Influenza in swine
Influenza is a zoonotic disease caused by influenza virus which infects a wide variety of species including humans, pigs, horses, sea mammals and birds. Influenza virus was first isolated in the United States in 1930 (Shope, Reference Shope1931) and transmission between species happens occasionally (Vincent et al., Reference Vincent, Ma, Lager, Janke and Richt2008a). Sero-archeological studies of human samples from 1918 to 1920 showed the original causative virus of the 1918 pandemic flu was closely related to influenza virus A/Swine/Iowa/30 (H1N1) strain, which is now referred to as classic H1N1 (cH1N1) (Webster, Reference Webster1999).
Viral characteristics
Influenza virus belongs to the family Orthomyxoviridae. Three types of influenza virus, types A, B and C, are differentiated on the basis of antigenic characteristics of the nucleoprotein (NP) (Mahy, Reference Mahy and Mahy1997; Alexander and Brown, Reference Alexander and Brown2000). Pathogenic influenza viruses in domestic animals are type A viruses (Maclachlan and Dubovi, Reference Maclachlan, Dubovi, Maclachlan and Dubovi2011). Influenza A viruses (IAV) are enveloped and pleomorphic, with a size of around 80–120 nm and possess eight single stranded, negative-sense RNA genome segments packaged within virions (Maclachlan and Dubovi, Reference Maclachlan, Dubovi, Maclachlan and Dubovi2011). Twelve proteins are encoded by these eight segments, including hemagglutinin (HA), neuraminidase (NA), matrix protein 1 (M1) and 2 (M2), polymerase basic 1(PB1) and 2 (PB2), NP, polymerase acidic (PA), PB1-F2, N-terminally truncated version of polypeptide translated from codon 40 of PB1 (PB1-N40) and non-structural protein 1 (NS1) and 2 (NS2) (Wise et al., Reference Wise, Foeglein, Sun, Dalton, Patel, Howard, Anderson, Barclay and Digard2009; Maclachlan and Dubovi, Reference Maclachlan, Dubovi, Maclachlan and Dubovi2011). Structural proteins HA, NA, M1 and M2 form the envelope of IAV with the cellular lipid bilayer. HA protein plays a critical role during IAV cell entry. HA attachment to permissive cell sialic acid receptor on the plasma membrane initiates virus entry into cells via receptor-mediated endocytosis (Murphy et al., Reference Murphy, Gibbs, Horzinek, Studdert, Murphy, Gibbs, Horzinek and Studdert1999). NA also binds to cell receptor sialic acid. During the detachment of mature progeny virus from host cells, the binding of NA and sialic acid on the same host cell prevents progeny virus self-aggregation back to the same host cell mediated by HA (Grienke et al., Reference Grienke, Schmidtke, von Grafenstein, Kirchmair, Liedl and Rollinger2012). In addition, the surface glycoproteins HA and NA induce protective-specific immune responses in the host, but are not highly conserved (Alexander and Brown, Reference Alexander and Brown2000). At present, 17 distinct HA antigenic subtypes and 10 NA subtypes are identified (Bouvier and Palese, Reference Bouvier and Palese2008; Tong et al., Reference Tong, Li, Rivailler, Conrardy, Castillo, Chen, Recuenco, Ellison, Davis, York, Turmelle, Moran, Rogers, Shi, Tao, Weil, Tang, Rowe, Sammons, Xu, Frace, Lindblade, Cox, Anderson, Rupprecht and Donis2012), allowing further sub-typing according to the combination of HA and NA proteins present on the virion surface.
PB1, PB2 and PA form a trimeric RNA polymerase complex that binds one end of RNA segments and forms ribonucleoprotein (RNP) complexes with NP (Klumpp et al., Reference Klumpp, Ruigrok and Baudin1997). RNP is required to transcribe positive strand messenger RNA (mRNA) and complementary RNA (cRNA), because negative strand RNAs cannot serve as translation templates directly (Baltimore et al., Reference Baltimore, Huang and Stampfer1970; Conzelmann, Reference Conzelmann1998). Segments 7 and 8 each encode two proteins (M1 and M2, NS1 and NS2, respectively) by differential splicing of mRNAs (Backstrom et al., 2011). NS1 protein plays multiple roles during viral replication and is not incorporated in progeny virus (Hale et al., Reference Hale, Randall, Ortin and Jackson2008; Shaw et al., Reference Shaw, Stone, Colangelo, Gulcicek and Palese2008; Matsuda et al., Reference Matsuda, Suizu, Hirata, Miyazaki, Obuse and Noguchi2010; Nivitchanyong et al., Reference Nivitchanyong, Yongkiettrakul, Kramyu, Pannengpetch and Wanasen2011). For example, NS1 interacts with phosphorylated serine threonine kinase Akt in cells and enhances Akt promoting anti-apoptotic activity (Matsuda et al., Reference Matsuda, Suizu, Hirata, Miyazaki, Obuse and Noguchi2010). NS1 also inhibits interferon production and antiviral effects, subsequently induced by interferon and enhances viral protein translation (Hale et al., Reference Hale, Randall, Ortin and Jackson2008). NS2 is also known as nuclear export protein (NEP) (Shaw et al., Reference Shaw, Stone, Colangelo, Gulcicek and Palese2008). Both M1 and NS2 are involved in mediating export of RNPs from the nucleus (O'Neill et al., Reference O'Neill, Talon and Palese1998; Akarsu et al., Reference Akarsu, Iwatsuki-Horimoto, Noda, Kawakami, Katsura, Baudin, Horimoto and Kawaoka2011). M2 tetramers in the virus capsid serve as ion channels after virion entry into the endosome. Changes in endosomal pH cause a conformational change in HA which allows fusion with the endosomal membrane. In an independent event, M2 pumps protons into the virion, which causes M1 (which is tightly associated with the RNPs) to release the RNPs so they can traffic to and enter the nucleus (Wang et al., Reference Wang, Takeuchi, Pinto and Lamb1993; Maclachlan and Dubovi, Reference Maclachlan, Dubovi, Maclachlan and Dubovi2011). M2 has an extracellular domain (M2e) that has been considered a potential vaccine component (Neirynck et al., Reference Neirynck, Deroo, Saelens, Vanlandschoot, Jou and Fiers1999). N40 is non-essential for viability and lacks transcriptase function, but interacts with other polymerases in the cellular environment and contributes to virus replication (Wise et al., Reference Wise, Foeglein, Sun, Dalton, Patel, Howard, Anderson, Barclay and Digard2009). Since influenza is an enveloped virus, antibodies can only easily bind to protein domains spiking out of the virus membrane. HA, NA and M2 proteins all have extracellular domains outside of the virus membrane. These three proteins all have the potential to be vaccine candidates that might induce humoral responses.
Swine IAV disease
When pigs are infected with IAV, an acute disease in the respiratory tract develops, similar to human infection. The incubation period of the disease is 1–3 days followed by sudden onset of clinical signs and recovery. Recovery usually occurs within 7–10 days following infection (Vincent et al., Reference Vincent, Ma, Lager, Janke and Richt2008a). High morbidity and low mortality rates are observed for most swine IAV strains (Vincent et al., Reference Vincent, Ma, Lager, Janke and Richt2008a). Characteristic clinical signs include fever, respiratory distress, coughing, sneezing, labored breathing, anorexia and prostration (Richt et al., Reference Richt, Lager, Janke, Woods, Webster and Webby2003; Ma et al., Reference Ma, Belisle, Mosier, Li, Stigger-Rosser, Liu, Qiao, Elder, Webby, Katze and Richt2011). Purple to red multifocal or coalescing consolidated areas are observed as gross lesions in the cranio-ventral lung lobes (Richt et al., Reference Richt, Lager, Janke, Woods, Webster and Webby2003; Vincent et al., Reference Vincent, Ma, Lager, Janke and Richt2008a). Acute epithelial necrosis with subsequent attenuation or reactive proliferation, bronchointerstitial pneumonia, atelectasis, bronchiolitis, proteinaceous fluid and peribronchiolar lymphocytic infiltration are typical microscopic changes within the lung (Richt et al., Reference Richt, Lager, Janke, Woods, Webster and Webby2003; Vincent et al., Reference Vincent, Ma, Lager, Janke and Richt2008a; Ma et al., Reference Ma, Vincent, Lager, Janke, Henry, Rowland, Hesse and Richt2010, Reference Ma, Belisle, Mosier, Li, Stigger-Rosser, Liu, Qiao, Elder, Webby, Katze and Richt2011). Virus shedding can be detected from nasal swabs and bronchoalveolar lavage (BAL) fluids. Young pigs are more susceptible to IAV than are adult pigs (Richt et al., Reference Richt, Lager, Janke, Woods, Webster and Webby2003). IAV co-infection with porcine reproductive and respiratory syndrome virus (PRRSV), porcine circovirus type 2 (PCV2), Mycoplasma hyopneumoniae (MHYO), Pasteurella multocida (PMULT) and other secondary bacterial infections in the respiratory tract of pigs leads to a syndrome known as porcine respiratory disease complex (PRDC) (Thacker et al., Reference Thacker, Thacker and Janke2001; Ellis et al., Reference Ellis, Clark, Haines, West, Krakowka, Kennedy and Allan2004; Opriessnig et al., Reference Opriessnig, Gimenez-Lirola and Halbur2011; Fablet et al., Reference Fablet, Marois-Crehan, Simon, Grasland, Jestin, Kobisch, Madec and Rose2012).
Swine IAV subtypes
IAV evolves continuously in two ways termed antigenic drift and antigenic shift. Minor changes of HA and NA proteins constitute antigenic drift involving the results of point mutations (substitutions, insertions and deletions) of nucleotides (Murphy et al., Reference Murphy, Gibbs, Horzinek, Studdert, Murphy, Gibbs, Horzinek and Studdert1999). Such minor mutations are due to polymerase errors that are common in RNA virus replication (Domingo et al., Reference Domingo, Baranowski, Ruiz-Jarabo, Martin-Hernandez, Saiz and Escarmis1998; Gauger and Vincent, Reference Gauger and Vincent2011). Antigenic drift may result in HA and NA types that are not recognized by antibodies induced prior to mutation. Antigenic shift constitutes major changes in gene combination or reassortment caused by exchange of whole gene segments between different strains which co-infect the same animal (Murphy et al., Reference Murphy, Gibbs, Horzinek, Studdert, Murphy, Gibbs, Horzinek and Studdert1999; Vincent et al., Reference Vincent, Ma, Lager, Janke and Richt2008a). These two mechanisms of evolution give rise to the emergence of variant viruses. Pigs are susceptible to challenge by many subtypes of IAV (Kida et al., Reference Kida, Ito, Yasuda, Shimizu, Itakura, Shortridge, Kawaoka and Webster1994). Before 1998, cH1N1 was the predominant subtype that caused most influenza infection in swine and had a predictable pattern similar to human influenza with high prevalence in late fall and early winter (Easterday and Van Reeth, Reference Easterday, Van Reeth, Straw, D'Allaire, Mengling and Taylor2007). In 1998, an influenza outbreak in swine herds occurred in several US states.
The causative subtype was identified as H3N2 (Vincent et al., Reference Vincent, Ma, Lager, Janke and Richt2008a), a triple reassortant of gene segments from human-like H3N2 HA, NA, PB1 genes, avian-like PB2 and PA genes and cH1N1-like NS, NP, and M genes (Zhou et al., Reference Zhou, Senne, Landgraf, Swenson, Erickson, Rossow, Liu, Yoon, Krauss and Webster1999; Webby et al., Reference Webby, Swenson, Krauss, Gerrish, Goyal and Webster2000). With time, triple reassortant H3N2 mutated and reassorted with cH1N1 to form new genotypes including new clusters of H3N2, H1N2 (HA from cH1N1 and other segments from H3N2), H3N1 and reassortant H1N1 (rH1N1, HA and NA from cH1N1 and other segments from H3N2) (Choi et al., Reference Choi, Goyal, Farnham and Joo2002; Richt et al., Reference Richt, Lager, Janke, Woods, Webster and Webby2003; Webby et al., Reference Webby, Rossow, Erickson, Sims and Webster2004). Reassortment of H3N2 with HA and NA from human virus lineages H1N1 and H1N2 form huH1N1 and huH1N2 has been reported as spreading in US swine herds (Vincent et al., Reference Vincent, Ma, Lager, Gramer, Richt and Janke2009; Lorusso et al., Reference Lorusso, Vincent, Harland, Alt, Bayles, Swenson, Gramer, Russell, Smith, Lager and Lewis2011). Within the H3N2 subtype, there are four phylogenetic clusters of H3N2 strain: I, II, III and IV (Richt et al., Reference Richt, Lager, Janke, Woods, Webster and Webby2003; Olsen et al., Reference Olsen, Karasin, Carman, Li, Bastien, Ojkic, Alves, Charbonneau, Henning, Low, Burton and Broukhanski2006; Hause et al., Reference Hause, Oleson, Bey, Stine and Simonson2010). Four phylogenetic clusters of swine H1 subtype have been identified in America: α (cH1N1), β (rH1N1), δ (huH1N1, huH1N2) and γ (H1N2), other than pandemic H1N1 (pH1N1) which forms clusters separated from North American viruses; cluster δ can be differentiated into two subclusters, δ1 (huH1N2) and δ2 (huH1N1) (Lorusso et al., Reference Lorusso, Vincent, Harland, Alt, Bayles, Swenson, Gramer, Russell, Smith, Lager and Lewis2011).
Reassortment of MA and NA genes from Eurasian IAV with North American triple reassortant virus resulted in pH1N1, which caused disease in both humans and swine in 2009 (Garten et al., Reference Garten, Davis, Russell, Shu, Lindstrom, Balish, Sessions, Xu, Skepner, Deyde, Okomo-Adhiambo, Gubareva, Barnes, Smith, Emery, Hillman, Rivailler, Smagala, Graaf, Burke, Fouchier, Pappas, Alpuche-Aranda, López-Gatell, Olivera, López, Myers, Faix, Blair, Yu, Keene, Dotson, Boxrud, Sambol, Abid, George, Bannerman, Moore, Stringer, Blevins, Demmler-Harrison, Ginsberg, Kriner, Waterman, Smole, Guevara, Belongia, Clark, Beatrice, Donis, Katz, Finelli, Bridges, Shaw, Jernigan, Uyeki, Smith, Klimov and Cox2009; Moreno et al., Reference Moreno, Di Trani, Alborali, Vaccari, Barbieri, Falcone, Sozzi, Puzelli, Ferri and Cordioli2010). Further reassortment of H3N2 and pH1N1, which is termed as rH3N2p, resulting in new IAV strains has been reported in 2010 (Tremblay et al., Reference Tremblay, Allard, Doyon, Bellehumeur, Spearman, Harel and Gagnon2011). rH3N2p contains up to five gene segments derived from pH1N1 (Kitikoon et al., Reference Kitikoon, Vincent, Gauger, Schlink, Bayles, Gramer, Darnell, Webby, Lager, Swenson and Klimov2012; Liu et al., Reference Liu, Ma, Liu, Qi, Anderson, Henry, Hesse, Richt and Ma2012). H3N2 variant (H3N2v), which resulted from the reassortment of H3N2 and M gene of pH1N1, has been circulating in U.S. pig herds since 2010 and human infection has been reported (CDC, 2012; Nelson et al., Reference Nelson, Vincent, Kitikoon, Holmes and Gramer2012). This strain appears to spread more easily from pig to human, rather than from human-to-human and to infect humans associated with exposure to pig outbreaks since July 2012 (CDC, 2012).
It has been reported that pigs were infected by avian influenza virus H4N6 subtype in 1999, but this infection did not spread in swine herds (Karasin et al., Reference Karasin, Brown, Carman and Olsen2000). Therefore, surveillance of emerging influenza subtype in pigs is critical to prevent and control influenza outbreaks in swine, and possibly humans.
The main subtypes of IAV circulating in North American swine are H1N1, H1N2 and H3N2 Cluster IV (Richt et al., Reference Richt, Lager, Janke, Woods, Webster and Webby2003; Vincent et al., Reference Vincent, Ma, Lager, Gramer, Richt and Janke2009; Kumar et al., Reference Kumar, Deflube, Biswas, Shobana and Elankumaran2011). According to the data from 2001 to 2007 from the University of Minnesota Veterinary Diagnostic Laboratory, among H1 subtypes, cluster α has been replaced with clusters β, δ and γ, and among H3N2 subtypes, cluster IV became dominant (Rapp-Gabrielson et al., Reference Rapp-Gabrielson, Sornsen, Nitzel, Wicklund, Wood, Kuhn and Gramer2008). Data from the University of Minnesota Veterinary Diagnostic Laboratory also indicate that of all IAV isolates from swine in 2010, 27.8% were H3N2 cluster IV, 22.4% were pH1N1, 18% were huH1N2 δ1, 9% were huH1N1 δ2, 15.7% were H1N1γ and the percentage of isolates belonging to α, β and other H3N2 clusters was less than 10% (Pfizer Inc., 2012). Influenza viruses of different clusters are antigenically divergent (Lorusso et al., Reference Lorusso, Vincent, Harland, Alt, Bayles, Swenson, Gramer, Russell, Smith, Lager and Lewis2011). Serologically, there is HA antibody-antigen cross-reactivity between classical H1 and reassorant H1 cluster β and H1 cluster γ, but limited cross-reactivity among cluster β, γ and δ or within δ clusters (Vincent et al., Reference Vincent, Lager, Ma, Lekcharoensuk, Gramer, Loiacono and Richt2006, Reference Vincent, Ma, Lager, Janke and Richt2008a, Reference Vincent, Ma, Lager, Gramer, Richt and Janke2009; Lorusso et al., Reference Lorusso, Vincent, Harland, Alt, Bayles, Swenson, Gramer, Russell, Smith, Lager and Lewis2011). For H3N2 IAV, clusters I and III, but not II, have HA antibody-antigen cross-reactivity between each cluster, and good reactivity within each cluster (Richt et al., Reference Richt, Lager, Janke, Woods, Webster and Webby2003).
The limited cross-reactivity of HA antibodies to HA antigens between different subtypes and clusters is one of the obstacles to development of vaccines to prevent all IAV viruses infecting swine. Pathogenicity, transmission, genetic and antigenic properties of a human H3N2v isolate and a swine rH3N2p isolate have been studied in pigs (Kitikoon et al., Reference Kitikoon, Vincent, Gauger, Schlink, Bayles, Gramer, Darnell, Webby, Lager, Swenson and Klimov2012). Phylogenetically, rH3N2p HA is closely related to cluster IV of H3N2 subtype (Kitikoon et al., Reference Kitikoon, Vincent, Gauger, Schlink, Bayles, Gramer, Darnell, Webby, Lager, Swenson and Klimov2012). Antibodies against cluster IV H3N2-TRIG and rH3N2p had reduced cross-reactivity with H3N2v (Kitikoon et al., Reference Kitikoon, Vincent, Gauger, Schlink, Bayles, Gramer, Darnell, Webby, Lager, Swenson and Klimov2012), but more information on antibody cross-activity against rH3N2p is needed. Currently, available commercial vaccines are prepared with H3N1-TRIG whole virus (inactivated) or the HA gene in RNA particle (RP) vaccines from H3N2-TRIG isolates. Challenge studies with these vaccines should be conducted to evaluate protection against rH3N2p strains.
In Europe, there are three circulating IAV subtypes (H1N1, H3N2 and H1N2), which are genetically different from cH1N1 and triple reassortant H3N2 in North America (Brown, Reference Brown2000; Kyriakis et al., Reference Kyriakis, De Vleeschauwer, Barbe, Bublot and Van Reeth2009). The predominating H1N1 IAV of Europe is known as ‘avian-like’, since genetic material from an avian genome was introduced into H1N1 IAV in 1979. Reassortment of HA and NA of ‘Hong Kong flu’ H3N2 and internal genes of avian-like H1N1 form the current human-like H3N2 subtype in Europe (Harkness et al., Reference Harkness, Schild, Lamont and Brand1972). H1N2 originated from H3N2 by acquiring HA from human-like H1N1 or avian-like H1N1 and NA from swine H3N2 (Brown et al., Reference Brown, Harris, McCauley and Alexander1998; Hjulsager et al., Reference Hjulsager, Bragstad, Bøtner, Nielsen, Vigre, Enøe and Larsen2006). These three subtypes have given rise to further reassortment strains including pH1N1 (Zell et al., Reference Zell, Scholtissek and Ludwig2012).
Immune responses to influenza infection in swine
Influenza virus infection induces both cellular and humoral immune responses. Soluble effectors including cytokines are secreted as a part of the innate immune response to IAV infection. Pro-inflammatory cytokines, including interferon α (IFN-α), tumor necrosis factor α (TNFα) and interleukin-1 (IL-1), are secreted in the lung in association with virus titers in pigs infected by IAV (Van Reeth, Reference Van Reeth2000). Cell-mediated immune responses participate in protecting swine from IAV infection. Proliferation of cross-reactive memory T-cells was detected in IAV recovered pigs that were free of maternal antibodies during infection, but not those with maternal antibodies present during infection (Kitikoon et al., Reference Kitikoon, Nilubol, Erickson, Janke, Hoover, Sornsen and Thacker2006). IAV infected pigs with reactive memory T-cells recovered faster than those without such memory T-cells, so these cells in pigs may participate in rapid recovery from IAV infection (Kitikoon et al., Reference Kitikoon, Nilubol, Erickson, Janke, Hoover, Sornsen and Thacker2006).
In adaptive humoral immunity, systemic and mucosal immune responses are induced following IAV infection, both of which are essential for the prevention and recovery from IAV infection (Cox et al., Reference Cox, Brokstad and Ogra2004). IAV-specific IgG and IgA antibodies are believed to significantly contribute to virus clearance. Antibodies against HA are the most important in preventing infection, although antibodies against NA contribute as well (Ma and Richt, Reference Ma and Richt2010). Testing HI antibody titers in serum has been used widely to predict humoral immune response and protection against IAV infection because vaccinated pigs are protected from IAV infection by high HI antibody titers (Larsen et al., Reference Larsen, Karasin, Zuckermann and Olsen2000; Vander Veen et al., Reference Vander Veen, Kamrud, Mogler, Loynachan, McVicker, Berglund, Owens, Timberlake, Lewis, Smith and Harris2009). Furthermore, testing serum HI titers for different IAV virus subtypes can predict cross-protection efficacy. Given IAV targets mucosal cells in the respiratory tract, antibodies need to be transported to mucosal sites. Short-lived serum IgG antibodies and more durable local IgA antibodies occur in pigs recovering from influenza infection or when vaccinated via a mucosal route. Pigs were protected from a subsequent IAV challenge (Charley et al., Reference Charley, Riffault and Van Reeth2006).
Swine influenza vaccines
Vaccination can be an effective way to decrease IAV infection, gross lesions of pneumonia, and economic losses due to influenza virus. Vincent et al. (Reference Vincent, Ma, Lager, Janke and Richt2008a) noted that ‘There are three major problems with the control and prevention of SI in the U.S.: (a) SIV is changing faster than traditional vaccines can be developed, (b) There is a need for vaccines that can induce better cross protection among SIV isolates, and (c) Passively acquired immunity is believed to block vaccine efficacy in pigs’.
A similar point of view was expressed in another publication (Ma and Richt, Reference Ma and Richt2010). Different types of IAV vaccine and strategies have been developed in order to address the problems associated with influenza vaccination in swine (Table 1). Commercial inactivated IAV vaccine for swine use became available in 1994 (Vincent et al., Reference Vincent, Ma, Lager, Janke and Richt2008a; Platt et al., Reference Platt, Vincent, Gauger, Loving, Zanella, Lager, Kehrli, Kimura and Roth2011). Inactivated whole virus IAV vaccines were the only commercially available vaccine used worldwide in swine herds (Ma and Richt, Reference Ma and Richt2010). However, Swine Influenza Vaccine, RNA (an RP vaccine expressing HA protein of H3N2 subtype) has recently been approved as a commercial vaccine in the U.S. (USDA, 2012a).
Table 1. Summary of characteristics of different types of influenza vaccines and vaccine candidates for swine use
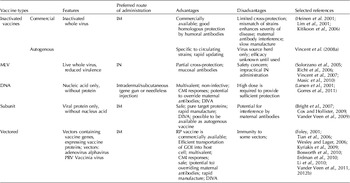
CMI, cell-mediated immunity; DIVA, differentiate infected from vaccinated animals; GOI, gene of interest; RP, RNA particle.
Inactivated virus vaccines
Although inactivated whole virus IAV vaccines protect pigs fully against homologous IAV challenge, they only partially protect pigs against heterologous challenge (Vincent et al., Reference Vincent, Ciacci-Zanella, Lorusso, Gauger, Zanella, Kehrli, Janke and Lager2010a, Reference Vincent, Lager, Faaberg, Harland, Zanella, Ciacci-Zanella, Kehrli, Janke and Klimovb).
Embryonated hen's eggs are generally used to propagate live virus for manufacturing inactivated IAV (Gorres et al., Reference Gorres, Lager, Kong, Royals, Todd, Vincent, Wei, Loving, Zanella, Janke, Kehrli, Nabel and Rao2011). Live virus is harvested from the eggs and killed with chemical treatment (Sanofi Pasteur, 2009). Since frequent antigenic shift and drift of IAV occurs and older vaccines may not protect against infection with the current circulating viruses, regulatory procedure for updating IAV strains in United States Department of Agriculture (USDA)-licensed veterinary vaccines is possible (Rapp-Gabrielson et al., Reference Rapp-Gabrielson, Sornsen, Nitzel, Wicklund, Wood, Kuhn and Gramer2008). It currently takes at least 1 year to update a commercial IAV vaccine (D. L. Harris, Iowa State University, personal communication). The procedure for changing virus strains in vaccines is based on the demonstration of efficacy and safety (Rapp-Gabrielson et al., Reference Rapp-Gabrielson, Sornsen, Nitzel, Wicklund, Wood, Kuhn and Gramer2008).
The most common vaccination route for influenza vaccines is intramuscular (IM) injection. IM vaccination induces a high level of specific IgG antibody in serum and lung but the antibody lacks cross protection against other virus strains of different subtypes (Heinen et al., Reference Heinen, Van Nieuwstadt, de Boer-Luijtze and Bianchi2001). Immune responses of pigs, naturally immunized by virus (A/Sw/Oedenrode/96 H3N2) infection or immunized by inactivated vaccine (A/Port Chalmers/1/73 H3N2, antigenically different from A/Sw/Oedenrode/96 H3N2) were compared following post A/Sw/Oedenrode/96 challenge by Heinen et al. (Reference Heinen, Van Nieuwstadt, de Boer-Luijtze and Bianchi2001). The results showed that serum HI antibody titers, virus neutralizing antibody titers and NP-specific IgG antibody titers developed by vaccinated pigs were similar or higher than those in naturally immune pigs. However, vaccinated pigs developed lower nasal IgA titers and lower cell-mediated immune responses than did naturally immune pigs (Heinen et al., Reference Heinen, Van Nieuwstadt, de Boer-Luijtze and Bianchi2001). Protection by this A/Port Chalmers/1/73 derived vaccine against A/Sw/Oedenrode/96 challenge was sub-optimal, because virus shedding was detected for a short period in vaccinated pigs compared with no virus shedding from naturally immune pigs (Heinen et al., Reference Heinen, Van Nieuwstadt, de Boer-Luijtze and Bianchi2001). The result of this study indicated the limited cross-protection induced by inactivated IAV vaccine to heterologous challenge. This is the major problem in development of swine influenza vaccines. Vaccine strain mismatch with circulating strains may even enhance the severity of disease (Vincent et al., Reference Vincent, Lager, Janke, Gramer and Richt2008b; Gauger et al., Reference Gauger, Vincent, Loving, Lager, Janke, Kehrli and Roth2011). Therefore, HA antigenic match of the vaccine strain and challenge strain is the key to providing protection by inactivated IAV vaccine. Inactivated commercial vaccines are often bivalent or trivalent, containing several circulating strains to increase the chances of matching the challenge viruses. For example, Flusure XP (Pfizer, Inc., New York, NY USA), which is an IAV vaccine for swine, contains up to four swine influenza virus strains to provide protection against a range of virus strains (Lee et al., Reference Lee, Gramer and Joo2007; Pfizer Inc., 2011). However, it is difficult to cover all strains in a single dose of vaccine and manufacturing cost rises with increasing numbers of IAV strains in vaccines.
Another problem encountered in IAV vaccination is the interference of maternal antibodies in piglets. Anti-influenza serum IgG is transferred to piglets from maternal antibodies in sow's colostrum. If sows are vaccinated with an IAV vaccine before farrowing, a significant level of IAV maternal antibodies (>40-fold in HI) can be detected in suckling piglets up to 14 weeks of age (Markowska-Daniel et al., Reference Markowska-Daniel, Pomorska-Mol and Pejsak2011). Swine influenza virus maternal antibodies are important for protecting young piglets but can be the cause of immunization failure (Wesley and Lager, Reference Wesley and Lager2006). Pigs vaccinated with commercial bivalent vaccine had better partial protection facing heterologous H1 challenge when maternal antibodies were absent than when maternal antibodies were present (Kitikoon et al., Reference Kitikoon, Nilubol, Erickson, Janke, Hoover, Sornsen and Thacker2006). It has been shown that IAV-specific humoral responses and cellular responses in vaccinated pigs have both been suppressed in the presence of maternal antibodies (Kitikoon et al., Reference Kitikoon, Nilubol, Erickson, Janke, Hoover, Sornsen and Thacker2006).
Mucosal responses, including IgA antibodies and cellular responses, have been the focus of much study to attempt to provide wider cross-protection and override maternal antibodies. Intranasal (IN) administration of IAV vaccines has been attempted as an alternative method to protect pigs and induce local immune responses (Lim et al., Reference Lim, Takada, Tanizaki, Ozaki, Okazaki and Kida2001). Four doses in consecutive weeks of IN vaccination with inactivated influenza vaccine provided complete protection to pigs from homologous challenge, and IgG and IgA were detected in mucosal secretions and serum (Lim et al., Reference Lim, Takada, Tanizaki, Ozaki, Okazaki and Kida2001). IgG antibodies were detected after the second vaccination, while IgA antibodies were detected following the fourth vaccination (Lim et al., Reference Lim, Takada, Tanizaki, Ozaki, Okazaki and Kida2001). The efficacy of mucosal administration of inactivated influenza vaccine to override the interference of maternal antibodies in piglets needs further evaluation. Four doses of vaccine are not convenient for practical vaccination on pig farms, and four doses may not be economically feasible. It would be helpful to determine the reason(s) that IgG induction requires fewer doses than mucosal IgA induction by inactivated vaccine in order to improve IN vaccine development.
Romagosa et al. (Reference Romagosa, Allerson, Gramer, Joo, Deen, Detmer and Torremorell2011) have shown that both inactivated commercial heterologous vaccine and inactivated autogenous homologous vaccine were able to reduce transmission of IAV. As a critical property of a vaccine, the extent of reduction in IAV transmission needs to be evaluated in other types of IAV vaccine in pigs. More information on whether IAV vaccine is able to shorten the infectious period, or decrease the reproductive ratio (‘the number of secondary infections caused by an infectious individual’) (Romagosa et al., Reference Romagosa, Allerson, Gramer, Joo, Deen, Detmer and Torremorell2011) also needs to be generated.
Live attenuated vaccines
Recombinant modified influenza viruses can be obtained with reverse genetics technology and provide a novel way to make modified live-attenuated virus (MLV) vaccines. HA0 protein, the precursor of HA, must be cleaved into HA1 and HA2 in order to fuse with endosomal membranes (Skehel and Wiley, Reference Skehel and Wiley2000). HA0 modified live-attenuated virus (Δha0MLV) was achieved by introducing a mutation to the HA cleavage site (Stech et al., Reference Stech, Garn, Wegmann, Wagner and Klenk2005; Gabriel et al., Reference Gabriel, Garn, Wegmann, Renz, Herwig, Klenk and Stech2008; Masic et al., Reference Masic, Lu, Li, Mutwiri, Babiuk, Brown and Zhou2010). Masic et al. (Reference Masic, Babiuk and Zhou2009) showed that Δha0MLV could infect pigs without live virus being shed, proving that Δha0MLV is attenuated in pigs. The H1N1 strain of Δha0MLV administrated IN induced a significant cross protection to H1N1 and H3N2 challenge. Both macroscopic and histopathologic lung lesion scores were significantly reduced in both homologous challenge and heterologous challenge groups (Masic et al., Reference Masic, Lu, Li, Mutwiri, Babiuk, Brown and Zhou2010). Virus shedding was not detected in 5/6 pigs from homologous H1 strain challenge and in 3/6 pigs from heterologous H3N2 challenge (Masic et al., Reference Masic, Lu, Li, Mutwiri, Babiuk, Brown and Zhou2010). Vaccinated pigs had considerable IgA in the lower respiratory tract and IgG in serum after either homologous or heterologous challenge (Masic et al., Reference Masic, Lu, Li, Mutwiri, Babiuk, Brown and Zhou2010). Two dose vaccinations were required to induce protection with Δha0MLV (Masic et al., Reference Masic, Lu, Li, Mutwiri, Babiuk, Brown and Zhou2010).
NS1 of swine influenza virus has been shown to be a virulence factor with the function of antagonizing type I interferon (IFN-α/β) (Talon et al., Reference Talon, Salvatore, O'Neill, Nakaya, Zheng, Muster, Garcia-Sastre and Palese2000). Introducing mutations into the gene encoding the NS1 protein causes the loss of IFN-α/β inhibiting potency (Talon et al., Reference Talon, Salvatore, O'Neill, Nakaya, Zheng, Muster, Garcia-Sastre and Palese2000; Solorzano et al., Reference Solorzano, Webby, Lager, Janke, Garcia-Sastre and Richt2005). A NS1 modified influenza strain (Sw/TX/98Δ126) has been shown to be virulence attenuated in inoculated pigs in which lung lesions were reduced and live virus shedding was reduced (Solorzano et al., Reference Solorzano, Webby, Lager, Janke, Garcia-Sastre and Richt2005). Induction of HI antibodies by this Δns1MLV indicated it was immunogenic (Solorzano et al., Reference Solorzano, Webby, Lager, Janke, Garcia-Sastre and Richt2005). To test the efficacy of Δns1MLV as an influenza vaccine candidate, pigs were vaccinated twice intratracheally with Δns1MLV, then challenged with the homologous virus or a heterologous virus. Pigs challenged with the homologous virus were completely protected by Δns1MLV and the virus was confirmed to be attenuated (Richt et al., Reference Richt, Lekcharoensuk, Lager, Vincent, Loiacono, Janke, Wu, Yoon, Webby, Solorzano and Garcia-Sastre2006). In heterologous subtype challenge with a cH1N1 strain, macroscopic lung lesion scores in vaccinated pigs and unvaccinated pigs were similar, while microscopic lung lesion scores and virus shedding in respiratory tract were reduced compared with the unvaccinated group (Richt et al., Reference Richt, Lekcharoensuk, Lager, Vincent, Loiacono, Janke, Wu, Yoon, Webby, Solorzano and Garcia-Sastre2006).
In another study, two doses of IN Δns1MLV vaccine were administered in an attempt to evaluate the efficacy of heterologous protection. Attenuated live influenza virus with truncated NS1 (TX98 H3N2) was administrated IN by dripping the vaccine into the nares to evaluate homologous and heterologous protection. CO99 H3N2 (antigenic variant from TX98) and IA04 (H1N1) were the heterologous strains that were evaluated (Vincent et al., Reference Vincent, Ma, Lager, Janke, Webby, Garcia-Sastre and Richt2007). The results demonstrated that IN administration of Δns1MLV (TX98) significantly reduced rectal temperature, and live virus shedding and lung lesions following challenge with TX98 (cluster I) and CO99 (cluster II) (Gramer et al., Reference Gramer, Lee, Choi, Goyal and Joo2007; Vincent et al., Reference Vincent, Ma, Lager, Janke, Webby, Garcia-Sastre and Richt2007). Modest levels of HI antibodies specific to TX98, but not CO99 or IA04 were detected in serum, and robust IgA and IgG antibodies with cross-reactivity to CO99 were detected in the mucosa (Vincent et al., Reference Vincent, Ma, Lager, Janke, Webby, Garcia-Sastre and Richt2007). The cross-reactive local antibodies induced by IN Δns1MLV vaccination indicate the potential for induction of universal protection by IN vaccination. In addition, modest HI antibodies in serum indicate the potential to reduce IAV antibodies from sows to piglets through colostrum.
MLV vaccines have not been approved for use in pigs. Cold-adapted MLV has been approved in the US for human (FluMist) and equine (FluAvert) use via the IN route (Belshe, Reference Belshe2004; Paillot et al., Reference Paillot, Hannant, Kydd and Daly2006). Cold-adapted MLV is achieved by inducing combination mutations in genes encoding PB1 and PB2 proteins of IAV, which cause virus replication to be temperature sensitive (Solorzano et al., Reference Solorzano, Webby, Lager, Janke, Garcia-Sastre and Richt2005). The FluMist vaccine strain is not only a cold adapted virus but also a reassorted virus strain. It contains six segments (PB1, PB2, NP, M, PA and NS) from human H2N2 (A/Ann Arbor/6/60) that contribute to virus attenuation and two segments encoding HA and NA proteins from circulating wild-type influenza virus (Chan et al., Reference Chan, Zhou, Kemble and Jin2008).
Safety is a major concern regarding the use of attenuated live virus as a vaccine. Given genome segments are able to reassort, there is concern that modified live vaccines will reassort with wild-type strains in the field to produce novel virulent influenza strains. The reassortment of viral strain and vaccine strain requires the replication of both genomes within a single cell at the same time. In all the vaccines studies above, live virus was not recovered from the upper respiratory tract or the lung after vaccination. Whether there was live virus in the lung before challenge was not examined. Another concern is that MLVs may revert to virulence over time if natural mutations occur (Babiuk et al., Reference Babiuk, Masic, Graham, Neufeld, van der Loop, Copps, Berhane, Pasick, Potter, Babiuk, Weingartl and Zhou2011).
The route of administration is another concern for the use of MLV in pigs. To induce local antibodies in respiratory mucosa, MLV normally requires IN administration. Commercial IN influenza vaccine for humans or horses is administrated in the form of a mist. The narrow space in the swine nasal cavity results in low efficiency of delivery of a mist deeply into the respiratory tract. Dripping vaccine into the nose, which is only commonly performed in an experimental setting, is time consuming and not likely to be efficient in a commercial farm setting.
DNA vaccines
Recombinant DNAs coding IAV proteins have been evaluated as vaccine candidates for swine. The era of gene vaccines was started by Wolff et al. in 1990. They demonstrated that protein can be expressed upon direct inoculation of plasmid DNA into mouse muscle (Wolff et al., Reference Wolff, Malone, Williams, Chong, Acsadi, Jani and Felgner1990). The advantages of DNA vaccination are: (i) one recombinant DNA molecule can encode multiple genes of interest, thereby reducing manufacturing cost; (ii) DNA vaccines do not carry infection risks associated with MLV vaccines; (iii) recombinant DNA can express high levels of proteins of interest in cells; (iv) DNA vaccines have the capacity to induce both humoral and cellular immune responses; (v) there is potential for DNA vaccines to override maternal antibodies which mainly recognize IAV surface proteins but not genomes (Dhama et al., Reference Dhama, Mahendran, Gupta and Rai2008); (vi) there is the capacity to differentiate infected from vaccinated animals (DIVA), because the DNA vaccine does not express all the proteins of the pathogens, and will induce different immune responses than those which occur in naturally infected animals. The barrier to developing efficacious DNA vaccines is low DNA transportation efficiency into target cells using a traditional IM vaccination route (Pertmer et al., Reference Pertmer, Eisenbraun, McCabe, Prayaga, Fuller and Haynes1995; Olsen, Reference Olsen2000; Dhama et al., Reference Dhama, Mahendran, Gupta and Rai2008).
Gene gun delivery has been shown to enhance the efficiency of DNA transfection by Olsen and colleagues in 2000. Two doses of gene gun administration of HA DNA vaccine to either pig skin or tongue resulted in high levels of HI antibodies after virus challenge; however, virus shedding was not completely prevented even with the co-administration of porcine interleukin-6 (Olsen, Reference Olsen2000; Larsen et al., Reference Larsen, Karasin and Olsen2001). This type of DNA vaccine immunization strategy may prime the pig immune system (Olsen, Reference Olsen2000; Larsen et al., Reference Larsen, Karasin and Olsen2001; Larsen and Olsen, Reference Larsen and Olsen2002). Gene gun delivered DNA vaccine as prime and inactivated commercial vaccine as boost was found to reduce viral shedding to an extent similar to that of a two-dose inactivated commercial vaccination strategy (Larsen et al., Reference Larsen, Karasin and Olsen2001).
Gorres et al. (Reference Gorres, Lager, Kong, Royals, Todd, Vincent, Wei, Loving, Zanella, Janke, Kehrli, Nabel and Rao2011) designed an IAV DNA vaccine by constructing a backbone with cytomegalovirus enhancer/promoter and the human T-cell leukemia virus type 1 R region recombined with trivalent HA genes (cH1N1, H3N2 and pH1N1) or monovalent HA gene (pH1N1). Using three doses of IM or needle-free (NF) for 0.5-ml subcutaneous vaccination of pigs, similar levels of HI antibodies to vaccine strain virus and cellular immune responses were induced in both trivalent and monovalent vaccine groups with both IM and NF methods (Gorres et al., Reference Gorres, Lager, Kong, Royals, Todd, Vincent, Wei, Loving, Zanella, Janke, Kehrli, Nabel and Rao2011). After H1 challenge, only IM and NF monovalent DNA vaccination reduced virus shedding at 3 days post challenge (dpc) and both NF trivalent and monovalent DNA vaccination completely protected against virus shedding at 5 dpc (Gorres et al., Reference Gorres, Lager, Kong, Royals, Todd, Vincent, Wei, Loving, Zanella, Janke, Kehrli, Nabel and Rao2011). Post H3 challenge, both IM and NF trivalent DNA vaccination reduced virus shedding at 3 dpc and fully prevented virus shedding on 5 dpc. Minimal lung lesions were observed in vaccinated pigs that were examined (Gorres et al., Reference Gorres, Lager, Kong, Royals, Todd, Vincent, Wei, Loving, Zanella, Janke, Kehrli, Nabel and Rao2011).
Nanoparticles such as chitosan have been tested as IAV DNA vaccine adjuvants for sustained release of vaccine; however, low transfection efficiency of the chitosan-DNA vaccine is a disadvantage of this approach (Zhao et al., Reference Zhao, Shi, Zhao, Wei, Sun, Huang, Zhang and Wang2011). There remains a need for identification of a more efficient method to deliver DNA vaccines in order to better evaluate this vaccination approach. So far, a high dose of DNA vaccine has been required for vaccination, which is expensive and not practical.
Subunit IAV vaccines
A subunit vaccine is an immunizing agent containing viral proteins, but no viral nucleic acid (Myers, Reference Myers and Myers2010). Subunit vaccines can contain higher concentrations of specific proteins than inactivated vaccines (Cox and Hollister, Reference Cox and Hollister2009). The major component of subunit swine influenza vaccine is one or more than one recombinant IAV protein, the viral structural proteins that are not present in subunit vaccines or the antibodies against them can be detected to differentiate infected from vaccinated animals. Thus subunit vaccines have the potential to be DIVA. IAV structural protein HA is expressed in subunit influenza vaccines as it is able to induce HI antibodies (Cox and Hollister, Reference Cox and Hollister2009; Vander Veen et al., Reference Vander Veen, Kamrud, Mogler, Loynachan, McVicker, Berglund, Owens, Timberlake, Lewis, Smith and Harris2009; Shoji et al., Reference Shoji, Chichester, Jones, Manceva, Damon, Mett, Musiychuk, Bi, Farrance, Shamloul, Kushnir, Sharma and Yusibov2011). Employing DNA recombinant technology, IAV proteins can be expressed in other platforms (Bachrach, Reference Bachrach1982). Several platforms have been developed to express IAV subunits to replace traditional egg-based vaccine manufacturing.
A baculovirus expression system was used to produce influenza virus HA protein in insect cells as a vaccine to induce protection against influenza infection in humans (Cox and Hollister, Reference Cox and Hollister2009). Trivalent recombinant HAs, a combination of HAs derived from influenza A subtypes H1N1, H3N2 and influenza B are present in a vaccine to achieve cross protection (Cox and Hollister, Reference Cox and Hollister2009). In another method, HA, NA and M1 proteins of influenza virus expressed individually by baculovirus-insect platform self-assemble into high molecular-weight enveloped influenza virus-like particles (VLPs) (Bright et al., Reference Bright, Carter, Daniluk, Toapanta, Ahmad, Gavrilov, Massare, Pushko, Mytle, Rowe, Smith and Ross2007). The capacity of such VLPs to induce cellular and humoral immune responses has been demonstrated in preclinical trials (Bright et al., Reference Bright, Carter, Daniluk, Toapanta, Ahmad, Gavrilov, Massare, Pushko, Mytle, Rowe, Smith and Ross2007). Nicotiana benthamiana, a close relative of the tobacco plant, was also developed as a subunit expressing platform, in which H5N1 HA protein formed H5 VLPs (D'Aoust et al., Reference D'Aoust, Lavoie, Couture, Trepanier, Guay, Dargis, Mongrand, Landry, Ward and Vezina2008). Cross-reactive antibodies to influenza H5 VLP were induced in a ferret model and a safety study in humans showed no significant induction of naturally occurring serum antibodies to plant-specific sugar moieties (Landry et al., Reference Landry, Ward, Trepanier, Montomoli, Dargis, Lapini and Vezina2010). Both of the above platforms are now employed to produce experimental influenza subunit vaccines for human use, and may be candidates for production of vaccines for swine use.
An alphavirus replicon RNA has also been employed to express IAV HA for swine vaccination (Vander Veen et al., Reference Vander Veen, Kamrud, Mogler, Loynachan, McVicker, Berglund, Owens, Timberlake, Lewis, Smith and Harris2009). There are two open reading frames (ORFs) in the alphavirus genome (Rayner et al., Reference Rayner, Dryga and Kamrud2002). All non-structural proteins responsible for replicating viral RNA are encoded in the first ORF (Rayner et al., Reference Rayner, Dryga and Kamrud2002). The second ORF of alphavirus normally encodes structural proteins that are responsible for the assembly of virus particles. An engineered virus genome, or replicon RNA, containing the alphavirus ORF1 combined with heterologous genes in ORF2 electroporated into VERO cells was able to express the heterologous proteins in high levels in the cultured cells (Rayner et al., Reference Rayner, Dryga and Kamrud2002). IAV HA protein expressed by the alphavirus replicon RNA platform in VERO cells was combined with adjuvant and tested as an IAV vaccine for swine (Vander Veen et al., Reference Vander Veen, Kamrud, Mogler, Loynachan, McVicker, Berglund, Owens, Timberlake, Lewis, Smith and Harris2009). This HA subunit IAV vaccine induced specific HI antibodies in vaccinated pigs and was efficacious in reducing virus shedding and gross and histopathologic lung lesions after homologous virus challenge (Vander Veen et al., Reference Vander Veen, Kamrud, Mogler, Loynachan, McVicker, Berglund, Owens, Timberlake, Lewis, Smith and Harris2009). These subunit vaccines made from alphavirus replicon RNA are free of the possibility of replicating virus, since no structural genes of the alphavirus are present (Vander Veen et al., Reference Vander Veen, Kamrud, Mogler, Loynachan, McVicker, Berglund, Owens, Timberlake, Lewis, Smith and Harris2009).
Vectored vaccines
Vectors are utilized to transport genes into cells. Vectored vaccines containing genomic material can express high levels of the encoded protein after cell entry. Vectors may be replicative or replication defective. Replication defective vectors have the ability to infect cells but lack essential genes for production of new virus particles. Thus, vectored vaccines need two essential features. The first is that the vectors are able to infect cells and transport the recombinant genome into cells. The second essential feature is that the recombinant genomes are able to replicate by themselves and express the gene of interest in high levels in infected cells. Since the genes of interest in a vectored vaccine are not all the genes of the target pathogen, vectored vaccines can be DIVA vaccines. A wide host range of the virus vector and lack of pre-existing antibodies in the target species are two other important features to be considered for good vector candidates. Besides transporting the gene that encodes the antigen into cells, vector particles are able to stimulate cellular immunity to the vaccine component, providing them with an advantage over subunit protein vaccines (Macklin et al., Reference Macklin, McCabe, McGregor, Neumann, Meyer, Callan, Hinshaw and Swain1998; Rayner et al., Reference Rayner, Dryga and Kamrud2002; Wesley et al., Reference Wesley, Tang and Lager2004). Also, because they are expressed within cells, vectored vaccine antigens have the potential to avoid interference from maternal antibodies. Another advantage is that a vector can express several genes encoding different antigens (Vander Veen et al., Reference Vander Veen, Harris and Kamrud2012a).
Human adenovirus serotype 5 (Ad5) has been examined as an IAV vector for pigs (Wesley and Lager, Reference Wesley and Lager2006). As the early transcription region 1 is deleted, Ad5 virus is replication-defective (Wesley et al., Reference Wesley, Tang and Lager2004). However, the recombinant gene of interest is able to be transcribed as it is under the control of constitutive promoters (Wesley et al., Reference Wesley, Tang and Lager2004). Pigs vaccinated with a 1-dose mixture of Ad5 expressing the IAV H3N2 HA gene (Ad5 HA) and Ad5 expressing the H3N2 NP gene (Ad5 NP) were completely protected from virus shedding and lung lesion development after homologous challenge. Pigs vaccinated with Ad5 HA shed low levels of virus and had low lung lesion scores which were not significantly different from that of Ad5 HA + Ad5 NP vaccinated pigs. Pigs vaccinated with Ad5 NP shed significantly lower levels of virus than unvaccinated pigs on 3 of 5 days after challenge (Wesley et al., Reference Wesley, Tang and Lager2004). Furthermore, Ad5 expressing IAV H3N2 HA and NP proteins (Ad5-HA&NP) was shown to be able to prime the immune response in the presence of maternal IAV antibodies in piglets (Wesley and Lager, Reference Wesley and Lager2006). Piglets receiving maternal antibodies from gilts were administrated Ad5-HA&NP as a priming IM vaccine when suckling milk containing IAV maternal antibodies from gilts and were boosted by an inactivated commercial vaccine (End-FLUence 2, Intervet Inc., Millsboro, Delaware) administered by the IM route. Sows had antibodies to IAV H3N2 strain and End-FLUence 2 comprising H1N1 and H3N2 strains. Piglets were then challenged with a heterologous IAV H3N2 strain after a booster vaccination. Better protection was induced in the pigs that received the priming vaccine compared with piglets without the A5-HA&NP priming vaccine (Wesley and Lager, Reference Wesley and Lager2006). After a single dose of an IN A5-HA vaccine, pigs were fully protected against homologous pH1N1 challenge, and partially protected against heterologous delta1 subtype challenge, indicated by limited reduction in the duration and amount of viral shedding; Vaccine associated enhanced respiratory disease was not observed in these pigs which received the heterologous challenged (Braucher et al., Reference Braucher, Henningson, Loving, Vincent, Kim, Steitz, Gambotto and Kehrli2012). A disadvantage of adenovirus vectors is the development of vector immunity (Pandey et al., Reference Pandey, Singh, Vemula, Couetil, Katz, Donis, Sambhara and Mittal2012). Pigs can only be primed with the adenovirus vector vaccine, the efficacy of a booster injection will be reduced by antibodies to the vector.
Alphavirus has also been developed as a vaccine vector based on an alphavirus replicon RNA. Since genes coding structural proteins of alphavirus are deleted in the alphavirus replicon RNA, new alphavirus particles cannot be produced. To make vaccine alphavirus particle vectors, alphavirus structural protein genes as helper RNAs are transported into cells in trans along with the replicon RNA during electroporation. Alphavirus-like particles, now known as either replicon particles or RP are formed subsequently (Rayner et al., Reference Rayner, Dryga and Kamrud2002; Vander Veen et al., Reference Vander Veen, Harris and Kamrud2012a).
The replication-deficient feature of RPs was achieved by several techniques: (1) dividing the structural protein genes into two elements (Pushko et al., Reference Pushko, Parker, Ludwig, Davis, Johnston and Smith1997; Smerdou and Liljestrom, Reference Smerdou and Liljestrom1999); (2) deleting the 26S promoters and a large portion of non-coding sequences in front of 26S including start codons and stop codons in each helper element (K.I. Kamrud, Harrisvaccines Inc., personal communication). There are several advantages of alphavirus RP which make it an attractive vaccine platform candidate. Firstly, vector safety has been proven as RPs are not shed or spread to cohorts or into the environment by vaccinated animals (Vander Veen et al., Reference Vander Veen, Loynachan, Mogler, Russell, Harris and Kamrud2012b). Secondly, anti-alphavirus vector immunity is minimal, thus the same animal can be vaccinated several times with RP vector-based vaccines. Thirdly, rapid development of a new vaccine is possible with the RP system (Vander Veen et al., Reference Vander Veen, Harris and Kamrud2012a). Within 6 weeks from receiving virus samples, an IAV subunit or RP vaccine can be prepared with the RP system (R.L. Vander Veen, Harrisvaccines Inc., personal communication). This feature of the RP system offers great potential for developing autogenous IAV vaccines. In addition, the RP vector has dendritic cell tropism, and can express multivalent genes of interest (Vander Veen et al., Reference Vander Veen, Harris and Kamrud2012a). As with other vectors, RP-based vaccines have the capacity to be DIVA, and are able to express high levels of heterologous genes.
Venezeulan equine encephalitis virus (VEEV), a member of the alphavirus family, was selected as an IAV vaccine vector expressing the HA protein. The VEEV has been shown to infect pigs, but only induces a transient viremia (Dickerma et al., Reference Dickerma, Baker, Ordonez and Scherer1973). Attenuated TC-83 VEEV strain, which is a biosafety level (BL) 2 pathogen, has been developed as an RP vector (Erdman et al., Reference Erdman, Kamrud, Harris and Smith2010). This makes manufacturing of RP-based vaccines easier and safer than using the original BL3 pathogenic 3014 VEEV strain. Pigs receiving two doses of RP vaccine expressing HA (HA RP) produced a high level of HI antibody from 7 days post booster vaccination and maintained this level for at least 40 days (Erdman et al., Reference Erdman, Kamrud, Harris and Smith2010). HA RP encoding the HA gene of cluster IV H3N2 or pH1N1 protected pigs from homologous IAV challenge in two other studies, thereby confirming the efficacy of the RP vaccine (Vander Veen, Reference Vander Veen2011, 2012b). In pigs vaccinated with HA RPs, HI antibodies and cell mediated immunity (CMI) were induced, live virus was not isolated from nasal swabs and BAL samples, and lung lesions were significantly reduced (Vander Veen et al., Reference Vander Veen, Loynachan, Mogler, Russell, Harris and Kamrud2012b). Mucosal antibodies specific to vaccine antigen were induced by adjuvanted alphavirus RP vaccine injected in the rear footpads in mice (Thompson et al., Reference Thompson, Nicholson, Whitmore, Zamora, West, Iwasaki, Staats and Johnston2008).
RPs encoding the NP gene homologous to that of the challenge virus were shown to reduce virus replication in pigs and to stimulate both humoral antibodies and CMI; the CMI responded to both homologous and heterologous IAV antigens in vitro (Vander Veen, Reference Vander Veen2011). Homologous NP RP itself did not protect pigs against homologous challenge as well as HA RP; NP RP along with HA RP has the potential to help piglets override maternal antibodies, which could be determined in a future study (Wesley and Lager, Reference Wesley and Lager2006; Vander Veen, Reference Vander Veen2011).
Pseudorabies virus (PRV), in the Alphaherpesvirinae subfamily of the Herpesviridae family, has been used as a vaccine vector to express IAV HA as well. PRV consists of a linear double-stranded DNA genome with a length of 143 kb (Klupp et al., Reference Klupp, Hengartner, Mettenleiter and Enquist2004). Several non-essential genes exist in the PRV genome, most of which can be deleted to reduce virulence and can be replaced by other genes without affecting virus replication (Tian et al., Reference Tian, Zhou, Zheng, Qiu, Ni, Yang, Yin, Hu and Tong2006). Based on these features, a commercial attenuated PRV DIVA vaccine was developed with gE deletion (Pensaert et al., Reference Pensaert, Labarque, Favoreel and Nauwynck2004). In addition, the attenuated PRV vaccine strain (Bartha-K61) was employed as an influenza vaccine vector expressing HA (Tian et al., Reference Tian, Zhou, Zheng, Qiu, Ni, Yang, Yin, Hu and Tong2006; Li et al., Reference Li, Zhou, Yu, Tian, Yan, Zhang, Hu and Tong2010). Recombinant PRV expressing H3N2 HA (rPRV-HA) protected mice against homologous virus challenge (Tian et al., Reference Tian, Zhou, Zheng, Qiu, Ni, Yang, Yin, Hu and Tong2006). In the rPRV-HA vaccinated group, live virus was not isolated from lung tissues from 4 dpc until the end of the study and lung lesions were mild (Tian et al., Reference Tian, Zhou, Zheng, Qiu, Ni, Yang, Yin, Hu and Tong2006). Since this PRV vector is not suitable to be used multiple times due to immunity to the vector, prime/boost immunization with DNA expressing soluble HA fused with three copies of murine complement C3d (HA/C3d DNA) and rPRV-HA was investigated (Li et al., Reference Li, Zhou, Yu, Tian, Yan, Zhang, Hu and Tong2010). This regimen induced better protection than a 1-dose vaccination with rPRV-HA in mice (Li et al., Reference Li, Zhou, Yu, Tian, Yan, Zhang, Hu and Tong2010). However, the protection provided to pigs by PRV vector influenza vaccine needs further evaluation. Attenuated PRV strain has a good safety record and broad host range (Klupp et al., Reference Klupp, Hengartner, Mettenleiter and Enquist2004; Yuan et al., Reference Yuan, Zhang, Liu, Zhang, Fooks, Li and Hu2008). These advantages further support PRV as an influenza vaccine vector candidate. However, immunity to the vector limits the PRV vector use with multiple doses. Furthermore, the use of attenuated PRV strain as a vector may interfere with the surveillance of PRV (Ma and Richt, Reference Ma and Richt2010). To ensure PRV-free status the use of a PRV vector that induces antibodies against PRV may be restricted in countries that are free of PRV.
Poxvirus vectored vaccines expressing HA are licensed for preventing influenza in equines and poultry (Kyriakis et al., Reference Kyriakis, De Vleeschauwer, Barbe, Bublot and Van Reeth2009). Modified vaccinia Ankara (MVA) is an attenuated vaccinia strain used widely to eradicate human smallpox (Rimmelzwaan and Sutter, Reference Rimmelzwaan and Sutter2009). The attenuation of MVA is created by continuous passages on primary chicken embryo fibroblast cells (Verheust et al., Reference Verheust, Goossens, Pauwels and Breyer2012). Recombinant MVA virus containing HA and NP genes of classical H1N1 IAV (A/Sw/IN/1726/88) or containing HA and NP genes of a human strain (A/PR/8/34) administered IN or IM to pigs was followed by challenge with homologous classical H1N1 IAV (Foley, Reference Foley2001). All vaccinations, except with A/PR/8/34 IM, resulted in a shortened virus shedding period and much lower virus titers in pigs (Foley, Reference Foley2001). MVA virus containing HA and NP genes of classical H1N1 IAV (A/Sw/IN/1726/88) administered IM or IN both reduced or completely prevented lung lesion development following homologous challenge (Foley, Reference Foley2001). These results indicate that MVA is competent as an influenza vaccine vector (Rimmelzwaan and Sutter, Reference Rimmelzwaan and Sutter2009). Other poxvirus vectors including a fowlpox vector (TROVAC® Merial, Duluth, Georgia, USA), a canarypox vector (ALVAC®, Sanofi Pasteur, Swiftwater, Pennsylvania, USA), and another vaccinia vector (NYVAC) were also shown to be safe and effective as HA protein vectors in pigs (Kyriakis et al., Reference Kyriakis, De Vleeschauwer, Barbe, Bublot and Van Reeth2009). All these vectors expressing H5N1 HA protein, when combined with an oil-in-water adjuvant, induced homologous HI antibodies in pigs and induced a cross-reactive immunity by inhibiting virus replication following a heterologous H5N2 influenza challenge (Kyriakis et al., Reference Kyriakis, De Vleeschauwer, Barbe, Bublot and Van Reeth2009). In addition, multiple doses of poxvirus vectored vaccines can be used in the same animal (Kyriakis et al., Reference Kyriakis, De Vleeschauwer, Barbe, Bublot and Van Reeth2009).
Autogenous vaccines
Autogenous vaccines are prepared from field virus strains, and normally are inactivated virus. In general, it takes 8–12 weeks to produce an inactivated autogenous vaccine (R.L. Vander Veen, Harrisvaccines Inc., personal communication). The use of autogenous vaccines has increased in recent years because of rapid mutation rates of IAV and the difficulty vaccine manufacturers have in updating their vaccine strains for commercial availability (Vincent et al., Reference Vincent, Ma, Lager, Janke and Richt2008a). An estimated $16.06 million in swine autogenous vaccines were sold in the US from May 1999 to April 2000 (Draayer, Reference Draayer2004). IAV and porcine reproductive and respiratory syndrome disease vaccines consisted of more than half of the autogenous vaccines produced (Draayer, Reference Draayer2004). In 2006, more than 20% of all known IAV-vaccinated breeding sows and more than 9% of IAV vaccinated nursery-age pigs were vaccinated with autogenous IAV vaccines (USDA, 2007). Up to 2010, around 50% of IAV vaccines used for swine in US markets were autogenous vaccines (Ma and Richt, 2010). Use of autogenous vaccines is only allowed under a veterinarian's direction in the herd from which the vaccine virus was recovered (Vincent et al., Reference Vincent, Ma, Lager, Janke and Richt2008a). Two to four different subtype viruses are typically contained within an autogenous vaccine mixture, but there can be up to five viruses. Efficacy of the vaccines is not evaluated when they are manufactured, but they may be monitored under a veterinarian's supervision at the time of use. Recently, the USDA Center for Veterinary Biologics (CVB) has notified vaccine manufacturers that recombinant non-living vaccines may be licensed as autogenous vaccines (USDA, 2012b). Autogenous vaccine production is normally achieved by inactivating live virus isolated from an infected herd and propagating the virus (Vincent et al., Reference Vincent, Ma, Lager, Janke and Richt2008a). The virus replication efficiency of different strains varies, especially for new emerging strains, and the propagation characteristics may be unknown. For example, propagating H17N10 strain in cell culture or embryo eggs has not been successful so far (Tong et al., Reference Tong, Li, Rivailler, Conrardy, Castillo, Chen, Recuenco, Ellison, Davis, York, Turmelle, Moran, Rogers, Shi, Tao, Weil, Tang, Rowe, Sammons, Xu, Frace, Lindblade, Cox, Anderson, Rupprecht and Donis2012). Such unpredictable factors may delay the production of inactivated live virus autogenous vaccines. However, if a vectored vaccine can be provided as an autogenous vaccine, this issue can be avoided, since there is no need for live virus propagation in the production procedure.
Conclusion
Experiments with vaccines have identified several alternative methods for safer and more rapid vaccine production (e.g., subunit vaccine, DNA vaccine or vectored vaccine) than are available for traditional egg-based manufacture. Without expressing all proteins from the pathogen, these vaccines have the capability to be DIVA. Most of the experimental vaccines, which are intended to protect against infection by various influenza subtypes, have achieved considerable efficacy. IN MLV induces mucosal antibodies and nearly complete cross-protection to heterologous challenge; however, safety is a concern and a practical IN method needs to be developed. DNA vaccines may be an improved version of subunit vaccines as a result of high level expression of influenza protein(s) in hosts, although delivering DNA vaccine into cells erodes the efficiency of DNA vaccines. Vector vaccines may be regarded as superior to DNA vaccines, and are an alternative approach for DNA delivery into cells. The experience of Ad5 vectored vaccine indicates that vectored vaccines expressing HA protein may not cause vaccine-associated enhancement of respiratory disease. Whether other vectored vaccines have this advantage needs to be assessed. Since RP vectored H3 subtype vaccine is approved as a commercial vaccine, and it has the capacity to be produced as an autogenous vaccine, the RP platform has the potential to supplement or take the place of traditional inactivated IAV vaccines to rapidly provide safe IAV vaccines in the future.
The HA protein is the major antigenic component for induction of humoral HI antibodies through expression by these advanced vaccines. Unfortunately, there remains the question of limited cross protection to heterologous challenge.
The current method for protecting against diverse influenza virus strains for commercial inactivated vaccines is to include various HAs in the same inactivated vaccine. An alternative way is to use an autogenous vaccine that can be prepared rapidly and is specific to the virus strain in the swine herd. However, a universal IAV vaccine that can protect pigs is still desirable. IAV proteins that can induce cross protection against AIV may be the key for the universal IAV vaccine. Once these proteins are discovered, the RP technique will be able to express these proteins rapidly as a universal IAV vaccine. IN and other routes of administration also need to be considered as an approach to providing cross protection.



