INTRODUCTION
According to the US Supreme Court, all individuals charged with a crime must be competent to stand trial (CST). As defined in Dusky v. US, 1 competency requires that defendants have the ability to consult with their attorney with a reasonable degree of rationality and possess a rational as well as factual understanding of the legal proceedings. The precise number of CST evaluations conducted each year is unknown. The oft-reported figure of 60,000 provided by Bonnie and GrissoReference Bonnie, Grisso, Grisso and Schwartz 2 is an estimate based on the number of felony indictments coupled with the estimated percentage of referrals for competency evaluations made by the courts in the 1990s. Later work has suggested a much higher number.Reference Vitacco, Rogers and Gabel 3 Using a similar method, Vitacco and colleagues examined surveys indicating the frequency with which the issue of competency is raised by defense attorneysReference Melton, Petrila, Poythress and Slobogin 4 and arrest rates at the time of publishing. They deduced that a conservative estimate of the quantity of evaluations could be 700,000 annually.Reference Vitacco, Rogers and Gabel 3
The national dilemma
Consistent with Vitacco’s estimates, reports suggest that the number of referrals for competency evaluations and subsequent restoration services are increasing nationally. The state of Washington experienced an 82% increase in referrals for competency evaluations between the years 2000–2011. 5 In Colorado, requests for competency evaluations increased 524% from 2000-2017; corresponding requests for restoration increased 931% in the same timeframe.Reference Phillips 6 Los Angeles County experienced an increase of 273% in competency referrals for misdemeanant offenders from 2010 to 2015.Reference Sewell 7 , Reference Gowensmith, Frost, Speelman and Therson 8 In Michigan, the number of evaluations rose from 3,000 in 2010 to 4,500 in 2016.Reference Hinkley 9 In Metro Detroit alone, the number of evaluations ordered increased 20% from 2012 to 2016.Reference Brand-Williams 10 In California, referrals to the Department of State Hospital (DSH) system for competency restoration almost doubled from fiscal year 2013/2014 to 2015/2016.Reference Lowder 11
As the number of referrals and evaluations increase, so does the corresponding number of defendants determined to be incompetent. Research consistently suggests that between 25% and 30% of defendants referred for CST evaluations are adjudicated incompetent.Reference Gowensmith, Frost, Speelman and Therson 8 , Reference Pirelli, Gottdiener and Zapf 12 McDermott and colleagues estimated that this would translate to a range of 15,000–30,000 defendants found incompetent every year, with substantially more if the figures of evaluation referrals from Vitacco et al. are accurate.Reference Vitacco, Rogers and Gabel 3 , Reference McDermott, Newman, Meyer, Scott and Warburton 13 In many jurisdictions, competency restoration occurs on an inpatient basis in state psychiatric hospitalsReference Gowensmith, Frost, Speelman and Therson 8 and evidence suggests that patients admitted as incompetent to stand trial (IST) comprise the largest proportion of forensic patients in hospitals throughout the nation.Reference Wik, Hollen and Fisher 14 , Reference Miller 15 According to recent reports, over 50% of the total patients in the California DSH were IST as of February 2016.Reference Bartos, Renner, Newark, McCleary and Scurich 16
There are many potential explanations for these observed increases, such as decreasing access to treatment for both mental illness and substance use in the communityReference Torrey, Kennard, Eslinger, Lamb and Pavle 17 ‑ Reference Bondurant, Lindo and Swenson 19 and decreasing availability of inpatient psychiatric beds.Reference Torrey, Kennard, Eslinger, Lamb and Pavle 17 For example, Los Angeles has experienced a 30% decrease in the number of inpatient psychiatric beds from 1995 to 2010.Reference Sewell 7 Others have postulated that the increased popularity of specialty courts, such as mental health and drug courts, contribute to an increase in competence referrals for defendants who are unable to comply with the guidelines stipulated by these courts because of their serious mental illness.Reference Stafford, Sellbom, Weiner and Otto 20 Some have suggested a more complex series of events as an explanation for the increasing numbers of IST commitments. The Director of Community Health and Integrated Programs at the Los Angeles County Department of Health Services was cited as believing that his city’s rise in competency referrals is due to the combination of homelessness, increasing awareness of mental illness in the criminal justice system, and increasing methamphetamine use.Reference Sewell 21
An alternative explanation for the increase in IST referrals is the frequency of malingering of psychiatric or cognitive symptoms among defendants coupled with the relative infrequency of court-appointed evaluators to systematically assessing feigning.Reference McDermott, Newman, Meyer, Scott and Warburton 13 Rates of malingering on competency evaluations have been estimated to be as high as 21%.Reference Vitacco, Rogers, Gabel and Munizza 22 In a study reviewing 464 competency reports, only 194 (41.8%) of evaluators considered the legitimacy of the reported symptoms and of those, only 69 (14.9%) employed a structured assessment of feigning.Reference Homsy, McDermott and Woofter 23 It follows that if referrals for evaluations are increasing, but evaluators are not assessing for possible malingering, there could be an increase in patients erroneously ruled incompetent.
Regardless of the source, it is clear that referrals for both competency evaluations and restoration services are increasing nationally. Although alternatives to inpatient psychiatric treatment for restoration recently have been suggested or implemented, Reference Gowensmith, Frost, Speelman and Therson 8 with no adequate explanation for the observed increases that might suggest a reasonable solution, this trend is likely to continue.
Characteristics of IST offenders
In studies of IST populations, there is a distinction between individuals referred for competency evaluations versus individuals on whom competency decisions have been made after evaluation. Although not specifically designed to understand the reasons for rises in IST referrals, both for evaluation and restoration, sociodemographic data, such as age, gender, and race are frequently gathered to better understand the IST population. For example, research has shown that defendants found incompetent to stand trial tend to be older than competent defendants.Reference Pirelli, Gottdiener and Zapf 12 , Reference Cooper and Zapf 24 – Reference Bartos, Renner, Newark, McCleary and Scurich 27 However, among an all-female sample studied by Kois and colleagues, age was not a significant characteristic in predicting competency, Reference Kois, Pearson, Chauhan, Goni and Saraydarian 28 suggesting that women may have unique characteristics in the criminal justice system. Study samples of patients referred for competency restoration indicate that most are male.Reference Cooper and Zapf 24 , Reference Hubbard, Zapf and Ronan 26 , Reference Warren, Murrie and Stejskal 27 However, although men are more frequently evaluated for competency, not surprising given the higher numbers of men arrested, studies have found that males and females are equally likely to be ruled incompetent in the US.Reference Pirelli, Gottdiener and Zapf 12
In terms of race and ethnicity, research has shown that the overrepresentation of people of color in the criminal justice system may be mirrored in the forensic psychiatric system for competency restoration.Reference Pinals, Packer, Fisher and Roy-Bujnowski 29 Research has shown that African Americans are more often referred for competency evaluations.Reference Cooper and Zapf 24 , Reference Hubbard, Zapf and Ronan 26 , Reference Kois, Pearson, Chauhan, Goni and Saraydarian 28 , Reference Pinals, Packer, Fisher and Roy-Bujnowski 29 This discrepancy continues even after the competency decision is made. Pirelli and colleagues demonstrated that, in 22 studies that presented ethnicity data, minority defendants were 1.5 times more likely to be found incompetent than white defendants.Reference Pirelli, Gottdiener and Zapf 12 One contributing factor could be the higher likelihood of a diagnosis of a psychotic or mood disorder among African Americans and Hispanics respectively.Reference Caldwell, Mandracchia, Ross and Silver 30 , Reference Minsky, Vega, Miskimen, Gara and Escobar 31
In regards to symptomatology, defendants found incompetent are more likely to be diagnosed with a psychotic disorder or evidence symptoms of psychosis than competent defendants or those not referred for an evaluation.Reference Pirelli, Gottdiener and Zapf 12 , Reference Cooper and Zapf 24 , Reference Hubbard, Zapf and Ronan 26 , Reference Viljoen and Zapf 32 , Reference Gay, Vitacco and Ragatz 33 Cognitive disabilities also are closely related to incompetency.Reference Bartos, Renner, Newark, McCleary and Scurich 16 , Reference Warren, Murrie and Stejskal 27 , Reference Cochrane, Grisso and Frederick 34 Diagnoses, therefore, can confound other variables associated with incompetency. Among the elderly community, the correlation between an older age and decreased competency to stand trial could be explained by a greater prevalence of cognitive disorders.Reference Frierson, Shea and Shea 25 , Reference Lewis, Fields and Rainey 35 Defendants with personality disorders and/or substance use disorder diagnoses are less likely to be found incompetent to stand trial.Reference Cooper and Zapf 24 , Reference Hubbard, Zapf and Ronan 26 , Reference Viljoen and Zapf 32 Viljoen and ZapfReference Viljoen and Zapf 32 found that defendants referred for competency evaluations were less likely to have a primary substance abuse disorder and less likely to meet the criteria for antisocial personality disorder as compared to those not referred, a result consistent with other research.Reference Cooper and Zapf 24 , Reference Hubbard, Zapf and Ronan 26
Other well-studied variables among the IST population are restorability and length of stay, both related to the nature of the mental disorder. A patient’s diagnosis, or how symptomatic the patient is, can determine if they are successfully restored and how long that process takes.Reference Gay, Vitacco and Ragatz 33 Research has shown that cognitive disability and psychotic symptomology are not just associated with findings of incompetency, but also with restorability and a prolonged length of stay. 36-39 Using records from 351 inpatient pretrial defendants who underwent competence restoration at a state psychiatric hospital from 1995 through 1999, patients with prolonged psychotic disorders and irremediable cognitive disorders were less likely to be restored.Reference Mossman 36 Similarly, Morris & DeYoungReference Morris and DeYoung 39 found that among 455 male defendants admitted to a forensic treatment center for competency restoration, psychotic disorders and cognitive disability predicted unsuccessful restoration within three months of treatment. They also demonstrated that diagnoses of personality disorders and substance use might represent a higher likelihood of competence, as they were predictive of successful restoration. Anderson and HewittReference Anderson and Hewitt 40 found that both higher intelligence and being African American was predictive of restoration. Others have found no major difference in populations of patients who have been restored vs. those who have not.Reference Advokat, Guidry, Burnett, Manguno-Mire and Thompson 41
Criminogenic factors also have been studied with respect to competency to stand trial, although research suggests this is closely intertwined with other variables, such as diagnosis. Previous work has demonstrated that violent crimes are more often associated with competency, while nonviolent offenses are associated with incompetency.Reference Cooper and Zapf 24 , Reference Hubbard, Zapf and Ronan 26 , Reference Rosenfeld and Ritchie 42 , Reference Warren, Rosenfeld, Fitch and Hawk 43 In contrast, Cochrane and colleagues found that violent charges were associated with high rates of incompetency findings.Reference Cochrane, Grisso and Frederick 34 However, when the authors controlled for diagnosis, the significance of the relationship disappeared. Kois and colleagues initially found that although nonfelony charges were more likely associated with incompetency, active psychotic symptoms were more predictive.Reference Kois, Pearson, Chauhan, Goni and Saraydarian 28 Similarly, Viljoen and Zapf reported no difference in charging offense between defendants referred for an evaluation and those not referred for an evaluation.Reference Viljoen and Zapf 32 In contrast, Pirelli and colleagues, when evaluating rulings of competency, found that among the studies that discussed current criminal charges, defendants with a violent charge were more likely to be found competent.Reference Pirelli, Gottdiener and Zapf 12
Importance
Regardless of the characteristics of the defendants found IST, the increasing numbers of these types of admissions is real and the impact has been detrimental. Patients in need of treatment can wait in jail for weeks for admission to a hospital.Reference Gowensmith, Frost, Speelman and Therson 8 Moreover, over-crowded forensic psychiatric institutions can risk staff safety and patient well-being. To better understand this growing population and to inform hospital administration, the University of California Davis, in partnership with the Department of State Hospitals’ (DSH) facility in Napa (DSH-Napa) implemented a triage screening procedure for individuals admitted for restoration to competence. This study utilizes archival clinical data from these screenings for IST patients admitted from 2009–2016. In addition to describing the sociodemographic, psychiatric, and criminal variables and the interrelationship between these factors, we examined changes over time to assess if any demographic or clinical factors were related to the observed increase in these types of commitments.
METHOD
This research was approved by all relevant institutional review boards. The details of the methods and procedures have been described in a previous paper.Reference McDermott, Newman, Meyer, Scott and Warburton 13 Briefly, the study was conducted at DSH-Napa, a 1200-bed primarily forensic inpatient psychiatric facility located in northern California. Approximately 380 beds are allocated for the restoration of patients committed as IST. The records of patients found IST and admitted to DSH-Napa for restoration of competence between the dates of 1/1/2009 and 12/31/2016 were eligible for inclusion in the study.
Procedure
All patients were admitted directly from the referring county jails. One component of the admission screening was a brief interview conducted by a psychologist, psychiatrist, or research assistant coupled with structured assessments. Once the patient was interviewed and assessment tools were completed, the interviewer was asked to form judgments about the patients’ overall competence and on both components of the California competency standard (understanding of criminal proceedings and ability to assist in their defense), potential for feigning of psychiatric symptoms or cognitive/memory deficits, and presence of possible cognitive deficits. These opinions were documented on a coding sheet that also included basic demographic information, clinical information (eg, current medications, prior psychiatric treatment), criminal arrest information (eg, most serious commitment offense, prior IST finding, number of prior arrests), as well as scores from the structured assessments. All interviewers were trained in these procedures. While interrater reliability was not conducted, all interviewers received extensive training in these screening procedures.
Measures
The M-FAST
The Miller Forensic Assessment of Symptoms TestReference Miller 44 (M-FAST) was developed as a screening instrument designed to identify feigned psychopathology. It is a 25-item structured interview that can be administered in approximately 5 minutes. Although it contains multiple subscales, a total score of 6 or greater is suggested as indicative of a need for a more extensive assessment of feigning. Scores in the sample ranged from 0 to 25, with an average score of 4.41 and a standard deviation of 4.89. While the modal score was 0, 31.0% scored at or above 6, the cut score for suspected malingering.
The BPRS
The Brief Psychiatric Rating ScaleReference Overall and Gorham 45 (BPRS) was used to quantify psychotic symptoms. The BPRS consists of 18 items rating psychiatric symptoms such as anxiety, depression, and hallucinations. It is a widely used assessment that includes affective symptoms and hostility as well as both positive and negative symptoms of a psychotic disorder. The four items quantifying positive psychotic symptoms were selected for the brief screen (ie, thought disorganization, suspiciousness, hallucinations and unusual thought content). Items are rated on a seven-point scale, with 1 indicating that the symptom was not observed and 7 indicating that the symptom was very severe. Scores in this sample ranged from 1 to 25, with higher scores indicating more severe psychotic symptoms. The mean score for the sample was 9.03 with a standard deviation of 4.79.
Competency screening
Four items were selected from the Georgia Court Competence TestReference Johnson and Mullett 46 (GCCT) to assess the patients’ abilities to understand courtroom proceedings. The GCCT was designed as a screening tool for assessing competence specific to the criteria in the United States. It contains three sections, including knowledge of the physical locations of courtroom personnel and their roles as well as an assessment of the defendant’s ability to assist in their defense. The four questions selected in this study included the defendant’s understanding of the roles of four courtroom personnel (defense attorney, district attorney, judge, jury). An additional question asked the defendant to name their attorney and express their beliefs about the adequacy of their attorney’s performance (eg, “What do you think of your attorney? What has it been like to work with him/her?”). Each item was scored as 0, 1 or 2, with 2 indicating an adequate answer, 1 a partially correct answer, and 0 either no answer or a wrong or delusionally-based response. Because there were five questions, scores ranged from 0 to 10. The average score was 5.74 with a standard deviation of 3.29.
Participants
There were a total of 3158 unduplicated IST admissions available during the specified time period. Women comprised 25.4% of the admissions (N = 802). Most admissions were White (n = 1352, 42.8%), with the remainder Black (n = 917, 29.0%), Hispanic (n = 583, 18.5%), Asian (n = 207, 6.6%), or of other ethnic descent (n = 98, 3.1%). The largest number of patients reported not completing high school (n = 1005, 43.1%), although many had a high school diploma or equivalent (n = 659, 28.3%), and a substantial number had some educational experience beyond high school (n = 668, 28.6%). The age of the patients on admission ranged from 18 to 89, with an average age of 38.77 (std = 13.07). The majority of patients reported at least one prior inpatient psychiatric admission as an adult (n = 1540, 60.5%), although many reported no prior psychiatric history, either inpatient or outpatient (n = 577, 22.7%). The remainder reported a history of mental health treatment only as a juvenile or as an outpatient (n = 427, 16.8%). Past psychiatric treatment was unavailable on 614 patients. Most admissions were English speaking (n = 2793, 93.7%); language was a barrier in 5.6% of interviews conducted (n = 166). The most common commitment offense was assault/battery (n = 1048, 35.7%), followed by theft (n = 284, 9.7%), robbery (n = 278, 9.5%), a sex offense (n = 231, 7.9%), murder (n = 224, 7.6%), miscellaneous charges (eg, vandalism, disorderly conduct; n = 194, 6.6%), criminal threats (n = 140, 4.8%), drug offenses (n = 140, 4.8%), weapons offenses (n = 121, 4.1%), arson (n = 103, 3.5%), resisting arrest (n = 72, 2.5%) and other (kidnapping, white collar crimes, major driving offenses, escape, (n = 97, 3.3%). For 226 (7.2%) of the admissions, the offense was not recorded. Only the most serious offense was recorded as the commitment offense.
Of the 3158 patient records reviewed during the specified time period, 87.3% (n = 2757) were returned to court as competent. Over 10% (10.8%, n = 342) were deemed not restorable and were either discharged or conserved as dangerous or gravely disabled, and 1.9% (n = 59) were transferred to another facility, were released by the court, died during their hospitalization, or were retained in the hospital for another forensic commitment, such as an not guilty by reason of insanity (NGRI) finding.
Of the 3158 admissions, 1099 (34.8%) could not be interviewed. Reasons for the inability to interview the patient varied. For example, some patients were too thought disordered to conduct an adequate interview (n = 392, 35.7%), some refused to cooperate with the interview (n = 292, 26.6%), some were unable to speak English (n = 125, 11.3%), some were too agitated or physically threatening (n = 68, 6.2%), and sometimes the interviews were not able to be completed due to the patients’ dementia or medical problems (n = 30, 2.7%). One hundred and ninety-three patients (17.6%) were not interviewed for unknown reasons (not documented by the evaluator).
Data analysis
Data were analyzed using SPSS version 25. Statistical analyses included frequency distributions to provide information regarding basic demographics. Chi-square and ANOVAs were conducted to assess differences over time and interactions between various factors.
RESULTS
As shown in
Table 1, the number of IST admissions increased yearly throughout the course of this study. In 2009, 280 unique patients were admitted as IST compared to 539 in 2016. Additionally, a large number of factors exhibited statistically significant variability over time. Most notably, the number of admissions with more than 15 prior arrests increased significantly (
![]() $ \chi $
2
= 139.84, df = 28, p = .000) from 17.7% in 2009 to 46.4% in 2016, depicted graphically in
Figure 1. Multiple other variables evidenced changes over time, although often the statistically significant change was related to increases and decreases from year to year. For example, admissions that were thought to be already competent evidenced statistically significant differences over time (
$ \chi $
2
= 139.84, df = 28, p = .000) from 17.7% in 2009 to 46.4% in 2016, depicted graphically in
Figure 1. Multiple other variables evidenced changes over time, although often the statistically significant change was related to increases and decreases from year to year. For example, admissions that were thought to be already competent evidenced statistically significant differences over time (
![]() $ \chi $
2
= 93.36, df = 14, p = .000), from a high of 24.6 in 2010 to a low of 10.7 in 2014.
$ \chi $
2
= 93.36, df = 14, p = .000), from a high of 24.6 in 2010 to a low of 10.7 in 2014.
TABLE 1. Changes in factors assessed over time

a Diagnoses on admission
b Women only admitted beginning in May 2010

FIGURE 1. Percent of admissions with 16+ prior arrests.
One variable that evidenced a consistent decrease over time was the percent of patients reporting prior inpatient psychiatric hospitalization (
![]() $ \chi $
2
= 183.12, df = 14, p = .000). The percentage of admissions reporting at least one past psychiatric hospitalization was over 76% in 2009 and decreased steadily to less than 50% in 2016. As seen in
Figure 2, this decrease appeared primarily related to declines in hospitalizations reported by admissions diagnosed with unspecified schizophrenic spectrum and other psychotic disorder (
$ \chi $
2
= 183.12, df = 14, p = .000). The percentage of admissions reporting at least one past psychiatric hospitalization was over 76% in 2009 and decreased steadily to less than 50% in 2016. As seen in
Figure 2, this decrease appeared primarily related to declines in hospitalizations reported by admissions diagnosed with unspecified schizophrenic spectrum and other psychotic disorder (
![]() $ \chi $
2
= 70.18, df = 14, p = .000). Those diagnosed with a schizophrenia-spectrum disorder (schizophrenia or schizoaffective disorder) reported slight decreases, especially in later years (
$ \chi $
2
= 70.18, df = 14, p = .000). Those diagnosed with a schizophrenia-spectrum disorder (schizophrenia or schizoaffective disorder) reported slight decreases, especially in later years (
![]() $ \chi $
2
= 60.02, df = 14 p = .000). Individuals with a diagnosis of bipolar disorder evidenced fluctuating rates of prior admissions from year to year (
$ \chi $
2
= 60.02, df = 14 p = .000). Individuals with a diagnosis of bipolar disorder evidenced fluctuating rates of prior admissions from year to year (
![]() $ \chi $
2
= 27.89, df = 14, p = .015), although there were notable drops in all diagnostic categories after 2013.
$ \chi $
2
= 27.89, df = 14, p = .015), although there were notable drops in all diagnostic categories after 2013.

FIGURE 2. Percent of admissions reporting at least 1 prior hospitalization.
Admission diagnoses also evidenced an interesting trend, shown in
Figure 3. Patients were more likely to receive a diagnosis of a schizophrenic spectrum disorder in 2009 through 2012 and more likely to receive a diagnosis of unspecified schizophrenic spectrum disorder (formerly psychotic disorder NOS) in later years (
![]() $ \chi $
2
= 214.15, df = 49 p = .000). When these two diagnoses were combined, the percentage with this diagnosis did not evidence substantial differences over time (
$ \chi $
2
= 214.15, df = 49 p = .000). When these two diagnoses were combined, the percentage with this diagnosis did not evidence substantial differences over time (
![]() $ \chi $
2
= 21.63, df = 5, p = .000). The highest percentage was 73.2 in 2014, with the lowest 61.9 in 2015.
$ \chi $
2
= 21.63, df = 5, p = .000). The highest percentage was 73.2 in 2014, with the lowest 61.9 in 2015.

FIGURE 3. Change in admission diagnoses over time.
As seen in
Table 1, gender of the admissions fluctuated over time, even when removing the two years DSH-Napa did not admit females for the entire year (2009 and 2010;
![]() $ \chi $
2
= 60.02, df = 14 p = .000). Generally speaking, the number of women admitted as IST increased over time.
$ \chi $
2
= 60.02, df = 14 p = .000). Generally speaking, the number of women admitted as IST increased over time.
Both age at admission and scores on the BPRS evidenced differences over time, although similar to the competency variable, these changes were reflective of variations from year to year [F(7,3150) = 2.50, p = .015; F(7,2566) = 10.24, p = .000], rather than a steady increase or decrease over time. Age ranged from a low of 37.49 in 2016 to a high of 40.18 in 2014. Similarly, BPRS scores ranged from a low of 8.17 in 2015 to a high of 11.02 in 2009.
Length of stay also evidenced substantial changes over time, as shown in Table 1. The overall length of stay decreased from an average of 345.68 days in 2009 to 162.68 days in 2016 [F(7,3112) = 8.48, p = .000]. The changes were even more striking when the sample was divided into length of stay for those restored to competence versus those deemed not restorable [F(7,2749) = 4.76, p = .000; F(7,305) = 19.45, p = .000, respectively]. Admissions restored to competence showed a steady decrease in length of stay over time, with a slight increase beginning in 2014. In contrast, the length of stay for those determined to be unrestorable evidenced steady decreases, with the LOS in 2016 almost a third the length of stay in 2009.
Length of stay also varied by diagnosis for admissions ultimately restored to competence, as seen in Table 2 (F(9,2415) = 28.10, p = .000. Figure 4 provides a graphic depiction of these differences. Three diagnoses exhibited longer lengths of stay than most other diagnoses: schizophrenic-spectrum disorders, cognitive disorders, and delusional disorders. Not surprisingly, substance use disorders evidenced the shortest lengths of stay, although their average length of stay was not significantly different from bipolar disorder, personality disorders or individuals returned as malingering.
TABLE 2. Discharge length of stay if restored by diagnosis

Note: F(9,2415) = 28.10, p = .000

FIGURE 4. Length of stay by discharge diagnosis for patients restored to competence.
Multiple variables did not change over time. The percentage of admissions believed to be malingering did not evidence statistically significant differences, although the percentages fluctuated for a low of 14.7 in 2016 to a high of 20.0 in 2014 (
![]() $ \chi $
2
= 7.07, df = 7, p = .421). Consistent with this, both scores on the M-FAST and percentage of admissions scoring above the cut point did not evidence statistically significant differences over time [F(7,2009) = 1.28, p = .257;
$ \chi $
2
= 7.07, df = 7, p = .421). Consistent with this, both scores on the M-FAST and percentage of admissions scoring above the cut point did not evidence statistically significant differences over time [F(7,2009) = 1.28, p = .257;
![]() $ \chi $
2
= 7.25, df = 7, p = .403, respectively]. The ethnic distribution of the sample also did not vary over time (
$ \chi $
2
= 7.25, df = 7, p = .403, respectively]. The ethnic distribution of the sample also did not vary over time (
![]() $ \chi $
2
= 5.72, df = 7, p = .573), with ethnic minorities representing close to 62% of admissions in 2009 and less than 54% in 2014.
$ \chi $
2
= 5.72, df = 7, p = .573), with ethnic minorities representing close to 62% of admissions in 2009 and less than 54% in 2014.
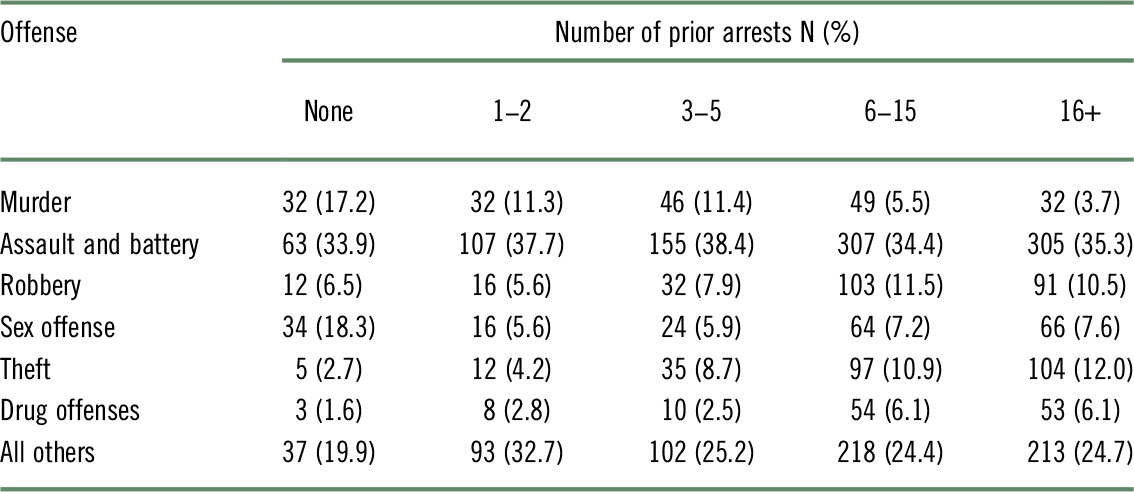
Because we found significant increases in number of prior arrests each year, we examined the relationship between commitment offense and number of prior arrests, categorized as none, 1–2 priors, 3–5 priors, 6–15, and more than 15. As shown in
Table 3 and depicted graphically in
Figure 5, three commitment offenses in particular were associated with prior arrests. Patients committed for theft charges (robbery and theft) evidenced significantly more prior arrests; patients committed for homicide charges had fewer prior arrests (
![]() $ \chi $
2
= 154.46, df = 24, p = 000).
$ \chi $
2
= 154.46, df = 24, p = 000).
TABLE 3. Commitment offense by arrest rates
Note:
![]() $ \chi $
2
= 154.46, df = 24, p = .000
$ \chi $
2
= 154.46, df = 24, p = .000

FIGURE 5. Commitment offense by prior arrest history.
Table 4 provides the diagnoses for those restored to competence versus those who were deemed not restorable. Not surprisingly, two diagnostic categories were least likely to be restored: patients with a schizophrenic-spectrum disorder and patients with a cognitive disorder. Over 40% of those diagnosed with a cognitive disorder were deemed unlikely to regain competence; almost 15% of those with a discharge diagnosis of a schizophrenic spectrum disorder were considered not restorable. These two diagnostic categories comprised almost 90% of the admissions ultimately determined to be unlikely to be restored to competence. Not surprisingly, all individuals discharged with diagnoses of either a personality disorder or malingering were restored to competence.
TABLE 4. Discharge diagnoses by restoration status

Note:
![]() $ \chi $
2
= 241.33, df = 9, p = .000
$ \chi $
2
= 241.33, df = 9, p = .000
DISCUSSION
Our data are consistent with previous studies documenting the characteristics of individuals found incompetent to stand trial. They also provide additional insight into factors contributing to nationwide increases in IST admissions. Perhaps one of the most illuminating findings is the decreasing numbers of IST admissions reporting prior inpatient psychiatric treatment. This result is not surprising given the reported decreased numbers of psychiatric beds in the US, both state and community, since deinstitutionalization began in the 1950s. In 1955, there were over five hundred thousand state psychiatric hospital beds. As deinstitutionalization continued, by 1994, only 71,619 beds remained.Reference Torrey, Kennard, Eslinger, Lamb and Pavle 17 A recent count indicated that in the first quarter of 2016, slightly less than 38,000 beds remain, an astronomical decline of 96.5% in this 60 year time period. 47 Moreover, the majority of these state beds are forensic, Reference Wik, Hollen and Fisher 14 meaning that in order to be admitted for treatment, you must commit a crime. Similar declines have been reported in community inpatient beds, to levels well below international standards and expert consensus guidelines.Reference Torrey, Kennard, Eslinger, Lamb and Pavle 17 , Reference Bastiampillai, Sharfstein and Allison 48
One relevant and likely related finding was the substantial increase over time of IST admissions with extensive criminal arrest histories. Although advancing age was considered as an explanation for this rise, as older defendants potentially have had more time in the community to offend, the age of admissions did not increase over time. As prior arrests accumulate, defendants face increasingly serious charges. In partial support of this notion, we found a significant relationship between number of prior offenses and the commitment offense. Defendants charged with homicide and sexual offenses were much less likely to have extensive criminal arrest histories. In contrast, admissions charged with theft, robbery, or drug offenses all evidenced increasing numbers of prior arrests, a result entirely consistent with data reported by Torrey.Reference Torrey, Kennard, Eslinger, Lamb and Pavle 17 He noted that many individuals with serious mental illness are charged with relatively minor offenses, such as assault and theft.Reference Torrey 49 Additionally, relatively minor offenses may become felonies as the number of prior arrests increase. For example, in California, petty theft becomes a felony when the individual has multiple prior arrests. As Figures 1 and 2 clearly depict, our data show that as arrest rates increase over time, percentages of admissions reporting prior hospitalizations decrease in the same time period.
While it remains unclear from our data if the increasing number of prior arrests and decreasing numbers of patients with prior psychiatric hospitalizations are related, both occurring coincidentally is consistent with the notion that the seriously mentally ill are now receiving services primarily from the criminal justice system, not from the mental health system. As recently as 2010, Torrey and colleagues conducted a study to ascertain where individuals with serious mental illness were receiving their treatment.Reference Torrey, Kennard, Eslinger, Lamb and Pavle 17 The evidence was clear: in the US, the odds of a person with a major mental disorder receiving treatment in a jail or prison instead of a psychiatric hospital was 3.2 to 1. Some states were substantially worse: In Nevada, the odds were 9.8 to 1, an almost 10 times greater likelihood that mental health treatment was provided in jails and prisons. This trend has been evident for the past several years. Combined with previous studies, our data provide information about an additional mechanism for the treatment of individuals with severe mental illness. While still receiving treatment via the criminal justice system, the setting is not a jail or prison; it is commitment in a state hospital.
Our data is entirely consistent with research on the impact of deinstitutionalization: individuals with serious mental illness released from institutions frequently receive mental health treatment via the criminal justice system. In the 1980s, Belcher found that a large number of patients released from a state hospital in Ohio were homeless within 6 months of discharge. Furthermore, almost 45% of those who were homeless had been arrested and incarcerated in that same time period.Reference Belcher 50 Numerous studies have reported high percentages of inmates with major mental disorders, 51-53 with sheriffs across the country lamenting the need to serve as de facto mental health institutions.Reference Ford 54 Consistent with Belcher’s study, research has shown that homelessness has become a national problem 55-57 and a substantial number of these homeless individuals have a severe mental disorder.Reference Roy, Crocker, Nicholls, Latimer and Ayllon 57 , Reference Koegel, Burnam and Farr 58 Often these individuals are arrested for crimes associated with either their mental illness or homelessness. Once arrested, they are so ill due to their untreated disorder, they are found not competent to stand trial. Unfortunately, this cycle is perpetuated, as treatment for individuals found not competent typically is geared exclusively towards competence restoration.Reference Iglehart 59 Once competent, they are returned to jail and when released, no intervention is provided to keep them engaged in mental health treatment and out of the criminal justice system. The decrease in prior hospitalizations reported by our admissions is entirely consistent with the results of our national survey (reported in this issue). The number one reason identified by stakeholders across the country as an explanation for the surge in IST commitments is the lack of general mental health services in the community, followed closely by the lack of intensive community treatment and inpatient beds.
Interestingly, we found that increasing numbers of women were admitted as not competent to stand trial. It is unclear if this reflects an overall increase in the rate of findings of incompetence for women or increasing numbers of women entering the criminal justice system. A recent meta-analysis has shown that women and men are found IST at comparable rates.Reference Pirelli, Gottdiener and Zapf 12 However, the number of women involved in the criminal justice system is growing: between 1980 and 2017, the number of incarcerated women increased by 700 percent. In this same time period, incarceration rates of women grew 50 percent faster than they did for men.Reference Carson 60 It stands to reason if more women are entering the criminal justice system, even with steady rates of findings of incompetency, more women will be deemed IST. Moreover, Steadman and colleagues found that the rate of serious mental illness in incarcerated women is substantially higher than for men.Reference Steadman, Osher, Robbins, Case and Samuels 51 , Reference Teplin, Abram and McClelland 61 This finding, coupled with the increasing arrest rates of women, may be the reason for our observed increasing rates of admissions of women found IST.
Consistent with the literature, patients evidencing the longest time to restore were those with schizophrenic-spectrum and cognitive disorders.Reference Gay, Vitacco and Ragatz 33 , 36-39 In addition, the majority of patients who could not be restored were those with a schizophrenic-spectrum diagnosis (70%), followed closely by individuals with a cognitive disorder diagnosis (18.3%), indicating that almost 90% of patients determined to be nonrestorable fell under those two diagnostic categories. Furthermore, close to half (42.6%) of admissions with a cognitive disorder diagnosis were ultimately deemed unrestorable. Interestingly, patients returned to court as competent with a diagnosis of delusional disorder evidenced lengths of stay comparable to these two disorders. Initially considered a variant of schizophrenia with only delusions, delusional disorder has been the subject of minimal research, largely because of small sample sizes.Reference Peralta and Cuesta 62 Hui and colleagues compared first episode patients with delusional disorder to first episode patients with schizophrenia and found numerous similarities.Reference Hui, Lee and Chang 63 In contrast, Marneros conducted a longitudinal study of patients with delusional disorder and schizophrenia and found distinct patterns of response, symptoms and outcomes between the two disorders.Reference Marneros, Pillmann and Wustmann 64 Herbel demonstrated that the majority (77%) of patients with delusional disorder found IST were restored to competence, although over 50% of these required an extended period of time on medication.Reference Herbel and Stelmach 65 In our sample, patients with a discharge diagnosis of delusional disorder evidenced a similar course of illness to patients with schizophrenic spectrum disorders, as well as a similar percentage who ultimately could not be restored. While our data did not compare characteristics between the two disorders, they suggest that the two diagnoses are comparable at least in regards to restorability and length of time to restoration.
Not surprisingly, individuals returned to court with a primary diagnosis of a personality disorder as well as those believed to be malingering evidenced very short restoration periods and all were “restored” to competence, a result consistent with the literature.Reference Cooper and Zapf 24 , Reference Hubbard, Zapf and Ronan 26 Two additional diagnostic groups evidenced the shortest length of stay: substance use disorders, typically a substance-induced psychotic disorder, and bipolar disorder. Research suggests that individuals receiving a diagnosis of bipolar disorder respond rapidly to medication, Reference Harrison, Cipriani and Harmer 66 which may explain their brief length of stay. Substance induced psychotic disorders typically evidence a remission of symptoms once the substance is withdrawn.Reference McKetin, Gardner and Baker 67 , Reference McKetin, Dawe and Burns 68 Once psychotic symptoms have remitted, patients are generally able to understand criminal proceedings and assist their attorney.
Consistent with previous research, our data indicate that minorities, specifically Blacks, are over-represented in our sample as compared to the ethnic distribution in CA. According to the 2017 census estimate, Blacks comprise 5.47% of the CA population. In our sample, almost 29% were Black, a result similar to the incarcerated population (27% Black). 47 In striking contrast, although Hispanics comprise over 39% of the CA population, they represented only 18.6% of our sample; in contrast, 41% of the incarcerated population is Hispanic. Perhaps more notably, although minorities represent the majority of our admissions, the single largest racial group in our sample was White, at 42.86%. While this is slightly higher than the 37% reported by the CA census, it is substantially lower than the 26% reported in CA jails and prisons. The reasons for these discrepancies are unclear. There is abundant evidence that Hispanics are less likely to seek mental health treatment for a variety of reasons, including mistrust and language barriers.Reference De Luca, Blosnich, Hentschel, King and Amen 69 Additionally, Hispanics are slightly more likely to be homeless, at least compared to non-Hispanic whites.Reference Fusaro, Levy and Shaefer 70 It is unclear if either of these factors is related to the decreased prevalence of Hispanics in our sample. Typically, competence is raised as an issue when the observed mental illness is so severe it impairs the individual’s ability to understand or assist their attorney. Seeking a competency evaluation generally is not in the purview of the defendant.
The pattern of changes in diagnosing over time was of particular interest, most notable the increase in the unspecified schizophrenia diagnosis and the concurrent decrease in the schizophrenic spectrum diagnoses. One explanation for this pattern of diagnosing may lie in the change from the DSM-IV TR to the DSM-5. For this specific disorder, the change was primarily related to the name: psychotic disorder not otherwise specified was renamed unspecified schizophrenic spectrum and other psychotic disorder in DSM-5, although there were slight changes in the definition. A more likely explanation is that increasing substance use, particularly the use of methamphetamine, clouds the picture and course of the disorder, making a definitive diagnosis impossible. Interestingly, as depicted in Figure 2, the group most impacted by the decline in inpatient treatment was individuals diagnosed with unspecified schizophrenic spectrum disorder. This diagnosis is given when an individual is exhibiting psychotic symptoms but does not meet full criteria for schizophrenia. Previous research has suggested that this diagnosis often is associated with either a substance use disorder, specifically a substance-induced psychotic disorder, or malingering, a finding consistent with our data on length of stay.Reference Scott, McDermott and Kile 71 Our survey findings indicate that some believe that the rising use of methamphetamine is related to increasing numbers of IST commitments. It is clear that comorbid substance use disorders are prevalent in individuals with a schizophrenic-spectrum disorder, which exacerbate psychotic symptoms.Reference Hides, Dawe and McKetin 72 With the dwindling availability of inpatient psychiatric beds, individuals presenting with psychotic symptoms and positive toxicology screens may not be admitted, at least until there is a definitive determination that the symptoms exhibited are not substance-induced. Increasingly literature is suggesting that there are discernable differences in substance – induced versus primary psychotic disordersReference McKetin, Baker, Dawe, Voce and Lubman 73 and one of these differences is involvement in the criminal justice system.Reference Fraser, Hides, Philips, Proctor and Lubman 74
CONCLUSIONS
Our data add to the body of literature on the potential causes of the nationwide increase in the competency referrals. Moreover, our results complement the extensive literature on the criminalization of individuals with mental illness since the closing of long-term state hospitals. The literature is clear that individuals with serious mental disorders are not accessing services in the community. Because of this, their mental illness remains untreated and often they are arrested. Jails and prisons are assuming the role of the nation’s mental health provider. Unfortunately, as is generally the case with jails and prisons, once released from custody, very few mechanisms are in place to engage these individuals in community mental health treatment. Our data, and nationwide data, suggest that another system has assumed this role: state hospitals and other providers charged with restoring individuals to competence. It appears that what Belcher found in the 1980s is continuing: once released from a state hospital, individuals with serious mental disorders become (or return to) homelessness and are re-arrested. And the cycle continues.
Acknowledgments
This research was conducted as part of a collaborative effort between DSH-Napa and UC Davis School of Medicine, Department of Psychiatry and Behavioral Sciences, funded by the California Department of State Hospitals.
Disclosure
Barbara McDermott, Katherine Warburton, and Chloe Auletta-Young have nothing to disclose.











