Introduction
Multiple psychiatric disorders often co-occur in the same individuals to the extent that different research programs have been developed to explain the comorbidity and to revise diagnostic systems (Cuthbert, Reference Cuthbert2014; Del Giudice, Reference Del Giudice2016; Borsboom, Reference Borsboom2017; Kotov et al., Reference Kotov, Krueger, Watson, Achenbach, Althoff, Bagby, Brown, Carpenter, Caspi, Clark, Eaton, Forbes, Forbush, Goldberg, Hasin, Hyman, Ivanova, Lynam, Markon, Miller, Moffitt, Morey, Mullins-Sweatt, Ormel, Patrick, Regier, Rescorla, Ruggero, Samuel, Sellbom, Simms, Skodol, Slade, South, Tackett, Waldman, Waszczuk, Widiger, Wright and Zimmerman2017). Personality has not been routinely integrated to these models, and for a long time, psychiatric nosology has separated personality (Axis II) disorders from other psychiatric (Axis I) disorders. However, relationships between personality and other psychiatric disorders have been studied much (Kotov et al., Reference Kotov, Gamez, Schmidt and Watson2010), and a recent study suggested that normative and pathological personality as well as other psychiatric disorders ‘are likely to entail a common individual differences continuum’ (Oltmanns et al., Reference Oltmanns, Smith, Oltmanns and Widiger2018). Here a joint factor model over personality and psychiatric domain constructs is explored in a representative and a genetically informative population sample – to our knowledge, for the first time.
Exploratory factor analysis seeks to explain correlations among multiple variables with a smaller number of underlying ‘factors’ (Lawley and Maxwell, Reference Lawley and Maxwell1971). When fitted to data, the model may reveal a theoretically more informative account of the inter-dependencies between multiple variables. For a long time, different psychiatric disorders have been grouped into internalizing and externalizing disorder factors (also called spectra) to distinguish and characterize core processes contributing to psychiatric comorbidity (Achenbach, Reference Achenbach1966; Krueger, Reference Krueger1999; Kotov et al., Reference Kotov, Krueger, Watson, Achenbach, Althoff, Bagby, Brown, Carpenter, Caspi, Clark, Eaton, Forbes, Forbush, Goldberg, Hasin, Hyman, Ivanova, Lynam, Markon, Miller, Moffitt, Morey, Mullins-Sweatt, Ormel, Patrick, Regier, Rescorla, Ruggero, Samuel, Sellbom, Simms, Skodol, Slade, South, Tackett, Waldman, Waszczuk, Widiger, Wright and Zimmerman2017).
More recently, researchers have increasingly payed attention to the substantial correlation between the internalizing and externalizing factors (Lahey et al., Reference Lahey, Applegate, Hakes, Zald, Hariri and Rathouz2012; Kotov et al., Reference Kotov, Krueger, Watson, Achenbach, Althoff, Bagby, Brown, Carpenter, Caspi, Clark, Eaton, Forbes, Forbush, Goldberg, Hasin, Hyman, Ivanova, Lynam, Markon, Miller, Moffitt, Morey, Mullins-Sweatt, Ormel, Patrick, Regier, Rescorla, Ruggero, Samuel, Sellbom, Simms, Skodol, Slade, South, Tackett, Waldman, Waszczuk, Widiger, Wright and Zimmerman2017). On a practical level, the correlation between the internalizing and externalizing factors indicates that these broad dimensions are ‘comorbid’ with each other, and therefore may share and dilute underlying risk factors that would ideally be diagnostic targets. For these reasons, a general-factor model has been proposed, which partitions psychiatric comorbidity to a ‘super-spectrum’, or ‘p factor’, reflecting general overarching risk for all psychopathology, and two domain-specific ‘residual’ factors of internalization and externalization risk (Lahey et al., Reference Lahey, Van Hulle, Singh, Waldman and Rathouz2011, Reference Lahey, Applegate, Hakes, Zald, Hariri and Rathouz2012; Caspi et al., Reference Caspi, Houts, Belsky, Goldman-Mellor, Harrington, Israel, Meier, Ramrakha, Shalev, Poulton and Moffitt2014). The domain-specific factors are uncorrelated with the p factor in this ‘bi-factor’ model. Attempts to statistically demonstrate superiority of a given factor model compared with alternatives have run into difficulties due to possible use of too many factors (Hayashi et al., Reference Hayashi, Bentler and Yuan2007; Eid et al., Reference Eid, Geiser, Koch and Heene2017), high ‘fitting propensity’ (Bonifay and Cai, Reference Bonifay and Cai2017), and because attempts to confirm psychiatric disorders as pure ‘measures’ of an underlying factor may be unrealistic even if they would ‘reflect’ such factors (Asparouhov and Muthén, Reference Asparouhov and Muthén2009). Exploratory factor modeling suffers less from these problems (Asparouhov and Muthén, Reference Asparouhov and Muthén2009; Garrido et al., Reference Garrido, Abad and Ponsoda2013), and in terms of fit, it expresses bi-factor and correlated-factor models as coequal rotations of the same statistical model (Jennrich and Bentler, Reference Jennrich and Bentler2011, Reference Jennrich and Bentler2012). From a substantive standpoint, the models have different implications, however, as will be further discussed below. Of note, we do not consider the ‘hierarchical’ (a.k.a., ‘second-order’) factor model that is not a rotation but a constrained (i.e. confirmatory) sub-model to the rotations studied herein, and potentially very difficult to distinguish from the bi-factor model (Mansolf and Reise, Reference Mansolf and Reise2017; Caspi and Moffitt, Reference Caspi and Moffitt2018).
The previous research on bi-factor models has used limited personality data (e.g. antisocial personality disorder) (Lahey et al., Reference Lahey, Applegate, Hakes, Zald, Hariri and Rathouz2012) and studied correlations between further personality traits and model-implied factors (Tackett et al., Reference Tackett, Lahey, van Hulle, Waldman, Krueger and Rathouz2013; Caspi et al., Reference Caspi, Houts, Belsky, Goldman-Mellor, Harrington, Israel, Meier, Ramrakha, Shalev, Poulton and Moffitt2014; Neumann et al., Reference Neumann, Pappa, Lahey, Verhulst, Medina-Gomez, Jaddoe, Bakermans-Kranenburg, Moffitt, van IJzendoorn and Tiemeier2016), but they did not study more comprehensive trait systems as a possible part of the factorial structure, as suggested by Oltmanns et al. (Reference Oltmanns, Smith, Oltmanns and Widiger2018). Here, we will do this and discuss the relative parsimony of the structures that the correlated-factor and bi-factor models suggest. Among quantitative models of personality, the system of ‘Big Five’ traits has received most attention (John et al., Reference John, Naumann, Soto, John, Robins and Pervin2008; Widiger and Mullins-Sweatt, Reference Widiger and Mullins-Sweatt2009; Kotov et al., Reference Kotov, Gamez, Schmidt and Watson2010). This system compares individuals on five normative dimensions: extraversion, agreeableness, conscientiousness, neuroticism, and openness. Recently, another five-dimensional clinical version of the Big Five personality system (assessing maladaptive variants) was introduced as an alternative to, and as a possible future replacement of, the existing DSM system of personality disorders (American Psychiatric Association, 2013). Here, we use both the Big Five traits and a brief form for DSM-5 Section III personality trait model to cover both normative and pathological personality trait systems. The two systems cover partly non-overlapping personality aspects as the pathological trait system better captures genetic variance in DSM-IV personality disorders than the normative trait system (Reichborn-Kjennerud et al., Reference Reichborn-Kjennerud, Krueger, Ystrom, Torvik, Rosenström, Aggen, South, Neale, Knudsen, Kendler and Czajkowski2017; Czajkowski et al., Reference Czajkowski, Aggen, Krueger, Kendler, Neale, Knudsen, Gillespie, Røysamb, Tambs and Reichborn-Kjennerud2018).
In this study, we investigated (i) the minimum number of underlying factors that are needed to adequately account for the population correlations between variables for 11 commonly studied psychiatric disorders, five pathological personality traits, and five normative personality traits, (ii) what these factors look like from correlated-factor v. bi-factor perspectives, and (iii) what their heritability and genetic correlations are. We also (iv) address possible response style effects on factor structure, which have been frequently discussed in context of the p factor (e.g. Neumann et al., Reference Neumann, Pappa, Lahey, Verhulst, Medina-Gomez, Jaddoe, Bakermans-Kranenburg, Moffitt, van IJzendoorn and Tiemeier2016; Caspi and Moffitt, Reference Caspi and Moffitt2018; Oltmanns et al., Reference Oltmanns, Smith, Oltmanns and Widiger2018); namely, we controlled for extreme and acquiescent self-reporting styles (Weijters et al., Reference Weijters, Geuens and Schillewaert2010a, Reference Weijters, Geuens and Schillewaert2010b; Wetzel et al., Reference Wetzel, Lüdtke, Zettler and Böhnke2016) because they would have given rise to an apparent methods factor without obvious substantive interpretation. The personality research field has favored the dimensional trait systems because there has been little or no evidence supporting a typological organization of personality (Markon et al., Reference Markon, Chmielewski and Miller2011; Haslam et al., Reference Haslam, Holland and Kuppens2012; Rosenström and Jokela, Reference Rosenström and Jokela2017), and the recently suggested DSM pathological personality trait system appears to capture all the genetic and most of the environmental variance in the older typological system of personality disorders (Reichborn-Kjennerud et al., Reference Reichborn-Kjennerud, Krueger, Ystrom, Torvik, Rosenström, Aggen, South, Neale, Knudsen, Kendler and Czajkowski2017). For these reasons and for the sake of concise exposition and computational feasibility, we did not include older personality disorder systems, with the exception of antisocial personality disorder that has typically been included in studies of p factor in one form or another (e.g. conduct disorder has been used in studies on children, and registered crimes have been used in registry studies) (Lahey et al., Reference Lahey, Van Hulle, Singh, Waldman and Rathouz2011, Reference Lahey, Applegate, Hakes, Zald, Hariri and Rathouz2012; Caspi et al., Reference Caspi, Houts, Belsky, Goldman-Mellor, Harrington, Israel, Meier, Ramrakha, Shalev, Poulton and Moffitt2014; Neumann et al., Reference Neumann, Pappa, Lahey, Verhulst, Medina-Gomez, Jaddoe, Bakermans-Kranenburg, Moffitt, van IJzendoorn and Tiemeier2016; Pettersson et al., Reference Pettersson, Larsson and Lichtenstein2016; Waldman et al., Reference Waldman, Poore, van Hulle, Rathouz and Lahey2016).
Methods and materials
Sample
Data for these analyses came from a population-based sample of Norwegian twins recruited from the Norwegian Institute of Public Health Twin Panel (Nilsen et al., Reference Nilsen, Knudsen, Gervin, Brandt, Røysamb, Tambs, Orstavik, Lyle, Reichborn-Kjennerud, Magnus and Harris2013). Approval for this study was received from The Norwegian Data Inspectorate and the Regional Committee for Medical and Health Research Ethics, and written informed consent was obtained from all participants after a complete description of the study. In wave 1 data, collected between the years 1999 and 2004, lifetime history of major DSM-IV Axis I disorders and all the 10 Axis II personality disorders in the past 5 years were assessed at interview in 2801 twins (43.5% of those who were eligible; 1390 complete twin pairs and 21 single twins; average age 28.2 years, age range 19‒36). Despite moderate selection toward good mental and somatic health, attrition did not appear to affect twin analyses of mental health according to an attrition study (Tambs et al., Reference Tambs, Rønning, Prescott, Kendler, Reichborn-Kjennerud, Torgersen and Harris2009). In wave 2, altogether 2284 twins (987 complete pairs and 310 single twins) were re-interviewed approximately 10 years later, and they filled in a mailed self-report questionnaire for personality. Attrition from first to second wave was low (82.2% were retained).
Measures
At both waves, lifetime psychiatric disorders were assessed using computerized Norwegian version of the World Health Organization's Composite International Diagnostic Interview (CIDI) (Wittchen and Pfister, Reference Wittchen and Pfister1997). Criteria for antisocial personality disorder within the past 5 years were assessed using a Norwegian version of the Structured Interview for DSM-IV Personality (coded: 0 = not present or limited to rare isolated examples; 1 = subthreshold; 2 = present; 3 = strongly present) (Pfohl et al., Reference Pfohl, Blum and Zimmerman1997; Rosenström et al., Reference Rosenström, Ystrom, Torvik, Czaijkowski, Gillespie, Aggen, Krueger, Kendler and Reichborn-Kjennerud2017). At wave 1, a face-to-face interview was conducted for all but 231 individuals who were interviewed over telephone for practical reasons. All the wave 2 interviews were conducted by telephone. Interviewers were mainly senior clinical psychology graduate students and experienced psychiatric nurses. Each twin in a pair was interviewed by a different interviewer. A lifetime estimate is dependent on the interviewees’ limited memory. To maximize lifetime coverage of disorder occurrence, we counted diagnosis in either study wave as a case. For economic reasons, some (see below) of the disorders were not interviewed in the second wave. We used data on all psychiatric disorders seen in previous general-factor studies that both were available to us and had more than 100 observed cases or sub-threshold cases (excluding conduct disorder, which is considered a childhood precursor of antisocial personality).
Alcohol use disorder was indicated by either alcohol abuse (F10.1 in ICD-10) or dependence (F10.2). Substance use disorder was indicated by any of opioid abuse/dependence (F11.1 or F11.2), cannabis abuse/dependence (F12.1 or F12.2), sedative abuse/dependence (F13.1 or F13.2), cocaine abuse/dependence (F14.1 or F14.2), amphetamine abuse/dependence (F15.1 or F15.2), hallucinogen abuse/dependence (F16.1 or F16.2), or inhalant abuse/dependence (F18.1 or F18.2). Due to its rarity and possible under-reporting, we also assigned substance use disorder for those sub-threshold cases who admitted in interview having used illegal drugs more than 10 times. Other analyzed variables were any major depressive episode (F30-39), dysthymic disorder (F34.1), panic attack (F40-48), agoraphobia (F40.0), social phobia (F40.1), specific phobia (any of F40.21-25), generalized anxiety disorder (F41.1), antisocial personality traits (an ordinal count of 0, 1, 2, or 3 or more DSM-IV criteria of antisocial personality disorder, excluding childhood conduct disorder criterion), psychotic-like experiences score, a three-category ordinal variable coded by values 0, 1, and 2, constructed from 22 symptoms screen in the psychosis module of the CIDI (Nesvåg et al., Reference Nesvåg, Reichborn-Kjennerud, Gillespie, Knudsen, Bramness, Kendler and Ystrom2017), and manic experiences score, constructed from symptoms assessed in the CIDI mania module.
From the above list of variables, wave 2 assessment re-evaluated everything else except substance use disorder and psychotic-like and manic experiences. In addition, the wave 2 assessment included the Big Five Inventory (BFI) administered through a mailed questionnaire. The BFI is a 44-item inventory that measures an individual on the Big Five personality traits (John and Srivastava, Reference John, Srivastava, Pervin and John1999). The inventory assigns for each person a value on five continuously distributed traits (standardized sum scores) that currently are perhaps the most frequently used traits in personality research (John et al., Reference John, Naumann, Soto, John, Robins and Pervin2008). The traits are extraversion, agreeableness, conscientiousness, neuroticism, and openness. These traits form a comprehensive system for describing personality, which has been frequently used to predict important life outcomes, including risk for psychopathology (Kotov et al., Reference Kotov, Gamez, Schmidt and Watson2010).
The DSM-5 includes two models of personality pathology, old and new/emerging (American Psychiatric Association, 2013). The new approach includes five personality traits conceptualized as maladaptive forms of the normative personality traits: negative emotionality (or affectivity; v. emotional stability), detachment (v. extraversion), antagonism (v. agreeableness), disinhibition (v. conscientiousness), and psychoticism (v. lucidity). We included the new system as it represented ongoing progress in the field, was a complete trait system, and strongly overlapped with old personality disorders in a previous study of the same sample (Reichborn-Kjennerud et al., Reference Reichborn-Kjennerud, Krueger, Ystrom, Torvik, Rosenström, Aggen, South, Neale, Knudsen, Kendler and Czajkowski2017). The same 36-item PID-5-NBF instrument has been used previously (Personality Inventory for DSM-5, Norwegian Brief Form), but here we excluded the trait compulsivity that did not make it into DSM-5 (Reichborn-Kjennerud et al., Reference Reichborn-Kjennerud, Krueger, Ystrom, Torvik, Rosenström, Aggen, South, Neale, Knudsen, Kendler and Czajkowski2017). All continuous-valued (trait) variables were standardized to a mean of zero and a variance of one.
Statistics
Variants of the correlated-factor and/or bi-factor analysis models have been frequently applied in factorial studies of psychopathology (Krueger, Reference Krueger1999; Lahey et al., Reference Lahey, Van Hulle, Singh, Waldman and Rathouz2011; Lahey et al., Reference Lahey, Applegate, Hakes, Zald, Hariri and Rathouz2012; Caspi et al., Reference Caspi, Houts, Belsky, Goldman-Mellor, Harrington, Israel, Meier, Ramrakha, Shalev, Poulton and Moffitt2014; Pettersson et al., Reference Pettersson, Larsson and Lichtenstein2016; Waldman et al., Reference Waldman, Poore, van Hulle, Rathouz and Lahey2016; de Jonge et al., Reference de Jonge, Wardenaar, Lim, Aguilar-Gaxiola, Alonso, Andrade, Bunting, Chatterji, Ciutan, Gureje, Karam, Lee, Medina-Mora, Moskalewicz, Navarro-Mateu, Pennell, Piazza, Posada-Villa, Torres, Kessler and Scott2017). In exploratory factor analysis (Lawley and Maxwell, Reference Lawley and Maxwell1971), factor solutions are largely data-driven and need to be rotated to improve interpretability, without changing the overall model fit. Rotation methods can provide correlated and uncorrelated factors and bi-factor solutions (Jennrich and Bentler, Reference Jennrich and Bentler2011, Reference Jennrich and Bentler2012). Here we investigate two such fit-equivalent solutions: (i) a correlated-factor model that has possibly correlated but otherwise coequally treated factors and (ii) a bi-factor solution that has a general-liability factor plus specific disorder-group factors that are uncorrelated with the general factor.
In confirmatory versions of factor analytic methods, researchers decide a priori which items are to ‘measure’ (load on) which factors and then examine ensuing model fits. Here, in exploratory factor analysis, we do not make a priori assumptions. The aim is to explore what latent structures could account for the observed comorbidity between current psychiatric constructs rather than use the constructs directly as ‘measurement items’ (i.e. the aim is not to test a ‘clean’ structure without any cross-loading) (Asparouhov and Muthén, Reference Asparouhov and Muthén2009). In exploratory settings, similarity between two vectors (lists) of factor loadings is frequently quantified using congruence coefficient, ϕ, taking values between −1 and 1 (Tucker, Reference Tucker1951; Lorenzo-Seva and ten Berge, Reference Lorenzo-Seva and ten Berge2006; Abdi, Reference Abdi2007). Values in the range 0.85‒0.94 are considered to reflect ‘fair similarity’ and values above 0.95 indicate that two factors can be ‘considered equal’ (Lorenzo-Seva and ten Berge, Reference Lorenzo-Seva and ten Berge2006).
We investigated exploratory correlated-factor (i.e. Geomin rotation) and bi-factor (i.e. Bi-geomin rotation) analysis solutions to understand the patterning of correlations among the different psychiatric disorders and personality traits (Jennrich and Bentler, Reference Jennrich and Bentler2012). Specific-factor inter-correlations were allowed. Mean- and variance-adjusted weighted least-squares estimator of Mplus software was used because we had a mixture of binary, ordinal, and continuous variables (Asparouhov and Muthén, Reference Asparouhov and Muthén2009). A sandwich version of the estimator was used to take in account and adjust for the non-independence of the nested twin data (Asparouhov, Reference Asparouhov2005). Ordinal-valued variables were always modeled using a liability-threshold model (Falconer, Reference Falconer1965; Olsson, Reference Olsson1979). The optimal number of latent factors in factor analysis was determined using Horn's parallel analysis method, applied to the eigenvalues of the Mplus-estimated polychoric correlation matrix (Horn, Reference Horn1965; Garrido et al., Reference Garrido, Abad and Ponsoda2013; Rosenström et al., Reference Rosenström, Ystrom, Torvik, Czaijkowski, Gillespie, Aggen, Krueger, Kendler and Reichborn-Kjennerud2017; see an intuitive explanation in the Supplementary material). Parallel analysis was preferred over methods based on likelihood-ratio test because necessary assumptions of such tests are violated under overfactoring (Hayashi et al., Reference Hayashi, Bentler and Yuan2007; Drton, Reference Drton2009). It was also preferred over many fit indices that lose their meaning in ordinal-data factor analysis (Garrido et al., Reference Garrido, Abad and Ponsoda2016; Xia and Yang, Reference Xia and Yang2018), but we present few typical indices (RMSEA, CFI, TLI) to satisfy curiosity of many readers.
The twin ‘ACE’ model of behavior genetics was used to estimate heritability of the factors (Neale and Cardon, Reference Neale and Cardon1992; see also our Supplementary explanation). Twin models were fit in Open Mx package version 2.7.11, under R software version 3.4.1, using full-information maximum likelihood estimation (Enders and Bandalos, Reference Enders and Bandalos2001; Neale et al., Reference Neale, Hunter, Pritikin, Zahery, Brick, Kirkpatrick, Estabrook, Bates, Maes and Boker2016).
In the supplementary sensitivity analysis, we discuss the importance of controlling for measurement-related factors in more detail. In short, extreme response style (ERS) and acquiescent response style (ARS) variables were computed from the BFI items according to a previously used formula (Wetzel et al., Reference Wetzel, Lüdtke, Zettler and Böhnke2016). Response style variables show characteristics of stable individual differences (Weijters et al., Reference Weijters, Geuens and Schillewaert2010a, Reference Weijters, Geuens and Schillewaert2010b; Wetzel et al., Reference Wetzel, Lüdtke, Zettler and Böhnke2016). We found a clear response style factor unrelated to psychopathology, and therefore, pre-processed all self-reported personality trait scores by regressing out ERS and ARS factors before entering them to the factor analyses of the main text. Alternative solutions are discussed and shown in the online Supplementary material.
Results
Table 1 provides a summary of available observations and prevalence of psychiatric disorders in the sample. The personality traits are not shown in the table because they were standardized sum scores (mean 0, variance 1; each had between 2293 and 2297 valid observations; online Supplementary Table S3 for unstandardized averages). We discuss first the correlated-factor and bi-factor analyses and their supplementary sensitivity analyses, and then the biometric partitioning of the resulting factor scores.
Table 1. Lifetime prevalence estimates for the disorders
a ‘Prevalence’ of antisocial traits is instead an average over the categorical weights (see Methods section).
Joint factor structure of psychiatric disorders and personality traits
Three factors were evident in the joint data analyses on disorders and personality traits (Fig. 1a). Both correlated-factor and bi-factor solutions were fit to the data (Table 2 displays the factor loadings and Figs. 1b and 1c illustrate the structure). In the correlated-factor solution, we observed a psychopathology (p) factor without noticeable loadings on personality, but with strong correlation to another factor (personality pathology) that loaded on all other personality traits except openness. We named this factor ‘personality pathology’ because ‘pathological’ PID-5-NBF traits loaded positively on it and the loading pattern of the FFI traits on it was an inverse of the ‘general factor of personality’ that assesses positive v. negative aspects of personality, emotionality, motivation, well-being, and self-esteem (Musek, Reference Musek2007). The third factor cross-loaded on typical externalizing behaviors and correlated negatively with the first (p) factor.
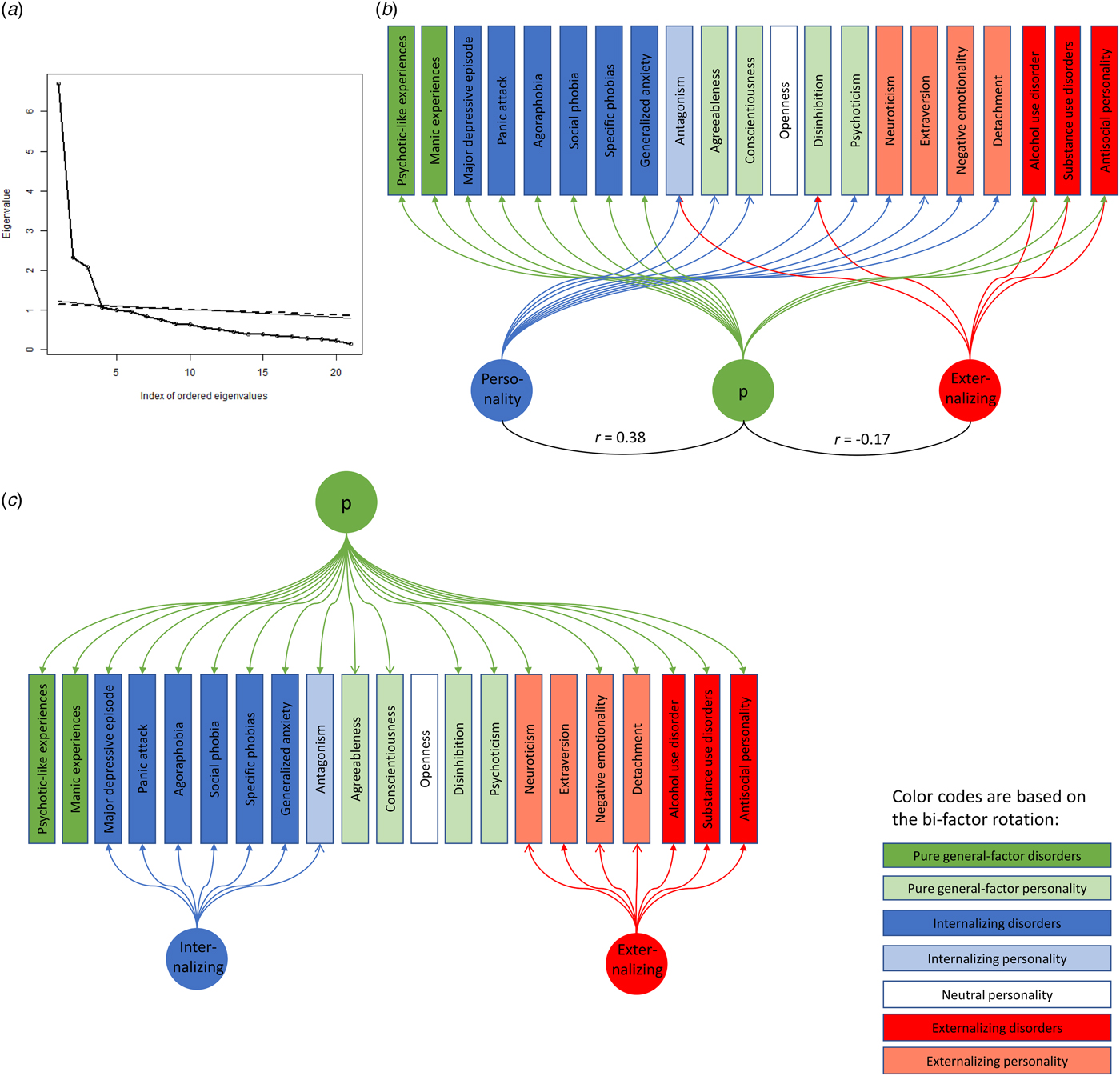
Fig. 1. Parallel analysis and path diagrams of correlated- and bi-factor models of psychopathology and personality (color figure in online version). (a) The number of observed eigenvalues (circles) above parallel-analysis (‘zero-correlation’) lines indicates the correct number of factors (i.e. 3); the two thin lines give upper (solid line; number of twin pairs) and lower (dashed line; number of twins) bounds for eigenvalues from the parallel analysis (Rosenström et al., Reference Rosenström, Ystrom, Torvik, Czaijkowski, Gillespie, Aggen, Krueger, Kendler and Reichborn-Kjennerud2017). (b) Arrows show correlated-factor model loadings above √0.1 (Table 2 for exact numeric values). (c) Bi-factor loadings. Solid arrow heads indicate positive loadings and open arrow heads indicate negative loadings. Color codes correspond to bi-factor rotation only for clarity, and ‘p’ refers to a general psychopathology factor. Black arcs indicate statistically significant factor correlations (note: internalizing and externalizing factors could have correlated in the oblique bi-factor solution, but they did not).
Table 2. Exploratory factor loadings
Loadings above √0.1≈0.316 are highlighted.
‘BFI’, Big Five Inventory; ‘PID-5-NBF’, Personality Inventory for DSM-5, Norwegian Brief Form. For statistically significant factor correlations, see Fig. 1
However, a rotation of this exploratory factor analysis solution allows another interpretation of the same statistical model having exactly the same model fit (i.e. RMSEA = 0.05 with 90% CI 0.047‒0.052, CFI = 0.914, TLI = 0.879; the numbers are the exact same for the correlated- and bi-factor models). In this bi-factor rotation, the general p factor loads on all disorders and almost all personality traits. The two residual group factors are uncorrelated with the p factor and have loadings on the typical internalizing and externalizing disorders and some of the associated personality traits. The bi-factor rotation makes the concepts of internalizing and externalizing disorders more visible by isolating the overlapping part of psychiatric comorbidity and personality content into the general p factor. It was a clinically interpretable model in the sense that there was no need to consider further latent factors that give rise to inter-factor correlations and it contained clear-cut factors for internalization and externalization. The bi-factor model incorporated personality traits and psychiatric disorders in a joint model instead of modeling pathological personality as a correlate of psychopathology.
All the factors of the bi-factor model were noticeably different from the factors of the correlated-factor model in all cross-comparisons (−0.71 < ϕ < 0.78). In contrast, the same index suggested that the general-factor loadings for interview diagnoses in the bi-factor model could be ‘considered equal’ (ϕ = 0.991 in a comparison with a strictly equal-loadings factor). When taking absolute values, uniformity held for all the general-factor loadings, including personality traits (ϕ = 0.962, and ϕ = 0.983 when excluding openness).
Supplementary sensitivity analyses of the joint factorial structure
We also investigated factor solutions with many other rotations and sets of input variables, although we chose to present only those in Table 2 in the main text for the sake of clarity. When we did not remove response style effects from the personality variables, we observed a similar bi-factor solution as in Table 2, but with an additional difficult-to-interpret specific factor for personality (online Supplementary Table S1). Inserting our response style variables into the factor model revealed that one of the four factors was related to response styles and unrelated to psychopathology (online Supplementary Table S2). For the sake of conciseness, pertinent response styles were regressed out, but this did not have a major influence on other structure than the response style factor.
Heritability patterns of factor scores
Heritability estimates (proportion of additive-genetic variance; h 2) of factor scores derived from the correlated-factor model were 48% (95% CI 42‒55%) for the p factor, 41% (CI 35‒48%) for the personality pathology factor, and 43% (CI 36‒50%) for the externalizing factor. Heritability estimates of the bi-factor scores were 48% (CI 41‒54%) for the p factor, 35% (CI 28‒42%) for the internalizing factor, and 37% (CI 31‒44%) for the externalizing factor. We did not observe statistically significant effects of twin pairs’ shared environment. Overall, the correlated-factor model implied higher phenotypic and genetic factor correlations than the bi-factor model (Table 3).
Table 3. Factor score correlations
Phenotypic correlations are Pearson correlations of factor scores, below-diagonal cells under biometric correlations give genetic correlations, and above-diagonal cells give environmental correlations. The correlations are based on model-derived (phenotypic) factor scores and can differ from model-implied latent correlations of Fig. 1, e.g. due to measurement noise (van den Berg et al., Reference van den Berg, Glas and Boomsma2007)
Discussion
We found three factors underlying the joint structure of 11 psychiatric disorders and 10 normal and pathological personality traits. This structure was explored using two statistically equivalent exploratory factor models, correlated-factor and bi-factor models that still provided different interpretations regarding the joint structure of psychiatric disorders and personality and on comorbidity. According to the correlated-factor model, psychiatric disorders, personality traits, and externalizing behaviors all reflected separate underlying factors that were inter-correlated and similarly heritable [41‒48%; a typical range (Polderman et al., Reference Polderman, Benyamin, de Leeuw, Sullivan, van Bochoven, Visscher and Posthuma2015)]. According to the alternative bi-factor rotated solution, all disorders and almost all personality traits reflected a general dimension of psychopathology (48% heritable p factor) plus less-heritable specific residual factors for internalizing and externalizing traits (35% and 37% heritable, respectively). The latter model was more parsimonious in that it had fewer and lower unexplained factor correlations and cross-loadings (but it was not different in terms of statistical fit). For both the models, genetic and environmental factor-score correlations differed from phenotypically observed correlations, but in the bi-factor model genetic correlations between the general and the specific factors remained moderate. This makes the general factor perhaps a more salient (less confounded/correlated) target for genome-wide and neuroscientific studies of psychiatric comorbidity compared with the disorder factor from the correlated-factor model, as explained below and in pertinent literature (Lahey et al., Reference Lahey, Krueger, Rathouz, Waldman and Zald2017; Caspi and Moffitt, Reference Caspi and Moffitt2018; Oltmanns et al., Reference Oltmanns, Smith, Oltmanns and Widiger2018).
The findings from the joint correlated-factor model of psychiatric disorders and normative and pathological personality conceptualized personality traits and psychiatric disorders as reflecting separate correlated factors. Under this theory, a researcher interested in associations between the disorder liability and third factors (e.g. a gene or an exposure) would typically adjust for ‘confounding’ personality, thus discarding the variance overlapping with it. In contrast, the p factor from the bi-factor model incorporates disorder-overlapping parts of personality and rules out the rest. In theory, the bi-factor model is practically useful in the sense that the p factor is pertinent to comorbidity research without further difficult-to-interpret controls for correlated residual personality, normative or pathological. In practice, this held better for genetic than for environmental influences, for which residual correlations remained in factor scores (Table 3). At this point, we do not take a strong position for or against either explorative structural model, but instead emphasize the higher level of parsimony of the bi-factor model, its connections with the existing literature, and its potential for generating hypotheses for future research.
For example, the personality trait antagonism is typically associated with externalizing psychiatric disorders (e.g. substance abuse), which involve aggression. On the other hand, internalizing disorders (e.g. depression) are typically associated with personality traits such as neuroticism that involves frequent negative emotions, including anger (Kotov et al., Reference Kotov, Gamez, Schmidt and Watson2010). In the correlated-factor model, such overlapping psychological content was expressed both in correlations between assumed latent factors and in cross-loadings (i.e. in some measured traits reflecting one part one factor, another part another factor). The same model can be expressed in a perhaps more conceptually trackable (bi-factor) form, with less-correlated factors and with cross-loadings constrained to general factor only (Fig. 1). These fit-equivalent interpretations (rotations) generate distinct hypotheses for future research. In the example case, the correlated-factors model implies that high antagonism is directly indicative of high risk for personality pathology and externalizing traits, whereas the bi-factor model implies that antagonism is instead indicative of general psychopathology with a lack of ‘normal’ internalizing tendency. This distinction can only be seen in the multivariate context, yet, might turn out clinically significant in the future research.
It is not well-understood what might give rise to a general factor of psychopathology, but several suggestive findings and proposals exist. Different authors have linked the p factor with functional arguments related either to life-history strategies (Del Giudice, Reference Del Giudice2014), to balance in fast v. slow cognitive processes (Carver et al., Reference Carver, Johnson and Timpano2017), to general integrity of the nervous system (Caspi et al., Reference Caspi, Houts, Belsky, Goldman-Mellor, Harrington, Israel, Meier, Ramrakha, Shalev, Poulton and Moffitt2014), and/or to inefficient intrinsic functional brain connectivity (Elliott et al., Reference Elliott, Romer, Knodt and Hariri2018). Empirical studies have reported physiological findings common to multiple psychiatric disorders, such as changes in volume of overlapping brain areas (Goodkind et al., Reference Goodkind, Eickhoff, Oathes, Jiang, Chang, Jones-Hagata, Ortega, Zaiko, Roach, Korgaonkar, Grieve, Galatzer-Levy, Fox and Etkin2015), shared cortical gene expression patterns (Gandal et al., Reference Gandal, Haney, Parikshak, Leppa, Ramaswami, Hartl, Schork, Appadurai, Buil, Werge, Liu, White, Consortium, Consortium, Horvath and Geschwind2018), overlapping genetic correlates (Lahey et al., Reference Lahey, Van Hulle, Singh, Waldman and Rathouz2011; Geschwind and Flint, Reference Geschwind and Flint2015; Neumann et al., Reference Neumann, Pappa, Lahey, Verhulst, Medina-Gomez, Jaddoe, Bakermans-Kranenburg, Moffitt, van IJzendoorn and Tiemeier2016; Pettersson et al., Reference Pettersson, Larsson and Lichtenstein2016; Wang et al., Reference Wang, Gaitsch, Poon, Cox and Rzhetsky2017), and lower than average performance level in tests of intelligence (Caspi et al., Reference Caspi, Houts, Belsky, Goldman-Mellor, Harrington, Israel, Meier, Ramrakha, Shalev, Poulton and Moffitt2014; Neumann et al., Reference Neumann, Pappa, Lahey, Verhulst, Medina-Gomez, Jaddoe, Bakermans-Kranenburg, Moffitt, van IJzendoorn and Tiemeier2016). Capturing possible shared etiologies of multiple psychiatric disorders to a single phenotype (factor) rather than in correlations between multiple phenotypes (factors) has potential to bring clarity to psychiatric nosology. This is a major argument in favor of the bi-factor model. A general-factor model of psychopathology and personality may offer scientific parsimony and clinical utility by treating psychiatric comorbidity as a measurable construct instead of an unexplained correlation.
In a partial contrast, Oltmanns et al. (Reference Oltmanns, Smith, Oltmanns and Widiger2018) argued that modeling of general factors may not be etiologically informative, as they might arise from impairments and dysfunctions that are secondary to underlying causes. It remains unclear how the hypothesis links with the abovementioned etiologic factors and why the etiology is so different for psychiatric disorders in comparison to other (e.g. neurological) disorders that also imply severe impairment and dysfunction (Wang et al., Reference Wang, Gaitsch, Poon, Cox and Rzhetsky2017; Brainstorm Consortium, 2018). Empirically, Oltmanns et al. (Reference Oltmanns, Smith, Oltmanns and Widiger2018) solution resembled our correlated-factor model, albeit with stronger factor correlations that may relate to use of more measurement items in their study or to their use of confirmatory framework wherein non-pure indicators can inflate absolute factor correlations (Asparouhov and Muthen, Reference Asparouhov and Muthén2009; Morin et al., Reference Morin, Arens and Marsh2016).
Sometimes researchers try to infer psychological content of the general factor based on comparatively high loading magnitudes of given disorders on the general factor and lack of specific factors for the disorders, as has been observed for psychotic disorders in comparison to other disorders (Caspi et al., Reference Caspi, Houts, Belsky, Goldman-Mellor, Harrington, Israel, Meier, Ramrakha, Shalev, Poulton and Moffitt2014; Carver et al., Reference Carver, Johnson and Timpano2017). However, we observed similar loading magnitudes for psychotic-like and manic experiences as for other disorders, and our general factor was highly congruent with uniform loadings for all disorders and personality traits. In fact, when we computed congruence coefficients between a uniformly loading factor and the ‘psychosis-heavy’ general factor reported in Caspi et al. (Reference Caspi, Houts, Belsky, Goldman-Mellor, Harrington, Israel, Meier, Ramrakha, Shalev, Poulton and Moffitt2014), it too exceeded a recommended cut-off for two factors being ‘considered equal’ (i.e. ϕ = 0.962 > 0.95) (Lorenzo-Seva and ten Berge, Reference Lorenzo-Seva and ten Berge2006). Eid et al. (Reference Eid, Geiser, Koch and Heene2017) noted that finding one non-significant specific factor is common in confirmatory bi-factor analyses, which they attributed to low identifiability and to a need to a priori anchor the general factor on some variable(s). Thus, use of pre-established and clear criteria for inferring differential loading magnitudes and patterns would help in distinguishing them from sampling noise, near-equivalent solutions, and other idiosyncratic variation. The higher loadings on psychotic v. other disorders observed by Caspi et al. (Reference Caspi, Houts, Belsky, Goldman-Mellor, Harrington, Israel, Meier, Ramrakha, Shalev, Poulton and Moffitt2014) might also relate to their very high participant retention rate, including psychotic individuals. If unbiased, our uniform factor loadings imply that all variables reflect the factor equally much in terms of their overall variance. In bi-factor models, however, one needs to assess several variables jointly to separate their residual and group factors from the general-factor score.
It is a limitation that exploratory correlated-factor and bi-factor models are statistically equivalent, having equal fit to data. One model may offer a more parsimonious interpretation than the other, but further studies are needed before either of the models can be claimed to reveal underlying etiologic processes. For example, longitudinal studies could be helpful, as well as biometric path studies (Franić et al., Reference Franić, Dolan, Borsboom, Hudziak, van Beijsterveldt and Boomsma2013) preferably in larger datasets compared with this study. On the positive side, much of the criticism and problems pertinent to confirmatory bi-factor modeling do not carry over to the present case of exploratory rotations (Asparouhov and Muthén, Reference Asparouhov and Muthén2009; Jennrich and Bentler, Reference Jennrich and Bentler2011, Reference Jennrich and Bentler2012; Eid et al., Reference Eid, Geiser, Koch and Heene2017). Furthermore, the latent distribution of factor models (a multivariate normal distribution) is typically chosen to facilitate computation, not because it necessarily best reflects ‘the nature’ (Lei and Lomax, Reference Lei and Lomax2005); here we developed some substantive arguments to distinguish between rotations and also technical arguments can be developed when multivariate normality is not assumed (Hyvärinen et al., Reference Hyvärinen, Karhunen and Oja2001; see also our Supplementary material). In addition, our estimates of heritability are lower bounds (i.e. likely underestimates) because, for computational reasons, we had to use a two-step procedure with heritability estimation performed on pre-computed phenotype-based estimates of factor scores (van den Berg et al., Reference van den Berg, Glas and Boomsma2007). In principle, factor and biometric models can be fully combined (Neale and Cardon, Reference Neale and Cardon1992; Franić et al., Reference Franić, Dolan, Borsboom, Hudziak, van Beijsterveldt and Boomsma2013; Rosenström et al., Reference Rosenström, Ystrom, Torvik, Czaijkowski, Gillespie, Aggen, Krueger, Kendler and Reichborn-Kjennerud2017). In practice, our attempts were thwarted either by computational demands of multivariate integration in case of ordinal-valued full-information approach or by instability of approaches like weighted least-squares estimation within relatively small zygosity sub-groups. Furthermore, our estimates could be subject to a degree of recruitment and attrition bias in the sample, or bias from just single occasion of self-reporting as opposed to two interviews, although an attrition study only indicated moderate selection toward good health without bias in genetic or environmental covariance structures (Tambs et al., Reference Tambs, Rønning, Prescott, Kendler, Reichborn-Kjennerud, Torgersen and Harris2009).
In summary, allowing for a correction for response styles, inter-correlations between psychiatric disorders and pathological and normative personality traits could be explained with three factors. Whereas a correlated-factor model led to distinct (but correlated) psychiatric-disorder and personality-pathology factors, an equally fitting bi-factor model led to an overarching shared psychopathology factor for disorders and normative and pathological personality traits, plus orthogonal domain-specific factors for internalizing and externalizing disorders and traits. The latter interpretation of the data promotes a joint etiologic model of comorbid personality pathology and general psychopathology, with potential to increase theoretical and diagnostic parsimony in psychiatry and to provide more interpretable target phenotypes for genetic studies.
Author ORCIDs
Tom Rosenström http://orcid.org/0000-0001-8277-3776.
Supplementary material
The supplementary material for this article can be found at https://doi.org/10.1017/S0033291718002982
Acknowledgements
We acknowledge funding from the US National Institutes of Health and National Institute on Drug Abuse (1R01DA037558-01A1), the Research Council of Norway (226985; 240061), the Norwegian Foundation for Health and Rehabilitation, the Norwegian Council for Mental Health, and the European Commission under the program ‘Quality of Life and Management of the Living Resources’ of the Fifth Framework Program (QLG2-CT-2002-01254). THR had full access to all the data in this study and takes responsibility for the integrity of the data and the accuracy of the data analysis. The funding sources had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication. All the authors report no conflicts of interest. The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008.
Financial support
We acknowledge funding from the US National Institutes of Health and National Institute on Drug Abuse (1R01DA037558-01A1), the Research Council of Norway (226985; 240061), the Norwegian Foundation for Health and Rehabilitation, the Norwegian Council for Mental Health, and the European Commission under the program ‘Quality of Life and Management of the Living Resources’ of the Fifth Framework Program (QLG2-CT-2002-01254).