praagh and Van Praagh4 The ‘A’ in these subtypes refers to cases with ventricular septal defect (VSD). Reference Calder, Van Praagh and Van Praagh5 Cases without VSD (type B) are not included in the drawing. Type A1, in which the LPA and RPA arise from the CAT by interposition of a short pulmonary trunk, conforms to Collet and Edwards type 1. In type A2, the LPA and RPA arise from the CAT with separate orifices, either close together or widely spaced (combination of types 2 and 3 of Collet and Edwards). Type A3, in which 1 PA is lacking, refers to cases with a single PA supplying 1 lung and arteries arising from the ductus or collateral arteries usually supplying the other lung. Type A4 includes hearts with aortic, coarctation, atresia or absence of the aortic isthmus. The descending systemic circulation is supplied by a large persistently patent arterial duct. ( c ) In the modified van Praagh classification, Reference Jacobs45 a simplification was proposed by combining types A1 and A2 of Van Praagh and Van Praagh (i.e. combining types 1, 2 and 3 of Collet and Edwards), thus giving rise to a type A1–2 where the LPA and RPA arise from the CAT by interposition of a short pulmonarytrunk or with separate orifices, either arising close together or widely spaced, without making this distinction. Types A3 and A4 conform to the original Van Praagh and Van Praagh classification. ( d ) Classification based on two subtypes: aortic versus pulmonary dominance. Reference Jacobs and Anderson32,Reference Russell, Jacobs and Anderson46 The aortic dominant type is characterized by adjacent or nearly adjacent PAs from the posterolateral aspect of the CAT, whereas in the pulmonary dominant type the distal systemic circulation is dependent on the patency of the arterial duct, as is encountered in cases of interruption of the aortic arch or coarctation. We endorse the latter classification as proposed by Russell et al. Reference Russell, Jacobs and Anderson46
aLevel of evidence.
In 2011, a simplified classification system with only two major subtypes was proposed, based on observations in a selection of autopsy hearts that (i) all hearts could be assigned to 1 of 2 groups based on the dominance of either the aortic or pulmonary circulation of the CAT; (ii) pulmonary dominance was found only when the aortic component of the trunk was hypoplastic and the descending aorta was supplied by the arterial duct; (iii) PAs arising from the lateral sides of the major pathway were observed only in the setting of pulmonary dominance; and (iv) only in cases with pulmonary dominance was the aortic component of the common trunk separate from the pulmonary component (Fig. 2d). Reference Jacobs and Anderson32,Reference Russell, Jacobs and Anderson46 These observations resulted in a classification system that divides CAT into two subtypes: cases with either aortic or pulmonary dominance. The authors argued that an advantage of this system, in addition to its simplification, is that it is congruent with embryology as well as with the clinical relevance of emphasizing the key morphological determinants (i.e. aortic or pulmonary dominance) of surgical outcome. A collateral advantage of this system is that the use of alphanumeric indications can be avoided by simply referring to aortic or pulmonary dominance, which is recommended for clinical discussions. The latter classification is endorsed by this task force. We acknowledge that this classification requires an additional description of anatomy, such as details on PAs.
Sequential segmental analysis
The majority of hearts with CAT have situs solitus (normal atrial arrangement) and concordant atrioventricular connections. Cases with right isomerism have been reported as have cases with a discordant atrioventricular connection. Reference Gumbiner, McManus and Latson47–Reference Smith and McKay49 The ventriculoarterial connection is a single outlet, with a variable amount of overriding of the TrV over the ventricular septum, including origin of the CAT exclusively from the right ventricle (RV). Reference Bogers, Bartelings and Bökenkamp50 Associated anomalies are common and should be described in detail (Table 7).
Table 7. Anatomical variations and associated cardiac and extracardiac anomalies in patients with common arterial trunk.

Data derived from multiple sources. Reference Van Praagh and Van Praagh4,Reference Calder, Van Praagh and Van Praagh5,Reference Bartelings and Gittenberger-de Groot31,Reference Bogers, Bartelings and Bökenkamp50–Reference Adachi, Ho, Bartelings, McCarthy, Seale and Uemura55
ALM = anterolateral muscle; ASD = atrial septal defect; AV = atrioventricular; AVSD = atrioventricular septal defect; MAPCAs = major aortopulmonary collateral arteries; PA = pulmonary artery; PAPVC = partial anomalous pulmonary venous connection; PLSCV = persistent left superior caval vein; PMM = posteromedial muscle; RCA = right coronary artery; RCx = ramus circumflex; RPA = right pulmonary artery; VSD = ventricular septal defect.
a Possibly secondary characteristic.
b Often caused by genetic/syndromic anomalies (see ‘Genetics of common arterial trunk’).
c Associated with 22qll.2 deletion syndrome.
d Associated with CHARGE syndrome.
Associated anomalies
Ventricular septal defect
VSD is present in a majority of cases. CAT with an intact ventricular septum is extremely rare and is not included in this document. The VSD is an outlet VSD, classically subarterial, whereby the truncal orifice can override the ventricular septum to various degrees (0–100%) and may originate exclusively from either ventricle. Reference Bogers, Bartelings and Bökenkamp50,Reference Adachi, Seale, Uemura, McCarthy, Kimberley and Ho51 The commonly used designation of the VSD as a malalignment VSD is incorrect in our view, because it implies a deviation of the outlet septum, which is deficient in CAT.
The VSD is generally large and non-restrictive; however, cases with extreme overriding (CAT arising from 1 ventricle) are associated with restrictive VSDs, which may affect the choice of surgical strategy. Reference Adachi, Seale, Uemura, McCarthy, Kimberley and Ho51
The VSD is situated between the limbs of the septomarginal trabeculation (TSM), and bordered superiorly by the TrV. The posteroinferior rim can either be muscular, comprising the continuation of the ventriculoinfundibular fold (VIF) and the TSM, or perimembranous. Its makeup is determined by the extent of development of the VIF, Reference Crupi, Macartney and Anderson29 which also determines whether continuity or discontinuity exists between the TrV and the mitral and tricuspid valves. Reference Crupi, Macartney and Anderson29 In most cases, fibrous continuity occurs between the mitral valve and the TrV. In the case of a well- developed VIF and TSM, the TrV is separated from the tricuspid valve. In the case of a hypoplastic VIF and TSM, there is fibrous continuity between the tricuspid valve and the TrV, in which case part of the posteroinferior rim of the VSD is fibrous; and thus, the outlet is a perimembranous VSD. This fibrous area contains the His bundle, which in these cases is not covered by muscle tissue and thus is considered more prone to damage during surgical repair.
Truncal semilunar valve
The number of valve leaflets in CAT can vary from 1 to 5; however, tricuspid, quadricuspid and bicuspid valve morphologies are most common. Reference Calder, Van Praagh and Van Praagh5,Reference Bogers, Bartelings and Bökenkamp50 Unicuspid and pentacuspid valves are extremely rare. One or more raphes can be present. Reference Suzuki, Ho, Anderson and Deanfield56,Reference Butto, Lucas and Edwards57 The TrV is often dysplastic, which affects function. The valve can have variable degrees over overriding and is most often dextroposed.
Pulmonary arteries
The PAs can arise separately from the CAT or via a short common trunk. The origin is most commonly from the left posterolateral part of the trunk. In the case of separate ostia, the left PA (LPA) is generally in a higher position than the RPA. Ostial stenosis has been described and can restrict pulmonary blood flow. Reference Rossiter, Silverman and Shumway58 Pulmonary arterial branch obstruction may occur but is rare. Pulmonary arterial hypoplasia or atresia, as well as the unilateral absence of 1 PA, distal ductal origin of 1 PA or origin of a PA from an aortopulmonary collateral have all been described.
Coronary artery anatomy
A myriad of coronary arterial variations can be observed. Reference Suzuki, Ho, Anderson and Deanfield56 Coronary anomalies were observed in 64% in 1 series. Reference Bogers, Bartelings and Bökenkamp50 The left coronary orifice is usually positioned in the posterior part of the common trunk, and the right orifice, in the right anterior and lateral parts. Reference Bogers, Bartelings and Bökenkamp50,Reference Suzuki, Ho, Anderson and Deanfield56 Variations in ostial position/distribution include single coronary arteries (uncommon), double coronary orifices, position of ostia near the TrV commissure, ostium stenosis/pinpoint orifices and an intramural proximal course of coronary arteries. Reference Bogers, Bartelings and Bökenkamp50,Reference Suzuki, Ho, Anderson and Deanfield56,Reference Oddens, Bogers, Witsenburg and Bartelings59
High take-off leading to acute angulation may be related to aortic dimensions, as was also described for other forms of congenital heart disease. Reference Veltman, Beeres and Kalkman60 Large infundibular branches of the right coronary artery may pose a risk for right ventriculotomy. Reference Anderson, McGoon and Lie61 Right circumflex branching from the right coronary artery has been described and poses a risk for obstruction during pulmonary banding. Reference Daskalopoulos, Edwards, Driscoll, Schaff and Danielson62 Coronary arteries may be positioned close to PAs, which poses a risk of coronary arterial damage during excision of the Pas. Reference Bogers, Bartelings and Bökenkamp50,Reference Adachi, Uemura, McCarthy, Seale and Ho52,Reference Oddens, Bogers, Witsenburg and Bartelings59
Left dominant coronary arterial distribution has been reported in a higher incidence than in the general population.
Truncal root, aortic arch and arterial duct
Although described by some authors to be present in CAT, Reference Van Praagh and Van Praagh4,Reference Calder, Van Praagh and Van Praagh5 the arterial duct is usually absent in cases with an unobstructed aortic arch. In the case of a widely open duct, the transverse arch is in most cases either interrupted or hypoplastic. IAA or aortic coarctation is present in 15–20% of patients; in these cases, the blood supply to the distal aorta is via an open arterial duct. The interruption in most cases affects the aortic B segment (between the left carotid and the subclavian artery). A right-sided aortic arch is present in approximately one-third of patients; mirror image branching is usual. An aberrant subclavian artery occurs in 4–10% of cases. Reference Freedom, Yoo, Freedom, Yoo, Mikailian and Williams53 A double aortic arch has been described but is rare. Reference Collet and Edwards3,Reference Angelini and Leachman63
The size of the (neo)aortic root is increased, and further dilation is often observed during longer follow-up but is rarely associated with dissection. Reference Carlo, McKenzie and Slesnick64,Reference Gutierrez, Binotto, Aiello and Mansur65 Whether the dilation is secondary to disturbed haemodynamics, primarily caused by a developmental anomaly of the vascular wall, or a combination of both, is at present unclear. Aortic arch anomalies are more prevalent in cases with the 22q11.2 deletion syndrome. Reference Momma, Matsuoka and Takao66
The left ventricle in common arterial trunk/ventricular abnormalities
Prominent muscle bundles, such as a prominent anterolateral muscle bundle, anteroseptal twist and posteromedial muscle, are commonly observed in CAT and may compromise the function of the mitral valve. Association with tricuspid atresia/RV hypoplasia and (in rare cases) mitral atresia/left ventricular hypoplasia, has been described. Reference Freedom, Yoo, Freedom, Yoo, Mikailian and Williams53
Other associated anomalies
Several other cardiac and noncardiac malformations have been associated with CAT (summarized in Table 7). Non-cardiac anomalies are usually related to genetic syndromes, mainly the 22q11.2 deletion syndrome, which may adversely affect prognosis.
Prenatal diagnosis and management
First trimester ultrasonography
Multidisciplinary cooperation in the field of foetal cardiology is developing. Using modern ultrasound equipment, it is now possible to diagnose congenital heart defects from the first trimester of pregnancy. Reference Sairam and Carvalho67 Obstetricians and trained sonographers are on the first diagnostic line. First trimester ultrasonography is recommended in the majority of European countries between 11.0 and 13.6 weeks of gestation, when the crown-to-rump length is between 45 mm and 85 mm. The increased nuchal translucency, Reference Sairam and Carvalho67,Reference Carvalho68 tricuspid insufficiency, reverse atrial contraction wave, but more precisely—an increased ductus venosus pulsatility index Reference Jicinska, Vlasin and Jicinsky69 —can be signs of foetal cardiac problems. High-frequency ultrasound or the spatiotemporal image correlation method can help in more precise cardiac diagnosis during the first trimester.
Second trimester foetal echocardiography
The first series of foetal CAT was described in 2001. Reference Duke, Sharland, Jones and Simpson70 Of 17 pregnancies, 4 were terminated, and 12 children were born alive. Of the live births, 7 were operated on and 5 survived. A series from 2003 described 23 foetuses with CAT. Reference Volpe, Paladini and Marasini8 Two foetuses died in utero, 8 pregnancies were terminated and 13 children were born alive. Of the live births, 3 died preoperatively, 5 died postoperatively and 5 children survived after the operation. TrV dysfunction was reported as the most severe sign of an adverse outcome, because the majority of those foetuses died in utero or before surgery.
The majority of cases of CAT in foetuses are diagnosed in the mid-trimester or later. This lesion is easy to miss during routine foetal ultrasound screening because the 4-chamber view is close to normal. The first sign of abnormality is the increased cardiac axis, usually 70° or more and usually with an intact ventricular septum in a typical 4-chamber view. The next step is to tilt the transducer towards the 5-chamber view to visualize the ventricular outflow tracts. The foetal parasternal long-axis view (starting from the lateral 4-chamber view) is the best for visualizing the VSD with 1 large vessel that overrides the interventricular septum. Such an image is characteristic for CAT or pulmonary atresia with VSD. Careful evaluation of the arterial valve is mandatory.
The TrV in CAT is always bigger than that of the aortic valve in tetralogy of Fallot or pulmonary atresia with VSD. Leaflets are described as dysplastic if they are thickened or nodular, and they are easily visualized during the whole cardiac cycle. The number of leaflets can be seen on good quality images. Coronary arteries can rarely be evaluated during foetal echocardiography. Colour Doppler is helpful in assessing TrV function. If the valve is dysplastic, turbulent forward flow and a regurgitant jet can be detected. Maximal velocity through the dysplastic, stenotic TrV is increased. Both stenosis and insufficiency of the TrV can deteriorate during pregnancy. If the heart is enlarged and there are signs of foetal congestive heart failure evaluated by the cardiovascular profile score, Reference Duke, Sharland, Jones and Simpson70 transplacental digoxin can be administered to improve the foetal condition and prolong pregnancy. Reference Huhta71
The next step is to evaluate the anatomy of the PA branches. The most common form is that in which the main PA arises from the trunk just over the TrV and divides into two usually normalsized branches. The right and LPA may also arise from the ascending part of the trunk, close to one another or more distant from one another. Finally, there may be a common trunk from which right and left pulmonary branches arise and the aortic arch is interrupted.
In cases of CAT, the PAs and aortic arch anatomy should be evaluated from several different, commonly non-standard views, which is sometimes extremely difficult. It is important to establish the distance between the PAs and aortic arch morphology. If the arch is interrupted, the patient has a ductal-dependent lesion, and intravenous prostaglandin must be administered after delivery.
From a mediastinal view it is possible to distinguish between the right and left aortic arch. In this view the thymus should be evaluated. In a foetus, the thymus is a large organ, the diameter of which in millimetres is about the same as the gestational age. The other method of thymus evaluation was described by Karl et al., Reference Karl, Heling, Sarut Lopez, Thiel and Chaoui72 who measured the thymic-thoracic ratio (TT ratio), which is measured in the 3-vessel and tracheal views (3VT). The vessels should be situated in the middle of the mediastinum. If they are seen close to the anterior mediastinal wall and the thymus is not seen, 22q11.2 microdeletion is likely. Colour and power Doppler should be used to look for any kind of vascular rings, which may coexist with CAT, like an aberrant right or left subclavian artery. PA branches and the presence (in cases of IAA) or the absence of the arterial duct can also be evaluated in the mediastinal view.
Extracardiac anomalies are found in about 40% of foetuses with CAT. A detailed evaluation of the anatomy of all foetal organs is necessary, because the presence of other defects worsens the postnatal prognosis.
Differential diagnosis
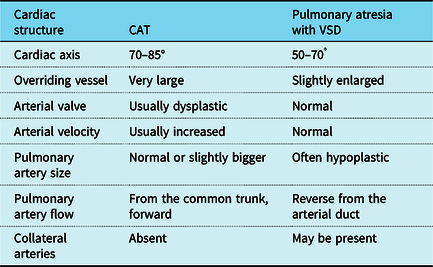
The most challenging diagnosis is to distinguish between CAT and tetralogy of Fallot with pulmonary atresia. Both lesions have similar appearances in prenatal scanning (Table 8). The heart is levorotated, and a large artery overrides the septum with a large outlet VSD. RVOT and PA branches are difficult to visualize. The major differences include the following: the morphology of the arterial valve is dysplastic in the majority of cases with CAT and normal in cases of pulmonary atresia with VSD; a more proximal branching of the PAs is seen in CAT; the size of the pulmonary branches is normal or even enlarged in CAT, but hypoplastic or within normal limits in pulmonary atresia with VSD; and finally, main aortopulmonary collaterals might be present in cases with pulmonary atresia with VSD but are not visualized in CAT. Reference Traisrisilp, Tongprasert, Srisupundit, Luewan, Sukpan and Tongsong73
Table 8. Differentiation between common arterial trunk and pulmonary atresia with ventricular septal defect in foetal echocardiography.
CAT = common arterial trunk; VSD = ventricular septal defect.
Counselling
Counselling is an extremely important part of complete foetal cardiac evaluation. General rules for prenatal counselling should be followed. Initially, only the most important information should be provided in simple, clear terms. Parents must have the opportunity to ask questions, to express grief and to have time alone if desired. Reference Allan, Dangel and Fesslova74
Because 35% of foetuses with CAT have a 22q11.2 microdeletion Reference Peyvandi, Lupo and Garbarini75 and because it is possible that other genetic problems may occur, if CAT is diagnosed or strongly suspected in the early period of pregnancy, genetic testing should be discussed with parents.
The morphology of CAT in foetuses differs from that in infants diagnosed postnatally. More commonly, a dysplastic TrV, leading to foetal and neonatal congestive heart failure, is seen. TrV morphology, apart from the genetic findings, is crucial for prenatal counselling because TrV dysplasia and insufficiency carry a high-risk of intrauterine death and a more complicated course postnatally.
The type of arterial trunk is important for planning a surgical procedure. However, in a large surgical series, the morphology of CAT, apart from that in cases with dysplastic TrV, was not important in determining the surgical result. Reference Naimo, Fricke and Yong76 Outcomes may vary between institutions; a general overview is given in the final chapter on outcomes. Although these data are important for overall knowledge about treatment results, during parental counselling, it is important to discuss outcomes on the basis of the results of the institution in which their child will be treated.
All aforementioned problems must be discussed with the parents who, once in possession of all the facts and according to the national laws of their country, can choose to either continue with or terminate the pregnancy. Termination rates vary among countries. The specialist in foetal cardiology must be prepared to discuss with parents both short- and long-term prognoses. In cases of late foetal diagnosis of CAT with a severely dysplastic TrV, perinatal palliative care may be discussed, with comprehensive medical and psychological support provided for parents.
Preoperative management
Delivery
Delivery should be in a tertiary centre with paediatric cardiologists and cardiac surgeons available. Neonatal long-distance transport should be avoided when possible. Reference Hellström-Westas, Hanseus, Jögi, Lundstrom and Svenningsen77 Following these precautions guarantees direct post-partum echocardiographic evaluation and stabilization in a neonatal or paediatric intensive care setting whenever necessary. CAT is an unstable cardiac anomaly, and heart failure may present early when pulmonary vascular resistance drops in the first weeks after birth. Especially when CAT is associated with coexisting anomalies, such as interrupted arch or TrV regurgitation or obstruction, it is important to have all necessary tertiary care at hand.
Preterm delivery should be avoided because it has been reported that birth during the early term period of 37–38 weeks’ gestation is associated with worse outcomes of neonatal cardiac surgery. Reference Costello, Pasquali and Jacobs78 Exceptions may be made when foetal distress exists, e.g. due to severe TrV insufficiency. In these circumstances, earlier delivery and, if needed, delivery by planned caesarean delivery may sometimes be indicated to avoid foetal demise.
Postnatal and preoperative diagnosis
Clinical findings
Prenatally undiagnosed patients typically present in the neonatal period or early infancy with signs of increasing cardiac failure and mild central cyanosis. These signs include tachypnoea, hepatomegaly and feeding difficulties resulting in failure to thrive. Those patients who have predominant, more obvious cyanosis have persistently increased pulmonary vascular resistance, PA stenosis or PA hypoplasia. Reference Shamszad, Moore, Ghanayem and Cooper79
Symptoms can be exacerbated by TrV abnormalities. Reference Colon, Anderson, Weinberg, Mussatto, Bove and Friedman80 Moderate-to-severe TrV insufficiency and the rarer condition of severe TrV stenosis can lead to early signs of congestive heart failure up to cardiogenic shock. Reference Shamszad, Moore, Ghanayem and Cooper79,Reference Colon, Anderson, Weinberg, Mussatto, Bove and Friedman80 Patients with IAA have a duct-dependent systemic circulation, and closure of the ductus arteriosus leads to progressive cardiovascular collapse.
Heart murmurs can be heard in more than half of the patients in the first week of life. Reference Calder, Van Praagh and Van Praagh5 Early diastolic murmurs can indicate TrV insufficiency. The heart sounds can be split or single, and explanations for this can be asynchronous closure of the valvar leaflets or production of a duplicate sound by vibrations within the arterial trunk. Reference Penny, Anderson, Andersen, Baker, Penny, Redington, Rigby and Wernovski81 Many patients also present with an ejection click. Reference Calder, Van Praagh and Van Praagh5 The clinical examination should include assessment of non-cardiac anomalies.
Chest X-ray and electrocardiogram
The chest X-ray demonstrates cardiomegaly and increased pulmonary vascularity in the majority of patients. Reference Calder, Van Praagh and Van Praagh5,Reference Penny, Anderson, Andersen, Baker, Penny, Redington, Rigby and Wernovski81,Reference Yoo, Kim and Bae82 Right aortic arch occurs in 2530% of patients. Reference Freedom, Yoo, Freedom, Yoo, Mikailian and Williams53,Reference Penny, Anderson, Andersen, Baker, Penny, Redington, Rigby and Wernovski81 The heart is commonly oval in shape due to the absence or hypoplasia of the RVOT. Reference Calder, Van Praagh and Van Praagh5,Reference Yoo, Kim and Bae82 Decreased pulmonary vascularity can indicate underdevelopment of the pulmonary trunk and branch PAs (Table 9). Reference Calder, Van Praagh and Van Praagh5,Reference Yoo, Kim and Bae82
Table 9. Typical neonatal chest X-ray and electrocardio graphic findings. Reference Calder, Van Praagh and Van Praagh5,Reference Penny, Anderson, Andersen, Baker, Penny, Redington, Rigby and Wernovski81,Reference Yoo, Kim and Bae82

ECG = electrocardiogram.
The electrocardiogram (ECG) features are non-specific. The frontal QRS axis is variable but is reported in most cases to be more than +60°. Biventricular hypertrophy is frequently seen whereas isolated right or left ventricular hypertrophy is less common (Table 9). Reference Calder, Van Praagh and Van Praagh5,Reference Penny, Anderson, Andersen, Baker, Penny, Redington, Rigby and Wernovski81
Preoperative transthoracic echocardiography
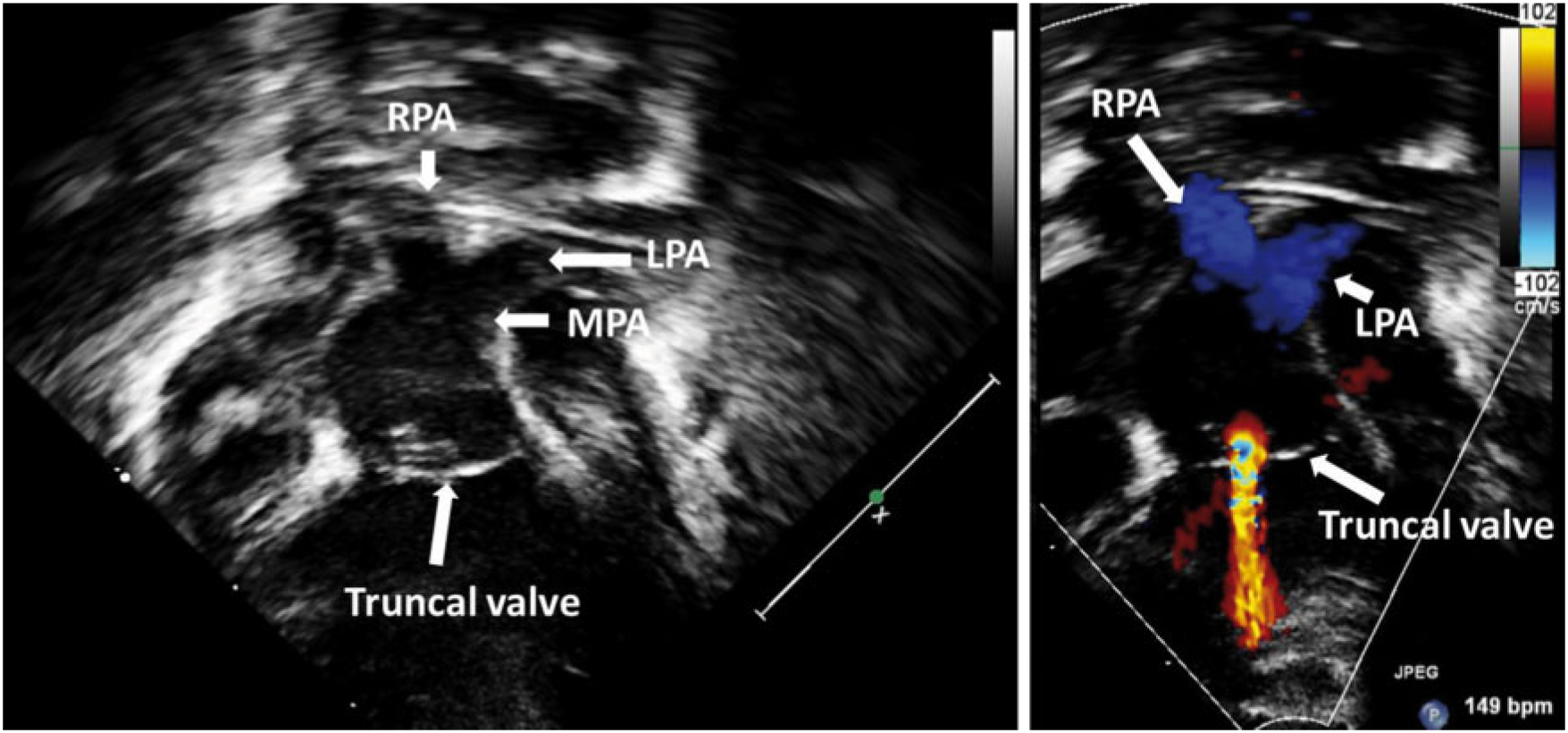
Transthoracic echocardiography (TTE) is the imaging method of choice for the diagnosis and preoperative assessment of CAT (Table 10). TTE can usually provide all of the diagnostic information that is necessary for surgical and clinical decision-making. The crucial findings are a single arterial trunk overriding the ventricular septum and a large-outlet VSD. Reference Nguyen, John, Nardell, Gonzalez, Timofeev and Marx83 These features are seen clearly in the parasternal long-axis view (Fig. 3). Reference Yoo, Kim and Bae82,Reference Nguyen, John, Nardell, Gonzalez, Timofeev and Marx83 The goals of preoperative TTE include, in particular, description of the VSD and any additional VSDs, morphological and functional evaluation of the TrV, assessment of the PAs (Fig. 4) and aortic arch (to exclude an IAA) and assessment of ventricular size and function. Reference Nguyen, John, Nardell, Gonzalez, Timofeev and Marx83 In addition, coronary artery anatomy and any pulmonary and systemic venous anomalies should be reported. The sequential segmental approach should be followed. Suggested echocardiographic reporting elements are illustrated in Table 11.
Table 10. Recommendations for postnatal and preoperative diagnosis.

CAT = common arterial trunk; CMRI = cardiovascular magnetic resonance imaging; CT = computed tomography; TTE = transthoracic echocardiography.
a Level of evidence.
b Class of recommendation.
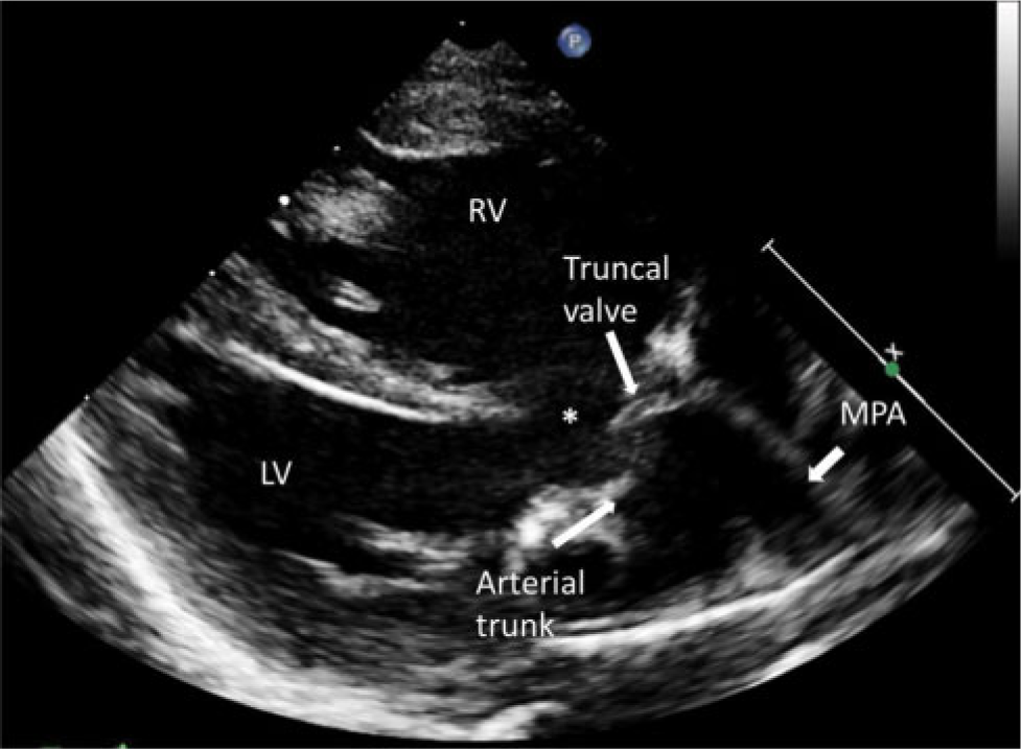
Figure 3. Parasternal long-axis view of a common arterial trunk. The arterial trunk overrides the ventricular septum and the large outlet ventricular septal defect (*). LV = left ventricle; MPA = main pulmonary artery; RV = right ventricle.

Figure 4. Two-dimensional transthoracic echocardiographs with colour Doppler showing the truncal valve and the pulmonary arteries in a neonate with a common arterial trunk. There is mild-to-moderate truncal valve regurgitation. LPA = left pulmonary artery; MPA = main pulmonary artery; RPA = right pulmonary artery.
Table 11. Proposed standard preoperative transthoracic echocardiographic views and reporting elements. Reference Yoo, Kim and Bae82,Reference Nguyen, John, Nardell, Gonzalez, Timofeev and Marx83

AV = atrioventricular; IAA = interrupted aortic arch; Pas = pulmonary arteries; SVC = superior vena cava; TTE = transthoracic echocardiography.
Three-dimensional echocardiography should be regarded as a complementary technique that can provide additional information about the morphology and function of the TrV (Table 10). Reference Nguyen, John, Nardell, Gonzalez, Timofeev and Marx83,Reference Simpson, Lopez and Acar84
Cardiovascular computed tomography
Echocardiography is the first-line and standard imaging modality for preoperative assessment. Reference Prakash, Powell and Geva85 In the majority of cases, echocardiography is sufficient. Cardiovascular computed tomography (CT) and cardiovascular magnetic resonance imaging (CMRI) are complementary techniques only when further information is needed (Table 10). Reference Han, Rigsby and Hlavacek86,Reference Fogel and Crawford87 Cardiovascular CT allows detailed assessment of coronary arteries, PAs and aortopulmonary collaterals and is well suited to visualize aortic arch anomalies, including aortic coarctation and IAA. Reference Han, Rigsby and Hlavacek86,Reference Hong, Kim, Lee, Lee, Kim and Lee88,Reference Sharma, Priya and Jagia89
Cardiac catheterization and angiography
Diagnostic cardiac catheterization and angiography are rarely needed because echocardiographic and cross-sectional imaging techniques are often sufficient to correctly describe the anatomical details (Table 10). Reference Prakash, Powell and Geva85 In cases with a complex anatomy or an abnormal coronary artery pattern (e.g. only 1 branch PA arises from the CAT, blood supply for the other lung is provided by a ductus arteriosus or aortopulmonary collateral), cardiac catheterization may clarify the anatomical situation. Cardiac catheterization, however, is important in patients with a late presentation to assess pulmonary vascular resistance and to test pulmonary vascular reactivity. Reference Stapleton, Wilmot and Suh90,Reference Hosseinpour and Shinebourne91
Other investigations
The 22q11.2 deletion has been associated with non-cardiac features, which might be important for the perioperative management of patients, such as palatal anomalies, hypocalcaemia and immune deficiency. Reference Peyvandi, Lupo and Garbarini75,Reference Kobrynski and Sullivan92 Thus, genetic testing is recommended in the neonatal period prior to surgical intervention.
Children with the 22q11.2 deletion had an increased number of infections in the postoperative period after cardiac surgery. Reference McDonald, Dodgen and Goyal93 Although only rarely do patients with the 22q11.2 deletion have severe immunodeficiency (complete absence of T cells), Reference Kobrynski and Sullivan92 irradiated blood products can be recommended for children with this condition. Reference Shamszad, Moore, Ghanayem and Cooper79 Patients with the 22q11.2 deletion are also at risk for postoperative hypocalcaemia, which can occur unpredictably and has been associated with significant complications and mortality. Reference Jatana, Gillis, Webster and Ades94,Reference Shen, Gu and Wang95 Consequently, serum ionized calcium should be measured pre- and postoperatively. Reference Jatana, Gillis, Webster and Ades94,Reference Shen, Gu and Wang95
Preoperative stabilization
Newborns with known CAT should not be discharged from the hospital before they are operated on. Discharge from the nursery or hospital with an undiagnosed CAT increases mortality. Reference Mastropietro, Amula and Sassalos96 Reparative surgery should be scheduled during the neonatal period if the condition of the patient permits. Reference Naimo, Fricke and Yong76,Reference Mastropietro, Amula and Sassalos96–Reference Jacobs, Mayer and Mavroudis99 TrV insufficiency or stenosis may lead to rapid haemodynamic deterioration and can be a reason for an early operation. Aortic arch interruption indicates the need for prostaglandin to secure ductal patency and may be another reason to perform the operation at an early stage.
Necrotizing enterocolitis is known to occur in term neonates with CAT; careful monitoring of feeding intolerance and abdominal distention is warranted. Reference McElhinney, Hedrick and Bush100 Right aortic arch occurs in 25–30% of patients with CAT (more frequently when the 22q11.2 deletion is present) and may lead to tracheal compression. Reference Freedom, Yoo, Freedom, Yoo, Mikailian and Williams53,Reference Penny, Anderson, Andersen, Baker, Penny, Redington, Rigby and Wernovski81 When respiratory symptoms are present, a CT scan and/or bronchoscopy should be performed to search for coexisting tracheobronchial and vascular pathologies. Reference McElhinney, McDonald-McGinn, Zackai and Goldmuntz101 Coronary artery anomalies are associated with CAT, so a preoperative CT scan should be pursued when echocardiography fails to provide accurate coronary artery anatomical details. The 22q11.2 deletion is present in 35% of all patients with CAT and should preferably be diagnosed or excluded before the operation. Reference Peyvandi, Lupo and Garbarini75 Blood products can be irradiated in patients with the 22q11.2 deletion, Reference Shamszad, Moore, Ghanayem and Cooper79,Reference Parshuram, Doyle, Lau and Shemie102 and calcium levels must be carefully monitored to prevent hypocalcaemia. Reference Shamszad, Moore, Ghanayem and Cooper79,Reference Shen, Gu and Wang95,Reference Ryan, Goodship and Wilson103
Bilateral PA banding may be used to stabilize a patient when a reparative procedure is (relatively) contraindicated: very low body weight (<1.5 kg), necrotizing enterocolitis or brain damage. TrV insufficiency/stenosis requiring valve replacement may form another indication for bilateral PA banding and delaying definitive surgery. Reference Yoshitake, Kaneko, Yakuwa and Achiwa104–Reference Hoashi, Kagisaki, Oda and Ichikawa106 Recovery from shock and weight gain are also indications for a staged repair.
When heart failure is present, stabilization may be obtained by diuretic therapy, mechanical ventilation and intravenous administration of inotropic medication, such as phosphodiesterase inhibitors and noradrenaline. Reference Hoffman, Wernovsky and Atz107 Nitric oxide should not be used in neonates and young infants with CAT because it may lead to an increase of pulmonary flow and haemodynamic instability due to a left-to-right shunt. Reference Parikh, Eisses, Latham, Joffe and Ross108 When mechanical ventilation is necessary to stabilize the patient, surgery should be planned urgently.
Surgery for common arterial trunk
Decision-making and timing
All cases should be discussed by the multidisciplinary team whenever possible, unless the situation is considered an emergency. High-risk cases benefit particularly from a more inclusive discussion, which should include input from intensive care and anaesthesia specialists. Severe truncal regurgitation (TrR) is a risk factor for outcome but is not a contraindication for surgery. Families should be clearly counselled about the higher risks and poorer outcomes associated with greater than moderate TrR and with IAA (Table 12).
Table 12. Recommendations for quoted operative risk (30-day mortality risk) associated with different common arterial trunk subtypes.

ECMO = extracorporeal membrane oxygenation; TrR = truncal regurgitation.
a Level of evidence.
b Class of recommendation.
There is good evidence that complete repair can be offered in all cases, accepting the higher risk associated with the more complex subtypes. Nevertheless, it is important that other risk factors be considered (Table 13) as well as any social issues that may impact the family’s capability to care for the child. In severe situations, it may be reasonable to offer comfort care as an option in cases in which the team feels that the operative risks are too high.
Table 13. Additional risk factors associated with surgical outcomes in common arterial trunk.

TrR = truncal regurgitation.
a Level of evidence.
b Class of recommendation.
Repair should be performed during the neonatal period. Reference Mastropietro, Amula and Sassalos96 Cases with associated IAA may require earlier surgery if they are clinically unstable. There is no evidence that an operation in the first few days of life carries any benefit over planned repair at 714 days. Reference Naimo, Fricke and Yong76,Reference Luo, Zheng and Zhu97,Reference Jacobs, Mayer and Mavroudis99,Reference Brown, Ruzmetov, Okada, Vijay and Turrentine109–Reference Chen, Gao and Hua119,Reference Hanley, Heinemann and Jonas134
In cases of premature birth, evidence shows that delaying surgery until gestational maturity has been achieved may reduce the risk of neurological morbidity secondary to cardiopulmonary bypass. This outcome has been shown in wider studies of neonatal surgery that included cases of CAT. The benefit is determined by extrapolation rather than specifically proven in a subset of patients with CAT. Reference Costello, Pasquali and Jacobs78
In patients who present later, in whom repair is undertaken when the child is older, there is a risk of reactive pulmonary vasculature or pulmonary vascular obstructive disease. Repair beyond the neonatal period has been achieved with good results, but infants who survive to this age are generally self-selected as the less complex variants. Older patients should undergo full haemodynamic assessment and calculation of pulmonary vascular resistance. Successful repair can be achieved with a resistance of up to 6–8 Wood units, or even as high as 9 Wood units as long as there is evidence of clear reversibility with oxygen therapy. Reference Arslan, Ugurlucan and Yildiz135
Use of bilateral pulmonary artery banding
Bilateral banding as a palliative procedure was attempted in the 1970s and 1980s as a means to delay definitive repair. Results were universally disappointing with an early mortality of >50%; the strategy was abandoned. There is no evidence to suggest that bilateral PA banding has any place in the regular management of CAT.
Nevertheless, in extreme cases where the risk of cardiopulmonary bypass is prohibitive (such as in the presence of an intracranial bleed or active necrotizing enterocolitis), the application of bilateral bands could be considered as a salvage procedure to balance the circulation in cases with uncontrolled congestive cardiac failure; this situation has been reported. Reference Yoshitake, Kaneko, Yakuwa and Achiwa104–Reference Hoashi, Kagisaki, Oda and Ichikawa106 There is insufficient evidence to determine whether this approach leads to a better outcome in these extreme cases, but application of bilateral banding techniques as proposed in the hybrid management of hypoplastic left heart syndrome would be the only reference. Reference Akintuerk, Michel-Behnke and Valeske136 The diastolic run-off in the setting of CAT would be a greater concern than in hypoplastic left heart syndrome with the increased risk of coronary steal. Regular monitoring of the ECG for signs of ischaemia may be helpful.
Surgical technique
Intraoperative parameters and bypass management
After sternotomy and opening the pericardium, snaring the RPA may help to achieve haemodynamic stabilization. Once cardiopulmonary bypass has started, both PAs must be snared to prevent massive pulmonary flow. Different cardiopulmonary bypass strategies have been described with limited evidence to support 1 strategy over another, and standard neonatal bypass management is entirely suitable for CAT repair, utilizing full-flow bypass with moderate hypothermia. There is no evidence to support the routine use of deep hypothermic circulatory arrest except in the setting of IAA, where it is used in all reported series. The use of regional cerebral perfusion during arch repair is well described but with no evidence to suggest any specific neurological benefit over deep hypothermic circulatory arrest in patients with CAT. Different myocardial protection strategies have also been described but antegrade administration is favoured by all published series. No specific benefit of 1 cardioplegia solution over another has been specifically shown in CAT nor of crystalloid versus cold blood-based preparations. The recommendation is that surgeons should use the neonatal cardioplegia strategy that they are familiar with. In cases of >moderate TrR, direct coronary ostial administration of cardioplegia may be necessary to achieve optimum delivery; however, care needs to be taken to identify the coronary ostia, which may be close to the valve commissures or in unusually high locations. Abnormal coronary patterns are frequent in CAT (Table 7).
There is no evidence to favour the use of specific inotropes in operative management, but it is recommended from extrapolation from other neonatal cardiac procedures that the use of phosphodiesterase inhibitors, such as milrinone, improve outcome. Reference Hoffman, Wernovsky and Atz107
Delayed sternal closure has been used variably in most studies but there is no evidence that delayed closure reduces morbidity or mortality. Evidence does show that delayed sternal closure is safe and effective. The use of PA pressure monitoring lines postoperatively has been described in several series, but there is no evidence to prove any clinical benefit from their use. The use of PA lines is safe, and proponents have cited their use in patients felt to be at higher risk of pulmonary hypertensive crisis (such as older age at repair).
Pulmonary artery separation
The PAs should be detached from the main trunk as a single button. This procedure can be performed by excision directly from the trunk or by first transecting the trunk above the PA take-off and then excising them: both techniques have been used with equal success. Care should be taken to identify the position of the coronary ostia before undertaking the excision and to beware of high origins of the coronary arteries close to the PA origins.
The defect in the trunk can be either closed directly or with patch repair. There is no evidence that 1 technique is superior to the other. Most series report a mixture of techniques based on surgeon preference.
Ventricular septal defect closure
The defect is most commonly a muscular outlet VSD but canalso be perimembranous VSD. Closure is performed through the ventriculotomy, but in cases of perimembranous extension, some sutures can be placed via the right atrium if preferred to gain access to the inferior border of the defect. There is no evidence to favour any particular patch material. Surgeons use their material of choice for neonatal VSD closure, most commonly xenograft pericardium, glutaraldehyde fixed autologous pericardium, thin-walled Gore-Tex® (W. L. Gore & Associates, Flagstaff, AZ, USA) or Dacron. The incidence of postoperative heart block is expected to be 1–2%.
Truncal valve repair
The degree of TrV regurgitation is classified subjectively as none, mild, moderate and severe in most series. There is no evidence to support what degree of regurgitation merits intervention, but most series favour TrV repair in all cases of severe regurgitation. No recommendation can be given on the value of intervention in cases of moderate regurgitation.
A variety of repair techniques have been described that depend on the degree of dilatation of the annulus, the number of leaflets and the degree of dysplasia of the leaflets themselves. Reference Backer125 Complete and partial annuloplasties have been used for a dilated annulus; leaflet thinning and release of fused commissures, for thickened valves; free edge plication and resuspension of commissures, for prolapsing leaflets; and cusp exclusion or union of neighbouring cusps, for localized dysplasia of 1 or 2 cusps. Most reports are a mixture of techniques and indications with variable results. A summary is shown in Table 14.
Table 14. Summary of surgical techniques commonly applied in truncal valve repair.

a Level of evidence.
b Class of recommendation.
There is good evidence that repair should be undertaken in all cases of severe regurgitation. Best results are achieved with annuloplasty or cusp exclusion types of procedures, whereas leaflet procedures or cusp repairs have poor outcomes. Reference Kaza, Burch, Pinto, Minich, Tani and Hawkins137–Reference Fujiwara, Imai, Yoshizawa, Ohno, Sakazaki and Tukuda141 Tricuspidization of quadricusp valves is associated with better outcomes, although the quadricusp valve has overall worse outcomes than trileaflet valves. Reference Myers, Bautista-Hernandez and del Nido140 Repair is likely to successfully reduce the degree of regurgitation; however, complete abolition of the regurgitation is usually not possible. Freedom from the need for subsequent reintervention is poor, with >50% of cases requiring rerepair or replacement within 5 years. Only 25% of patients are likely to survive without reoperation on the TrV at 20 years of age. Reference Naimo, Fricke and Yong76 The need for concomitant TrV repair at the time of the initial CAT repair increases the operative risk by up to 3 times, Reference Russell, Pasquali and Jacobs111 reflecting the risk of >moderate TrR in this condition.
TrV replacement should be avoided in neonatal CAT repair whenever possible. Reference Chai, Jacobs and Quintessenza142 Outcomes are extremely poor for replacement during the primary repair, with mortality approaching 100%. It is also noted that a combination of IAA with severe TrV regurgitation carries an extremely poor prognosis. Reference Russell, Pasquali and Jacobs111
Reconstruction of the right ventricular outflow tract
Repair of CAT can be achieved either by placing a valved conduit between the RV and PA (RV-PA) or by creating a direct anastomosis of the PAs to the ventriculotomy, without a conduit (Tables 15 and 16). Both alternatives have been widely used, with the majority of cases utilizing a valved conduit; a variety of modifications of each strategy have been described. Extensive mobilization of both PAs down to the hilus is recommended to prevent stretching of the RPA and to facilitate a direct anastomosis. There is no evidence to support 1 strategy over another in terms of survival or operative outcome; similar early outcomes have been described with both techniques. However, there are no randomized trials, and patient characteristics are not always comparable within individual series. There is insufficient evidence to suggest that certain morphological subtypes may be better suited to a particular strategy, but there is evidence that cases with >moderate TrR achieve better outcomes with a valved conduit because it avoids the volume loading of regurgitant flow in both ventricles.
Table 15. Techniques for reconstruction of the right ventricular outflow tract.

CAT = common arterial trunk; LAA = left atrial appendage; Pas = pulmonary arteries; PR = pulmonary regurgitation.
Table 16. Conduits for reconstruction of the right ventricular outflow tract.

There is good evidence that the direct anastomosis technique provides longer freedom from reoperation on the RVOT. Reference Luo, Zheng and Zhu97,Reference Danton, Barron and Stumper128 Although some studies have found that catheter reintervention is no different from those with an RV-PA conduit, there is strong evidence that these techniques delay the need for surgical reintervention at the cost of an increased degree of pulmonary regurgitation (PR) compared with the use of conduits. Reference Vouhe143–Reference Xu and Shen145,Reference Honjo, Kotani and Akagi147–Reference Raisky, Ali and Bajolle149,Reference Barbero-Martial and Tanamati152 There is no evidence to relate the PA arrangement to the suitability of each technique, but the direct anastomosis technique is likely to be easiest in anatomical types where the LPA and RPA arise from the aorta with a common stem and to become more difficult in patients with separate pulmonary ostia with widely spaced orifices due to the tension placed on the RPA.
Valved conduits have been the most prevalent technique used in the literature to reconstruct the RVOT. Homografts have the best performance in terms of freedom from reintervention, with pulmonary outperforming aortic homografts in most series. Reference Sinzobahamvya, Boscheinen and Blaschczok113,Reference Tlaskal, Chaloupecky and Hucin154,Reference Niemantsverdriet, Ottenkamp, Gauvreau, Del Nido, Hazenkamp and Jenkins155 In common with all conduits, the small sizes required in neonatal repair mean that reintervention is inevitable and usually relatively early compared with the use of conduits in older children. Freedom from surgical conduit replacement is described as 40–60% at 5 years in most larger studies. Reference Sinzobahamvya, Boscheinen and Blaschczok113,Reference Danton, Barron and Stumper128,Reference Tlaskal, Chaloupecky and Hucin154,Reference Niemantsverdriet, Ottenkamp, Gauvreau, Del Nido, Hazenkamp and Jenkins155,Reference McElhinney, Rajasinghe, Mora, Reddy, Silverman and Hanley160 Homografts are the most widely used conduit, followed by the bovine jugular vein (Contegra®, Medtronic, Minneapolis, MN, USA), which is reported to have good handling characteristics but inferior freedom from degeneration and outgrowth compared to that of homografts. Reference Sinzobahamvya, Boscheinen and Blaschczok113,Reference Chen, Gao and Hua119,Reference Tlaskal, Chaloupecky and Hucin154,Reference Hickey, McCrindle and Blackstone158,Reference Sinzobahamvya, Asfour and Boscheinen159 Dacron valved conduits have been used in small numbers and valveless Gore-Tex® tubes (W. L. Gore & Associates) in a handful of cases, but with insufficient numbers to be able to draw conclusions on the relative merits, only that they can all be safely used. Reference Luo, Zheng and Zhu97,Reference Danton, Barron and Stumper128,Reference Chen, Glickstein and Davies148,Reference Sandrio, Ruffer, Purbojo, Glockler, Dittrich and Cesnjevar153,Reference Niemantsverdriet, Ottenkamp, Gauvreau, Del Nido, Hazenkamp and Jenkins155,Reference Curi-Curi, Cervantes, Soulé, Erdmenger, Calderón-Colmenero and Ramírez162 An expanded polytetrafluoroethylene conduit (with bulging sinuses and a fan-shaped valve of the same material) shows promising results and may be useful in the future. Reference Miyazaki, Yamagishi and Maeda163
Interrupted arch repair
IAA occurs in 10–15% of all cases of CAT and carries a higher operative risk as described previously. Evidence indicates that the best outcomes are achieved using bypass management with two arterial cannulae to ensure equal perfusion and cooling of the entire circulation. Placement of a small Gore-Tex® shunt (W. L. Gore & Associates) on the innominate artery has been recommended because this allows better access for the cross-clamp and also can be used to deliver selective antegrade perfusion to the brain during arch repair. The interruption is most commonly type B. The techniques for arch repair are similar to those in other conditions with IAA and have most commonly been performed using a combination of a direct anastomosis with patch augmentation of the concavity of the reconstructed aortic arch. The use of a patch has the advantage that it may also be used for repair of the defect created by excising the PAs. Other authors have reported using direct anastomosis for IAA repair without a patch; the reported outcomes are similar with all techniques. The need for reoperation on the arch is rare (<10%).
Palliative repair leaving the ventricular septal defect open
This alternative approach has very few reported cases and no comparison with more standard approaches. The PAs are separated from the trunk and then connected to the RV with a valveless, small (typically 5–6 mm) Gore-Tex® tube (W. L. Gore & Associates), thereby leaving the VSD open. The limited reports regarding this approach show that it is safe; however, there is no evidence to recommend its use over standard repair. Reference Sandrio, Ruffer, Purbojo, Glockler, Dittrich and Cesnjevar153
Reoperations
Almost all patients with CAT will need reinterventions. Parents or caretakers should be informed about this situation from the beginning. Reinterventions should always be discussed by a multidisciplinary team, and a careful preoperative/preintervention work-up is mandatory.
Truncal valve reoperation
Reoperation is performed predominantly for TrV (now the neoaortic valve) regurgitation. Stenosis is extremely rare. Typically, 20–25% of all patients with CAT will need a reoperation on the TrV. The majority of these patients will have undergone some sort of valve repair at the time of the definitive repair; freedom from reoperation in this group is approximately 50% at 5 years. Reference Russell, Pasquali and Jacobs111,Reference Patrick, Mainwaring and Carrillo122,Reference Kaza, Burch, Pinto, Minich, Tani and Hawkins137–Reference Myers, Bautista-Hernandez and del Nido140,Reference Chai, Jacobs and Quintessenza142 Repair techniques reflect the fact that these procedures are being performed in an older age group than the neonatal repairs and that the valves are typically retracted and distended from chronic regurgitation. Techniques include subcoronary annuloplasty, bicuspidization, leaflet extensions and commissural resuspension. There is insufficient evidence to recommend or compare different techniques for valve repair, but the limited series suggest that repair can be achieved in a considerable number of patients, with a trend towards the predominance of repair over replacement in recent years. Reference Myers, Bautista-Hernandez and del Nido140,Reference Fujiwara, Imai, Yoshizawa, Ohno, Sakazaki and Tukuda141 The valve is typically replaced with a mechanical prosthesis when repair is no longer possible.
When the aortic root diameter exceeds 55 mm later in life, surgical repair is generally indicated. Reference Carlo, McKenzie and Slesnick64,Reference Gutierrez, Binotto, Aiello and Mansur65,Reference Erbel, Aboyans and Boileau164
Right ventricular outflow tract reoperation
The need for reintervention on the RVOT is likely to be inevitable in CAT, but the timing is influenced by the size and type of RVOT reconstruction used at the initial procedure. Lifelong follow-up of all patients with CAT is strongly recommended because the majority will need reintervention, usually on the RVOT. All conduits eventually become restrictive through a combination of degeneration and out-growth, with some limited evidence that conduit duration is best in pulmonary homografts, followed by aortic homografts and bovine jugular vein conduits. There are multiple studies of RV-PA conduits that include patients with CAT, but with insufficient evidence to recommend 1 conduit type over another at the time of reoperation. Larger conduits tend to perform better than smaller ones, and it is recommended that, at the first reoperation, the conduit should be at least 16 mm in diameter. The timing for conduit replacement is no different in CAT than in other situations and is based on a composite indication of raised RV pressures (>67% systemic pressure in the RV), impaired RV function and the development of exercise limitation associated with conduit stenosis or impaired function. Reference Kaza, Lim and Dibardino112,Reference Sinzobahamvya, Boscheinen and Blaschczok113,Reference Derby, Kolcz, Gidding and Pizarro146–Reference Chen, Glickstein and Davies148,Reference Barbero-Martial and Tanamati152,Reference Niemantsverdriet, Ottenkamp, Gauvreau, Del Nido, Hazenkamp and Jenkins155,Reference Brown, Ruzmetov, Rodefeld, Vijay and Turrentine157–Reference McElhinney, Rajasinghe, Mora, Reddy, Silverman and Hanley160,Reference Baumgartner, De Backer and Babu-Narayan165 It has been reported that RV-PA conduits do not last as long in patients with CAT as in patients with other conditions. Reference Buber, Assenza and Huang161
Patients with no conduit are likely to have longer freedom from reoperation than those with an RV-PA conduit (see Reconstruction of the right ventricular outflow tract above), but most will require reintervention due either to PR, to a degree of stenosis in the RVOT or to a combination of both. Reference Danton, Barron and Stumper128,Reference Raisky, Ali and Bajolle149 The indications for intervention in PR are not well defined in CAT, and practice is determined by extrapolation of the indications in repaired tetralogy of Fallot, based on indexed RV volumes and the development of symptoms. In equivocal cases, cardiopulmonary exercise testing may aid decision-making. Choice of RVOT replacement in these cases can be either with a homograft valved conduit or, in older children, with a valved xenograft in the pulmonary position accommodated by an outflow tract patch. Both techniques have been used with equal success. Reference Tlaskal, Chaloupecky and Hucin154,Reference Buber, Assenza and Huang161
Overall, RVOT reoperation in CAT is safe and would be expected to have a low operative mortality.
Percutaneous reinterventions on right ventricular outflow tract, right ventricle-to-pulmonary artery conduits and pulmonary arteries
Interventional therapies such as balloon dilatation and stent implantation can improve the lifespan of obstructed RV-to-PA conduits Reference Peng, McElhinney and Nugent166–Reference Carr, Bergersen and Marshall168 and may therefore be reasonable in severely obstructed conduits. Reference Carr, Bergersen and Marshall168 Stent implantation proved to be safe, Reference Peng, McElhinney and Nugent166,Reference Sugiyama, Williams and Benson167 even in smaller homograft conduits. Reference Carr, Bergersen and Marshall168 However, stenting of the conduit results in free PR with possible side effects such as RV dilatation, RV dysfunction and arrhythmias. Percutaneous pulmonary valve replacement was first reported nearly 20 years ago Reference Bonhoeffer, Boudjemline and Saliba169 and can now be considered as an alternative to surgical pulmonary valve replacement in selected patients. Reference McElhinney, Hellenbrand and Zahn170,Reference Lurz, Coats and Khambadkone171 For both stenting of the conduit and percutaneous pulmonary valve replacement, coronary artery compression testing is indicated. Reference Stout, Daniels and Aboulhosn172–Reference Fraisse, Assaidi and Mauri174 In patients with additional lesions requiring intervention (e.g. tricuspid valve regurgitation, TrV regurgitation), surgical intervention is preferred. Multidisciplinary team discussion with a risk-benefit analysis, before interventional stent implantation or percutaneous pulmonary valve replacement, is recommended.
Patients with CAT are at risk of developing branch PA stenoses leading to RV pressure load and to differences in right and LPA blood flow. Reference Asagai, Inai and Shinohara110,Reference Lund, Vogel and Marshall129,Reference Tlaskal, Chaloupecky and Hucin154 Assessment of the significance of stenosis should include symptoms, echocardiographic findings and crosssectional imaging data. Balloon dilatation and stenting of relevant branch pulmonary stenoses might be useful. Reference Stout, Daniels and Aboulhosn172,Reference Gonzalez, Kenny, Slyder and Hijazi175,Reference Kenny, Amin, Slyder and Hijazi176
Intraoperative assessment
Intraoperative transoesophageal echocardiography
Intraoperative transoesophageal echocardiography (TOE) during or after surgery plays a major role in detecting residual lesions and is considered the standard in patients undergoing cardiac surgery. Reference Smallhorn177,Reference Ayres, Miller-Hance and Fyfe178 The patient’s minimum weight for using intraoperative TOE is typically 2.5 kg and caution is recommended in children who weight <3 kg. Reference Ayres, Miller-Hance and Fyfe178 The most important reporting elements in patients with CAT are listed in Table 17. Reference Yoo, Kim and Bae82
Table 17. Proposed standard intraoperative transoesophageal echocardiography and reporting elements. Reference Yoo, Kim and Bae82

AV = atrioventricular; CAT = common arterial trunk; Pas = pulmonary arteries; RV-to-PA conduit = right ventricle to pulmonary artery conduit; TOE = transoesophageal echocardiography; VSD = ventricular septal defect.
Epicardial echocardiography has a role for patients in whom TOE cannot be used or in whom TOE does not provide sufficient visualization of particular cardiac structures. It has been demonstrated that epicardial echocardiography allows detection of the majority of residual lesions. Reference Muhiudeen, Roberson, Silverman, Haas, Turley and Cahalan179,Reference Manvi, Dixit, Srinivas, Vagarali, Patil and Manvi180 A disadvantage is that the transducer is placed directly on the heart, which can promote arrhythmias and haemodynamic compromise. Reference Smallhorn177
Postoperative management in the intensive care unit
The postoperative course after surgery for CAT can be complicated for many reasons. Pulmonary hypertension may occur, especially when surgery is performed later. Reactive pulmonary vasculature and pulmonary vascular obstructive disease are known to develop rapidly in CAT, and there is a relation between later timing of the operation and pulmonary hypertensive complications postoperatively. Reference Stapleton, Wilmot and Suh90,Reference Hosseinpour and Shinebourne91,Reference Kozlik-Feldmann, Hansmann, Bonnet, Schranz, Apitz and Michel-Behnke181 After the patient is weaned from cardiopulmonary bypass, the degree of pulmonary hypertension should be measured by intraoperative TOE (or epicardial echocardiography if the child is too small for TOE). The tricuspid valve Doppler gradient is recorded. When the central venous pressure is added, one has a reliable measurement of systolic RV pressure, which equals systolic PA pressure in the absence of a gradient between the RV and PAs. If RV pressure cannot be reliably recorded (e.g. when there is no tricuspid insufficiency), direct puncture of the RV (or RV to PA connection) may form an alternative.
If pulmonary hypertension prohibits weaning from cardiopulmonary bypass or if it results in supra- or near-systemic RV pressures, the recommendation is to administer respiratory nitric oxide at 20 ppm. Reference Kaestner, Schranz, Warnecke, Apitz, Hansmann and Miera182 Usually cardiopulmonary bypass can be discontinued thereafter, and the patient can be transported to the paediatric ICU. Reactive pulmonary vasculature and pulmonary hypertensive crisis may be caused by pain, unrest and bronchial suction. Therefore, adequate analgesia and sedation are mandatory in the immediate postoperative period. The rebound effect of nitric oxide withdrawal on pulmonary hypertension can be countered by intravenous administration of sildenafil, which may be continued later in the oral form. Reference Kaestner, Schranz, Warnecke, Apitz, Hansmann and Miera182 Phosphodiesterase inhibitors, such as milrinone, have been described to improve results after many types of neonatal operations Reference Hoffman, Wernovsky and Atz107 and are therefore also advised following CAT surgery. Noradrenaline can be combined with milrinone in the first postoperative phase. The chest may be left open for the first few days if haemodynamic instability is present or expected.
Both pulmonary hypertension and RVOT stenosis may lead to (supra-)systemic RV pressures and insufficient left ventricular filling, which in combination may cause rapid haemodynamic deterioration. Other residual defects must also be excluded and corrected before transportation to the ICU, including residual VSD, and more than mild tricuspid or TrV insufficiency.
High RV pressures and difficulty to wean the patient from cardiopulmonary bypass or an unstable course after arrival in the ICU may also be the result of RVOT stenosis. This must be sought after aggressively and treated when present: stretching of the RPA and kinking of the LPA have been described and can be the consequence of stretching by a too-short or kinking by a too- long conduit. Excessive dead volume of a big conduit can impair haemodynamics, and conduit pulsatility may cause dynamic obstruction of the LPA. If echocardiography fails to lead to a diagnosis of the exact cause of elevated RV pressure, a CT scan and/ or cardiac catheterization should be considered. Extracorporeal membrane oxygenation must be considered when conventional measures fail to have an adequate effect. It may also be helpful in providing sufficient haemodynamic stabilization to perform further diagnostic tests and (interventional) treatment when needed.
Adverse cardiac events are known to occur more frequently in patients with the 22q11.2 deletion. The duration of mechanical ventilation and the lengths of the ICU and hospital stays are reported to be longer. Reference O’Byrne, Yang and Mercer-Rosa133 Attention should be paid to hypocal- caemia and irradiation of blood products. Reference Shen, Gu and Wang95,Reference Parshuram, Doyle, Lau and Shemie102,Reference Ryan, Goodship and Wilson103
Postoperative assessment
Early postoperative transthoracic echocardiogram
Recent studies have shown that early mortality rates following CAT repair have decreased significantly in the last decades since the first report in 1968 by McGoon et al. Reference Naimo, Fricke and Yong76,Reference Tlaskal, Chaloupecky and Hucin154,Reference McGoon, Rastelli and Ongley183,Reference Jacobs, Mayer and Pasquali184 However, early residual lesions may occur and can complicate the postoperative course and the early follow-up of patients with CAT.
TTE plays a major role in the immediate postoperative assessment of patients with CAT and should focus on evaluation of the RV-to-PA conduit and the PA branches, the anatomy and function of the TrV, the evaluation of the aortic arch in patients with IAA and the assessment of biventricular size and function. Reference Yoo, Kim and Bae82 Specifically, attention should be paid to conduit obstruction and regurgitation, branch PA stenosis and hypoplasia, residual VSDs, regurgitation and stenosis of the TrV to detect complications, which might need early intervention and to obtaining postoperative baseline results for serial follow-ups. Patients with IAA are at risk for aortic arch obstruction; therefore, assessment of the aortic arch should be part of the postoperative TTE. Reference Brown, Ruzmetov, Okada, Vijay and Turrentine109,Reference Bohuta, Hussein and Fricke123 In the postoperative course, pulmonary hypertension can have an impact on management in the ICU. Reference Shamszad, Moore, Ghanayem and Cooper79 TTE should distinguish increased RV pressure caused by pulmonary hypertension from that from conduit or branch PA obstruction. Standard TTE views and reporting elements are listed in Table 18.
Table 18. Proposed postoperative and follow-up transthoracic echocardiographic views and reporting elements.

IAA = interrupted aortic arch; PA = pulmonary artery; RV-to-PA conduit = right ventricle to pulmonary artery conduit; TR = tricuspid regurgitation; TTE = transthoracic echocardiography; VSDs = ventricular septal defects.
Cardiovascular computed tomography and cardiovascular magnetic resonance imaging
Echocardiography is the first-line, standard imaging modality for immediate postoperative assessment. Reference Prakash, Powell and Geva85 Early postoperative assessment after surgical repair of CAT with CT or CMRI may be necessary in the context of poor echocardiographic windows to assess the reconstructed aortic arch in patients with IAA for obstruction or aneurysms, to evaluate the RV-to-PA conduit or to visualize the branch Pas. Reference Han, Rigsby and Hlavacek86,Reference Fogel and Crawford87
Cardiac catheterization and angiography
Early catheter-based reinterventions on the branch PAs and the RV-to-PA conduit after CAT repair in the neonatal period or early infancy may be necessary. Reference Stapleton, Wilmot and Suh90,Reference Lund, Vogel and Marshall129 These reinterventions can include balloon dilatation or stenting of the conduit or the PAs. Lund et al. Reference Lund, Vogel and Marshall129 reported that freedom from any RVOT or PA reintervention was 68±4% at 1 year and 48±5% at 2 years and that this result was mainly associated with a smaller conduit size. Catheter reinterventions for aortic arch stenosis in patients who had repair of an IAA may be necessary and typically occurred in the first 18 months after surgery, according to a recently published study. Reference Uzzaman, Khan and Davies185
Assessment during long-term follow-up
Follow-up recommendations
Lifelong individualized follow-up of patients with CAT is recommended (see also Table 19). Reference Haas and Schirmer191 In the first year after the operation, we suggest at least 3- to 6-month follow-up intervals and after that every 6–12 months. Reference Boris186,Reference Wernovsky, Rome and Tabbutt187 Adults with CAT should be seen by cardiologists who specialize in adults with congenital heart disease in specialist centres, in which recommendations for follow-up and care can be made on an individual basis. Reference Baumgartner, De Backer and Babu-Narayan165 Patients with pulmonary arterial hypertension and patients with Eisenmenger syndrome should be managed accordingly. Reference Baumgartner, De Backer and Babu-Narayan165,Reference Stout, Daniels and Aboulhosn172,Reference Kozlik-Feldmann, Hansmann, Bonnet, Schranz, Apitz and Michel-Behnke181,Reference Galié, Humbert and Vachiery192
Table 19. Follow-up recommendations.

ACHD = adults with congenital heart disease; CMRI = cardiovascular magnetic resonance imaging; CPET = cardiopulmonary exercise testing; ECG = electrocardiogram; TTE = transthoracic echocardiography.
a Level of evidence.
b Class of recommendation.
For children and adults with the 22q11.2 deletion syndrome, multidisciplinary management is advisable because it is a multisystem disorder that can also affect the endocrine, immune, haematological and musculoskeletal systems, as well as intelligence, mental health and other issues. Reference Fung, Butcher and Costain193,Reference Habel, Herriot and Kumararatne194
Clinical investigations
Clinical examination
Clinical evaluation should include oxygen saturation, blood pressure, arrhythmias, central venous pressure, heart murmurs and signs of heart failure. Findings related to the RV-to-PA conduit may include a precordial thrill, prominent A-wave of the jugular veins and a systolic murmur. Reference Baumgartner, De Backer and Babu-Narayan165 In patients with TrV regurgitation, a diastolic decrescendo murmur can be heard, and bounding peripheral pulses may be present. A chest X-ray may reveal RV-to-PA conduit calcification. Reference Baumgartner, De Backer and Babu-Narayan165
Electrocardiogram and 24-h ambulatory Holter monitoring
In the long-term follow-up of patients with CAT, a 12-lead ECG is part of the routine baseline diagnostic examination, especially in those patients who are on antiarrhythmic treatment. Reference Wernovsky, Rome and Tabbutt187,Reference Decker, McCormack and Cohen195 It is assumed that the arrhythmia burden and the risk for sudden cardiac death are similar to those in patients with tetralogy of Fallot with increased risk if the TrV is abnormal. Reference Decker, McCormack and Cohen195 Many patients have a bundle branch block, with a right bundle branch block being the most common finding. Reference O’Byrne, Mercer-Rosa and Zhao132 Attention should be paid to signs of right or left ventricular hypertrophy and/or dilatation, change in intraventricular conduction and pressure overload.
Twenty-four hour ambulatory Holter monitoring should be performed when indicated (Table 19). Reference Haas and Schirmer191 The frequency in adults should be individualized depending on the suspicion of arrhythmias and clinical findings (need for reoperation, progressive haemodynamic problems). Reference Baumgartner, De Backer and Babu-Narayan165,Reference Warnes, Williams and Bashore196
Transthoracic echocardiography
The consensus is that TTE is the primary non-invasive imaging modality and should be included in every follow-up visit (Table 18). Reference Prakash, Powell and Geva85 The echocardio- graphic evaluation of repaired CAT includes assessment of the RV-to-PA conduit (Fig. 5), PAs, the anatomy and function of the TrV (substrate of TrV regurgitation), aortic root size, residual VSD, biventricular function and right ventricular systolic pressure from tricuspid valve regurgitation velocity to assess conduit stenosis. Evaluation of the anatomy of the aortic arch is particularly important in patients who had repair of IAA.

Figure 5. Two-dimensional transthoracic echocardiogram illustrating the RV-to-PA conduit. ( a ) Colour-guided and Doppler echocardiography shows good RV-to- PA conduit function ( b and c ) PA = pulmonary artery; RV = right ventricle; RVOT = right ventricular outflowtract.
Similar to the situation in patients with tetralogy of Fallot or other congenital heart diseases, detailed visualization of the RV and its outflow tract, as well as of the PAs, is often limited by restricted acoustic windows, which can become even worse in adolescence and adulthood. Reference Valente, Cook and Festa197 Furthermore, quantitative assessment of the RV with its complex geometry and valve regurgitation can be challenging, typically requiring the complementary use of CMRI. Reference Valente, Cook and Festa197,Reference Kilner, Geva, Kaemmerer, Trindade, Schwitter and Webb198 Three-dimensional echocardiography allows highly repeatable quantification of right and left ventricular volumes and the ejection fraction but also depends on the acoustic window and produces lower volume measurements compared with CMRI. Reference Simpson, Lopez and Acar84,Reference Grewal, Majdalany, Syed, Pellikka and Warnes199
Cardiovascular magnetic resonance imaging
CMRI plays an increasing role in the long-term follow-up of patients with congenital heart disease. It is the reference standard modality for biventricular volume and mass assessment and is well suited for life-long repeated follow-up studies. Reference Kilner, Geva, Kaemmerer, Trindade, Schwitter and Webb198,Reference Mannaerts, Van Der Heide and Kamp200,Reference Malm, Frigstad, Sagberg, Larsson and Skjaerpe201 CMRI cine imaging and angiographic techniques are valuable in visualization of the RV-to-PA conduit or connection and of the PAs, which may become stenotic after CAT repair. Reference Fogel and Crawford87,Reference Valsangiacomo Buechel, Grosse-Wortmann and Fratz202 Furthermore, residual VSDs, the TrV anatomy and the aortic arch can easily be visualized. Phase-contrast CMRI allows quantification of the RV-to-PA conduit and TrV regurgitation and enables measurement of peak velocities across the TrV and conduit. For patients with residual VSDs, the shunt (Qp/Qs) can be quantified with flow measurements above the TrV and in the RV-to-PA conduit. Reference Beerbaum, Körperich, Barth, Esdorn, Gieseke and Meyer203 Viability imaging using the late gadolinium enhancement technique is able to detect myocardial fibrosis. In patients with tetralogy of Fallot, the presence of myocardial fibrosis was related to adverse clinical markers, such as ventricular dysfunction and exercise intolerance. Reference Babu-Narayan, Kilner and Li204,Reference Wald, Haber, Wald, Valente, Powell and Geva205
The timing of CMRI in patients after CAT repair depends on the clinical course and findings. In patients younger than 10 years of age, CMRI is recommended when there is a concern about unfavourable disease progression and echocardiographic data are insufficient to answer the clinical question (Table 19). Reference Valente, Cook and Festa197 In adolescent and adult patients with stable clinical and echocardiographic findings, follow-up with CMRI is recommended every 3–5 years in stable patients and every 12 months in patients with progressive findings (progressive RV/left ventricular dilatation or dysfunction) or when reoperation is being considered. Reference Valente, Cook and Festa197 Late gadolinium enhancement imaging should be performed at the time of the first CMRI examination and when there is clinical deterioration. Reference Stout, Daniels and Aboulhosn206 Table 20 illustrates the proposed measurements and reporting elements.
Table 20. Proposed CMRI measurements and reporting elements. Reference Warnes, Williams and Bashore196

BSA = body surface area; CMRI = cardiovascular magnetic resonance imaging; IAA = interrupted aortic arch; LGE = late gadolinium enhancement; LPA = left pulmonary artery; LV = left ventricle; Pas = pulmonary arteries; RPA = right pulmonary artery; RV = right ventricle; RV-to-PA conduit = right ventricle to pulmonary artery conduit.
Computed tomography
CT is an imaging modality that is well suited for the anatomical evaluation of the RV-to-PA conduit, the branch PAs, the aortic arch and the aortic root, especially if echocardiography is not sufficient. Reference Han, Rigsby and Hlavacek86,Reference Saremi, Ho, Cabrera and Sáanchez-Quintana207 In patients with contraindications for CMRI, CT can provide comparable information regarding ejection fraction and ventricular volumes. Reference Han, Rigsby and Hlavacek86,Reference Takx, Moscariello and Schoepf208,Reference Maffei, Messalli and Martini209 CT is the modality of choice for coronary assessment before reoperations or reinterventions and is able to provide detailed information about coronary origins, course and relationship to the great vessels. Reference Han, Rigsby and Hlavacek86,Reference Valente, Cook and Festa197
Cardiac catheterization and (coronary) angiography
In adult patients with a history of ischaemic heart disease, 1 or more cardiovascular risk factors, suspected ischaemia, male patients >40 years of age and postmenopausal female patients, or in case of another indication for preoperative cardiac catheterization, coronary angiography is recommended before surgery. Reference Falk, Baumgartner and Bax188 Cardiac catheterization with haemodynamic assessment can be of use when surgical or interventional treatment is considered. Reference Baumgartner, De Backer and Babu-Narayan165 Endovascular stenting of obstructed RV-to-PA conduits has been shown to decrease RV pressure and prolong conduit lifespan. Reference Peng, McElhinney and Nugent166,Reference Sugiyama, Williams and Benson167 Transcatheter pulmonary valve replacement is a less invasive method compared with repeat open-heart surgery for dysfunctional RV-to-PA conduits in older patients (>5 years of age, >20 kg), and recent data show good short- and longer-term results. In a U.S. trial, 15 out of 150 patients who received a Melody valve (Medtronic) had CAT. Reference Cheatham, Hellenbrand and Zahn189,Reference Eicken, Ewert and Hager190 Catheterization with manometry is often the method of choice if aortic arch obstruction is suspected and offers the possibility of balloon aortic arch angioplasty or a stent implant. Reference Bohuta, Hussein and Fricke123
Cardiopulmonary exercise testing
In adults with congenital heart disease, exercise intolerance is common and associated with increased risk of hospitalization and death. Reference Diller, Dimopoulos and Okonko210 For patients after CAT repair, reduced exercise capacity has also been demonstrated. Reference O’Byrne, Mercer-Rosa and Zhao132 The consensus is that cardiopulmonary exercise testing should be introduced into the diagnostic work-up when the patient is able to do the test (from 8 years of age upwards) and should be performed on a regular basis during long-term follow-up (Table 19).
Late management of residual or new lesions
Management of truncal valve regurgitation
TrV incompetence is a frequent finding in patients with CAT during follow up due to dysplasia and anatomical variations of the valve. Reference Henaine, Azarnoush and Belli139 Similarly to other patient groups, patients with CAT with TrV regurgitation should be monitored closely. Reference Sarris, Balmer and Bonou211 The indication for vasodilator therapy in TrV regurgitation is unclear. In a small paediatric study, which included a few patients with CAT, no significant effect of angiotensin-converting enzyme inhibitors on left ventricular dilatation or function was found. Reference Gisler, Knirsch, Harpes and Bauersfeld212 Studies in adult patients with chronic aortic regurgitation have reported controversial results, Reference Evangelista, Tornos, Sambola, Permanyer-Miralda and Soler-Soler213,Reference Schön214 and 1 recent meta-analysis indicated that vasodilators had a favourable effect on left ventricular remodelling (Table 21). Reference Shah, Singh, Bhuriya, Molnar, Arora and Khosla215
Table 21. Recommendation for vasodilator therapy.

CAT = common arterial trunk.
a Level of evidence.
b Class of recommendation.
General consensus regarding timing of surgical TrV treatment is lacking. However, for patients with moderate-to-severe TrV incompetence, surgical treatment should be considered, especially when symptoms or a positive exercise test co-exist. Reference Myers, Bautista-Hernandez and del Nido140,Reference Falk, Baumgartner and Bax188
Truncal root dilatation
The truncal root is commonly dilated in patients with CAT, which is probably related to intrinsic structural vessel wall abnormalities. Reference Carlo, McKenzie and Slesnick64,Reference Niwa, Perloff and Bhuta216 Carlo et al. Reference Carlo, McKenzie and Slesnick64,Reference Gutierrez, Binotto, Aiello and Mansur65,Reference Frischhertz, Shamszad, Pedroza, Milewicz and Morris217 showed that patients with severe TrV regurgitation have a higher truncal root z-score; however, the risk for complications such as aortic dissection is rare. Assessment of the size of the aortic root with echocardiography is recommended during follow up and should be complemented by CMRI or CT if surgical aortic intervention is considered or the echocardiographic windows are poor. Reference Erbel, Aboyans and Boileau164,Reference Zanjani and Niwa218 Surgical repair is generally indicated when the aortic size exceeds 55 mm. Reference Carlo, McKenzie and Slesnick64,Reference Gutierrez, Binotto, Aiello and Mansur65,Reference Erbel, Aboyans and Boileau164
Right ventricular outflow tract obstruction
According to current guidelines, RVOT obstruction at any level should be repaired regardless of symptoms when the Doppler peak gradient is >64 mmHg (peak velocity >4 m/s), provided that RV function is normal and no valve substitute is required.
In asymptomatic patients in whom balloon valvotomy is ineffective and surgical valve replacement is the only option, surgery should be performed in the presence of a systolic RV pressure >80 mmHg (tricuspid regurgitation velocity > 4.3 m/s). Intervention in patients with a gradient <64 mmHg should be considered in the presence of the following:
-
Symptoms related to pulmonary stenosis, or
-
Decreased RV function, or
-
Double-chambered RV (which is usually progressive), or
-
Important arrhythmias, or
-
Right-to-left shunting via an atrial septal defect or VSD. Reference Baumgartner, De Backer and Babu-Narayan165
Endocarditis prophylaxis
Infective endocarditis is a serious complication. Patients with CAT are at high-risk of developing infective endocarditis mainly due to implanted prosthetic valves in the pulmonary position (RV-to- PA conduit) or prosthetic material used for pulmonary valve repair. Reference Baumgartner, De Backer and Babu-Narayan165,Reference Habib, Lancellotti and Antunes219 According to current guidelines, antibiotic infective endocarditis prophylaxis is recommended in all types of cyanotic congenital heart diseases, thus encompassing all patients with unrepaired CAT. It is also recommended in patients repaired with a prosthetic material, whether placed surgically or by percutaneous techniques, up to 6 months after the procedure or lifelong if a residual shunt or valvular regurgitation remains, which is applicable to the majority of patients with CAT after repair. Reference Habib, Lancellotti and Antunes219 Patients should also be encouraged to have regular dental examinations and to maintain good oral hygiene. Reference Baumgartner, De Backer and Babu-Narayan165,Reference Habib, Lancellotti and Antunes219
Exercise and sport
No specific recommendations for patients after CAT repair exist. However, physical activity has a known benefit for fitness and social integration. Reference Baumgartner, De Backer and Babu-Narayan165,Reference Haas and Schirmer191
In general, clinical assessment before sport recommendation should be performed. Reference Longmuir, Brothers and De Ferranti220 For children with congenital heart disease, sport eligibility screening was suggested, latest at a preschool age. Reference Freedom, Yoo, Freedom, Yoo, Mikailian and Williams53 In addition to a detailed history and cardiology investigations including TTE, ECG and a Holter ECG, formal exercise testing (preferably cardiopulmonary exercise testing) is often indicated. Reference Haas and Schirmer191,Reference Longmuir, Brothers and De Ferranti220,Reference Takken, Giardini and Reybrouck221 Detailed recommendations should be made on an individualized basis and should consider the patient’s morbidities, which may include arrhythmias, ventricular dysfunction, pulmonary hypertension or pulmonary vascular obstructive disease, severity of residual lesions, oxygen saturation, aortic dilatation, anticoagulation and implanted devices. Reference Haas and Schirmer191,Reference Takken, Giardini and Reybrouck221
Pregnancy
Preconception counselling is important, and the issues surrounding pregnancy, contraception and family planning should already have been addressed in adolescence. Reference Uebing, Steer, Yentis and Gatzoulis222 All women with repaired CAT should be offered prepregnancy risk assessment and counselling as well as genetic counseling. Reference Uebing, Steer, Yentis and Gatzoulis222,Reference Regitz-Zagrosek, Roos-Hesselink and Bauersachs223 Patients with Eisenmenger syndrome who have not undergone repair have a high maternal mortality. Reference Avila, Grinberg and Snitcowsky224 In accordance with the European Society of Cardiology guidelines on the management of cardiovascular diseases during pregnancy, we recommend using the modified World Health Organization classification of pregnancy risk to assess risk. Reference Regitz-Zagrosek, Roos-Hesselink and Bauersachs223,Reference Thorne, Macgregor and Nelson-Piercy225
Care during pregnancy and delivery and in the post-partum period should involve a multidisciplinary team, including a cardiologist trained in adult congenital heart disease, cardiac surgeons, obstetricians, anaesthetists and neonatologists. Individualized care plans documenting follow-up schedules during pregnancy and the post-partum period, as well as the preferred mode of delivery, are useful (Table 22).
Table 22. Recommendations for prepregnancy counselling and care during pregnancy.

CAT = common arterial trunk.
a Level of evidence.
b Class of recommendation.
Outcomes
Surgical repair of CAT is major surgery. It is to be expected that all patients who survive the initial repair will need 1 or more reoperations and/or catheter interventions in the future. Additional lesions, such as IAA and dysfunction of the TrV, need associated surgical repair and carry additional risks.
Looking at the outcomes in the congenital cardiac surgical databases, we found a total of 1569 patients with CAT repair in the European Congenital Heart Surgeons Association Database and a hospital mortality of 15.8%. The number of patients with CAT and associated IAA repair was 61, having a hospital mortality of 9.8%. 228 A report from the Society of Thoracic Surgeons Congenital Heart Surgery Database shows an operative mortality of 9.5% in 602 CAT repairs in the period January 2014 through December 2017. Reference Jacobs, Mayer and Pasquali184
Importantly, mortality following CAT repair has decreased over the years, as has been reported by the aforementioned databases and also by Tlaskal et al. Reference Tlaskal, Chaloupecky and Hucin154 In a review of 83 patients operated on between 1981 and 2009, mortality was 46% between 1981 and 1996 and only 4% between 1997 and 2009. A total of 14 patients with IAA repair and 8 patients with TrV repair were included in this series.
Simultaneous repair of IAA and/or TrV dysfunction carries an extra risk of death, as was shown in a 2012 update from the Society of Thoracic Surgeons Congenital Heart Surgery Database where, in the period between 2000 and 2009, a total of 572 CAT repairs were reported with a hospital mortality of 10% when CAT repair was isolated, 30% when associated with TrV repair and 24% when associated with IAA repair. When CAT repair was performed with both IAA and TrV surgery, mortality was 60%. Reference Russell, Pasquali and Jacobs111
Long-term survival is reported to be 73.6% after 30 years by the Melbourne group. Freedom from RVOT-related reoperation at 20 years was 4.6%. Reference Naimo, Fricke and Yong76
Conflict of interest
None declared.
Author contributions
Mark Hazekamp: Conceptualization; Data curation; Formal analysis; Investigation; Methodology; Project administration; Supervision; Writing-original draft; Writing-review & editing). David Barron: Conceptualization; Formal analysis; Investigation; Methodology; Writing-original draft; Writing- review & editing. Joanna Dangel: Conceptualization; Formal analysis; Investigation; Methodology; Writing-original draft; Writing-review & editing. Tessa Homfray: Conceptualization; Formal analysis; Investigation;
Methodology; Writing-original draft; Writing-review & editing. Monique Jongbloed: Conceptualization; Formal analysis; Investigation; Methodology; Writing-original draft; Writing-review & editing. Inga Voges: Conceptualization; Formal analysis; Investigation; Methodology; Project administration; Writing-original draft; Writing-review & editing.