INTRODUCTION
Transitions in care can pose several communication challenges for patients, families and healthcare providers. This time point can also be a source of significant stress for patients, as they try to cope with self-management of symptoms after completing a treatment or a stay in-hospital.Reference Barton, Hudson, Delaney, Gruver and Liu 1 , Reference Tindale 2 Several different groups have developed tools in the form of a patient discharge summary to help alleviate this stress and provide patients and families with a written record of a completed treatment or hospital course.Reference Nekhlyudov and Schnipper 3 When used in the inpatient setting, these summaries often provide patients with record of their hospital stay and clear, concise self-management instructions to be followed after discharge.Reference Barton, Hudson, Delaney, Gruver and Liu 1 , Reference van der Linden, Steenland and van Houwelingen 4 , Reference Moore, Wisnivesky and Williams 5
The North American Nursing Diagnosis Association has highlighted transfers in care as time points that can lead to significant ‘relocation stress’, which can lead to anxiety, depression, feelings of insecurity, and trust and dependency issues.Reference Tindale 2 , Reference Carpenito-Moyet 6 Several groups have studied the impact of a patient discharge summary generated at transfers in care, and have found that providing diagnosis-specific discharge summaries positively affects patient satisfaction and patient safety, improves communication among care providers, empowers patients to better self-manage their symptoms, and results in fewer hospital re-admissions.Reference Tindale 2 , Reference Hall, Keane, Wang, Debell, Allana and Karia 7 , Reference Lo, Diane and Rodriguez 8
For patients receiving radiation treatment, the end of a course of radiotherapy often marks a transition from active treatment, where patients are seen daily by radiation therapists, nurses and oncologists, to a period of follow-up where patient are not coming into the cancer centre on a daily basis. In particular, the 2 weeks following radiotherapy can be associated with increased side effects. In a report published in 2005, the Institute of Medicine recommended that patients completing cancer treatment should be provided with a Survivorship Care Plan to help the transition into follow-up care.Reference Hewitt, Greenfield and Stovall 9 Some of the key components of this care plan include the cancer type, treatments received and the dates of initiation and completion of these treatments, radiation doses delivered, interventions for symptom management, as well as contact information for treatment providers.Reference Hewitt, Greenfield and Stovall 9
Currently, at our institution, patients receive a card on the last day of radiotherapy signed from his/her radiotherapy team which contains site-specific self-management instructions. For patients receiving palliative radiotherapy, follow-up care is often provided by the referring or palliative care physician without a return visit to the radiation oncologist.Reference Lau and Bezjak 10 This time point can also lead to significant stress for patients and families.Reference Tindale 2 , Reference van der Linden, Lok and Steenland 11 , Reference Hernanz, Montero, Fernandez-Lizarbe, Polo and Ramos 12
An automated electronic discharge summary was designed for patients completing radiation therapy to help improve communication between care providers and provide patients with a printed record of treatment.Reference Lau and Bezjak 10 This can then be passed onto other care providers involved in a patient’s circle of care. It has been recognised that patients receiving radiation therapy often travel significant distances to receive care at a cancer centre, therefore these patients can potentially rely on several different emergency departments if they run into difficulty with radiation-induced side effects post-treatment.Reference Lamont, Hayreh and Pickett 13 The discharge summary is intended to also help better direct management of radiation side effects, and provide valuable contact information so that staff from emergency departments can more easily contact the appropriate radiation oncologist.
METHODS
In order to facilitate communication during transitions of care, the discharge summary for radiation therapy included the following information: patient identification, radiation oncologist information, radiation treatment site, total dose delivered, as well as the start and completion dates of radiation treatment. Manual generation of this document can be time consuming and prone to errors during the transcription process, therefore an auto-generated process was favoured. Utilisation of the eSCRIBE function within the current version of the Electronic Health Record, MosaiQ enabled automatic generation of the discharge summary (Figure 1). eSCRIBE is an automated document-creation tool that uses Microsoft WordTM templates to customise specific documents that meet the needs of the department, saving time when creating and editing documents. 14 eSCRIBE allows for numerous merge fields that automatically retrieve information from the patient’s chart during the transcription process. 14
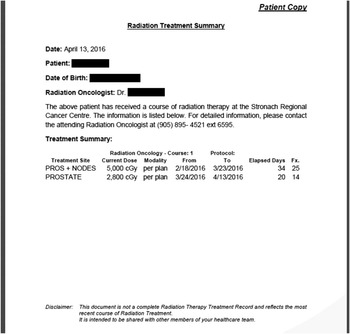
Figure 1 An example of a discharge summary. Date of document creation, patient’s name, patient date of birth, responsible radiation oncologist and radiation treatment summary will be merged automatically from MosaiQ into the document.
In order to ensure the generation and dissemination of the discharge summary to every patient completing radiation treatment, treatment delivery radiation therapists generated and distributed the document to patients on the last day of treatment (Figure 2). This process was designed to minimally impact daily workflow, and as such, generation of the discharge summary currently requires less than one minute. The discharge summary was also automatically captured in the patient’s chart as a permanent document. As described in previous work, our department has implemented radiation oncology care plans and IQ scripts to facilitate daily workflow.Reference Chan, Malam and Loudon 15 The utilisation of these functions allows different tasks to be prompted automatically and safeguards tasks from being missed (Figure 2). An IQ script was created in MosaiQ to facilitate the creation of the discharge summary. Thus, completion of the last day education task triggers a cascade of automated workflow prompts. This forced function allows the discharge summary document to be automatically generated as a standard of practice for all radiation therapy patients.

Figure 2 Flowchart (partial) depicting incorporation of the generation of the discharge summary into the end-to-end radiation therapy workflow.
The discharge summary was piloted with patients receiving palliative radiotherapy (n=22), as it was hypothesised that this patient population has a higher risk of post-radiotherapy emergency department visits than patients treated in the radical setting. A telephone survey was also conducted in which patients were asked multiple questions regarding the discharge summary (Table 1).
Table 1 Summary of pilot questionnaire for palliative radiotherapy patients receiving a discharge summary (n=22)

RESULTS
After conducting the telephone questionnaire, it was reported that 45% of patients surveyed received the discharge summary (Figure 3). Of the 55% of patients who did not receive the document, 8% of patients indicated they lost the summary, 15% of patients had passed away since completing treatment, and 23% were in-hospital at the time of radiation treatment. A retrospective chart review of the remaining 54% of these patients revealed that the summary had not been printed (Figure 3).

Figure 3 Graphs describing distribution of patients who did or did not receive a radiation treatment discharge summary.
For patients who received the summary, 78% stated that the discharge summary was easy to understand and 89% kept a personal copy for their records. A total of 33% of patients forwarded the discharge summary onto another healthcare provider; 9% of this cohort of patients required an emergency department visit post-treatment, and all of these patients reported bringing the discharge summary with them. Patients also suggested that the language on certain parts of the discharge summary should be simplified, which was addressed before rolling out the discharge summary to all radiotherapy patients.
DISCUSSION
Telephone questionnaire
A total of 22 patients who were scheduled to receive the discharge summary were contacted to complete a telephone questionnaire. Nine patients reported receiving the discharge summary, while 13 patients either did not receive the summary or were reported by a family member as having passed away. For patients who had passed away, the questionnaire was not administered, therefore it is hypothesised that some of these patients likely did receive the discharge summary. A small sample of patients also reported that they received the discharge summary, but lost the document.
For patients who did not receive the discharge summary, several reported being inpatients at the time of radiotherapy. When attending treatment appointments, documentation is placed inside a paper-based hospital chart. It was hypothesised that these patients did not receive the discharge summary likely because it was placed in the hospital chart and was not given directly to the patient. As a result of this, the discharge summary has been modified to indicate the document is a ‘Patient Copy’ and two copies are printed for inpatients. One copy is given directly to the patient while the second copy is placed in the hospital chart as part of the medical record.
Integration of discharge summary into daily workflow
The discharge summary was piloted with patients receiving palliative radiotherapy. These patients were contacted for the telephone questionnaire, and received radiotherapy on all treatment units within the Radiation Therapy Department. Therefore, treatment unit staff had to remember to print the discharge summary specifically for this patient population before this process becoming a part of the daily departmental workflow. This resulted in some patients not receiving the discharge summary as it had not been printed. As the discharge summary has been incorporated into the daily workflow for all patients and is an automated process, this issue has been resolved.
Addition of a disclaimer
During the development process, several concerns were raised that the discharge summary might be mistaken for a complete set of previous radiotherapy records. As patients receiving palliative radiotherapy can receive several courses of radiotherapy over time, radiation oncologists and radiation therapists planning further treatment need to request and obtain previous radiotherapy records. This is important to ensure a full understanding of the previous doses delivered to targets and organs at risk. Misinformation here can result in normal tissues and targets being over or under-dosed. As the discharge summary lists how much dose was most recently delivered, but does not comment on dose to organs at risk or show anatomically where the dose was deposited, the department wanted to ensure that the discharge summary does not replace a request for a patient’s previous radiotherapy records.
In addition, patients expressed that they were sometimes overwhelmed by large amounts of information they received about their diagnosis and some had forgotten the purpose of the discharge summary. Therefore a disclaimer was added to the bottom of each discharge summary which states, ‘This document is not a complete Radiation Therapy Treatment Record and reflects the most recent course of Radiation Treatment. It is intended to be shared with other members of your healthcare team’.
Transfer of information
The discharge summary represents a transfer of information process among healthcare providers, which helps to reduce the risk of miscommunications. The use of a template to generate the document facilitates a standardised approach to communicate radiation treatment information and ensures that the necessary information is conveyed. Upon generating the discharge summary, an electronic copy of the document is also automatically saved into the patient’s electronic chart as a record that it was generated. The document is identified as ‘Patient Copy’, and the patient is encouraged to bring the printed copy of the document when visiting other healthcare providers. Should another member of the patient’s healthcare team have any questions, regarding the radiation treatment received and its impact on any care provided, the document provides clear contact information to consult with the patient’s radiation medicine team.
Patient family and advisory council
As the intention of the discharge summary was to provide patients with a physical record of their radiation treatment, input regarding the content of the document was also sought from the Patient and Family Advisory Committee (PFAC) of the Cancer Centre. Suggestions were consolidated with feedback gathered during the pilot. This feedback was used to further guide revisions to the document before implementing the initiative broadly to all patients receiving radiation therapy treatment. Overall, the discharge summary was viewed positively by the PFAC. There were general comments regarding the language of the document, such as referring to the ‘Attending Physician’ as ‘Radiation Oncologist’, and the order that the information was presented. These changes were easily implemented. A suggestion was also made to add a statement to remind patients of the document’s purpose. The rationale was that over time, patients may not remember that the discharge summary was intended to be shared with other healthcare providers, if needed. As noted above, this was also expressed by patients during the telephone questionnaire. As such, a line specifying the purpose of the document was added as part of the disclaimer to the template of the discharge summary.
Although this study was designed as a pilot, there were a few limitations encountered. The sample size for the telephone questionnaire was small, which was attributed to the nature of the study population. Conducting research with patients who are undergoing palliative treatment can be particularly challenging, as they often are not feeling well and also have varying life expectancies. Although the telephone questionnaire was specifically designed to be short so as not to pose a significant burden on patients, some patients did not feel well enough to provide answers. At the time the telephone questionnaire was administered, it was discovered that several patients’ conditions had deteriorated and other patients had passed away.
CONCLUSION
Care transitions can pose significant challenges in communication for healthcare professionals, patient and families.Reference Barton, Hudson, Delaney, Gruver and Liu 1 , Reference Tindale 2 For patients receiving radiotherapy, a significant transition of care often occurs at the completion of radiation treatment. Literature has shown that development of a discharge summary can help alleviate stress for patients while improving compliance by providing concise discharge instructions.Reference Barton, Hudson, Delaney, Gruver and Liu 1 , Reference van der Linden, Steenland and van Houwelingen 4 The discharge summary can also provide patients with a communication tool should further medical management be necessary during a time when radiation-induced side effects can become more prominent.
Future directions for this initiative involve incorporating other aspects of patients’ care into the discharge summary. For example, it was queried whether chemotherapy treatment information could be included with the discharge summary. This would provide the patient with a consolidated document of any chemoradiation treatment received into a broader ‘Treatment Summary’. Although this was perceived as important information to include within the document, including chemotherapy information presented challenges. There was a logistical challenge, regarding when the document should be generated, as the completion dates for chemotherapy and radiation treatment were often different. There was also a technical challenge, as more work was required to understand the process of extracting medical oncology information into the treatment summary. As a result, the addition of chemotherapy information was determined to be outside the scope of this project, but was highlighted as a future direction to enhance the discharge summary.
Overall, the implementation of a discharge summary for patients completing radiotherapy was well-received by patients. It has allowed for improved communication between different healthcare facilities and providers, while also providing the patient with a record of completion of treatment. The discharge summary was also developed with careful consideration of work load for radiation therapy staff. Automation and integration of the electronic discharge summary into the daily workflow for all patients has made the entire process very user-friendly and has not disrupted efficiency or daily workflow on radiation treatment units. This has enabled this initiative to also be very well-received by radiotherapy staff. Currently, the discharge summary has been rolled out to all patients receiving radiotherapy and has been integrated into regular workflow within the Radiation Therapy Department.
Acknowledgement
Thank you to the Radiation Medicine Team for their continued support of this project.
Financial support
This research received no specific grant from any funding agency, commercial or not-for-profit sectors.
Conflicts of Interest
None.
Ethical Standards
As this work is considered a quality initiative/project, the authors assert that all procedures contributing to this work were reviewed by the Chair of the Institutional Research Ethics Board (REB). The Chair has issued a formal letter confirming that this study does not constitute research involving humans as defined under Article 2·5 of the Tri Council Policy Statement (TCPS2 2014) – Ethical Conduct for Research Involving Humans, and therefore does not fall under the scope of REB review and approval, however, regular administrative and/or other approvals as required by institutional policy/procedures were sought as appropriate.







