Introduction
Endoscopic nasal surgery has gained wide acceptance as a safe treatment modality for chronic sinus disease.Reference Stammberger1, Reference Kennedy2 It enables a minimally invasive approach, reducing patient morbidity. New instruments for endoscopic nasal surgery continue to be introduced in an attempt to reduce the problems associated with ‘grabbing’ tools, which essentially tear tissue and strip mucosa. However, accessing areas that can only be visualised with 30° and 70° endoscopes remains one of the most difficult challenges in this field.Reference Orsel, Sauvage, Puyraud and Bessede3 Such access limitations can cause difficulties when dealing with pathology on the lateral and anterior maxillary sinus walls, such as the base of an antrochoanal polyp or a transitional cell papilloma.
An endoscopic Caldwell–Luc technique has been utilised by the senior author for many years and is minimally invasive.Reference Yanagisawa, Coelho and Yanagisawa4, 5 It offers a potential advantage over traditional approaches, and has not previously been described in the UK literature.Reference Anselmo-Lima, Demarco, Asato and Prado6
Surgical technique
Appropriate pre-operative vasoconstriction of the nose is performed with the patient under general anaesthetic. Pathology within the nasal cavity is first addressed. If this extends into the maxillary sinus, as may occur with an antrochoanal polyp or transitional cell papilloma, an uncinectomy combined with a middle meatal antrostomy is performed to allow visualisation of the sinus.
Local anaesthetic with adrenaline is then infiltrated beneath the upper lip, over the site of the canine fossa. A 5 mm trocar with sheath is then inserted into the maxillary sinus via the canine fossa, parallel to the nasal floor, with a finger extended along its shaft to prevent deep penetration through the posterior wall (Figure 1). The trocar is removed, leaving the sheath in place, which is gently rotated to widen the bony hole. The maxillary sinus can be inspected using a 4 mm, 0° endoscope introduced through the sheath. The sheath is then removed and a microdebrider inserted with its suction tip closed. The assistant temporarily supports the microdebrider with its tip in the maxillary sinus whilst the surgeon re-inserts a 30° or 70° telescope into the nose (Figure 2). This allows a view, through the middle meatal antrostomy, of the tip of the instrument in the maxillary sinus (Figure 3). The surgeon can now deal with pathology in the maxillary sinus. In order to access more awkward areas, such as the anterior wall, it is important to ensure that the microdebrider is not gripped by the bony hole formed by the trocar. If it is, the trocar and sheath should be re-introduced so that the sheath can be rotated to further enlarge the bony hole. This allows sufficient movement for the suction tip of the microdebrider to be rotated and placed directly over the area of pathology to be removed.

Fig. 1 Operative photograph showing trocar introduced through canine fossa.

Fig. 2 Operative photograph showing combined approach technique, with the endoscope inserted through the right nostril and the powered microdebrider inserted through the canine fossa into the right maxillary sinus.
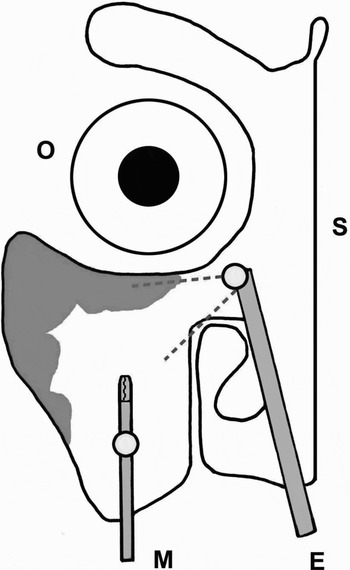
Fig. 3 Diagram showing removal of antral pathology with a 70° endoscope, viewed through the middle meatal antrostomy. O = right orbit; S = septum; M = microdebrider; E = endoscope
One area of potential concern with this technique is injury to the infra-orbital nerve. Extra care must be taken when using instrumentation on the superior wall of the sinus, as the nerve is not always protected within a bony canal. We would suggest that mucosa in this area is removed with caution, and that the microdebrider should be ‘pulsed’ to prevent suction of the nerve into the lumen.
Over the last two years, this technique has been used successfully in 10 patients under the care of the senior author. Five of these patients underwent surgery for removal of an antrochoanal polyp, three had transitional cell papilloma, and the remaining two had dental or unilateral chronic sinus pathology. The average time taken to perform the procedure was 38 minutes (range, 19–55 minutes). Seven of the 10 procedures were performed as day cases. No patients experienced major complications, such as infra-orbital nerve injury or oro-antral fistula. The post-operative appearance of the antral wall at six to eight weeks revealed healthy mucosa in all patients. One patient with transitional cell papilloma required surgery for recurrence after six months.
Discussion
This endoscopic Caldwell–Luc technique offers a simple, effective means of dealing with pathology in inaccessible areas of the maxillary sinus when approached from the nasal cavity. The 5 mm trocar and sheath are inexpensive and are often included in endoscopic sinus instrument sets. The additional cost of extra equipment is therefore negligible. The operative time for this procedure would appear to be no longer, and perhaps shorter, than that for an ‘open’ procedure for removing pathology from the maxillary sinus.
Formal Caldwell–Luc procedures are widely acknowledged to be associated with a high incidence of post-operative complaints (i.e. pain, facial numbness, localised swelling and bleeding).Reference Lund, Rowe-Jones and Gleeson7, Reference Bolger, Kennedy and Kennedy8 However, the endoscopic Caldwell–Luc technique described above offers several benefits to the patient, including surgery as a day case, lower post-operative morbidity and reduced recurrence of disease.





