Catheter-associated urinary tract infections (CAUTIs) occur frequently in inpatients, leading to morbidity and mortality.Reference Mak and Kuo1–Reference Umscheid, Mitchell, Doshi, Agarwal, Williams and Brennan9 They are a common healthcare-associated infection (HAI); they prolong the length of stay and cost >US$400 million annually in the United States.Reference Klevens, Edwards and Richards10–Reference Saint12 These HAIs are less well studied in children,Reference Davis, Colebaugh and Eithun5 with CAUTI incidence ranging from 1 to 5 per 1,000 catheter days.Reference Davis, Colebaugh and Eithun5,Reference Alten, Rahman and Zaccagni13,Reference Brilli, McClead and Crandall14 The CAUTI incidence in a national network of children’s hospitals is 1.07 per 1,000 catheter days.15
Pediatric patients also require indwelling catheters or clean intermittent catheterization (CIC) as outpatients, putting them at risk for ambulatory CAUTIs.Reference Larijani, Moghtaderi, Hajizadeh and Assadi16–Reference Jewes, Gillespie and Leadbetter19 Less is known about ambulatory CAUTIs because of coding and reporting discrepancies, difficulty identifying urinary catheter use in the ambulatory setting, and interpretation of ambulatory cultures.Reference Meddings, Saint and McMahon20–Reference Tieder, Hall and Auger22 Approximately 3% of community dwelling elderly adults and 5%–7% of nursing home residents use indwelling catheters, and bacteriuria is the most common complication.Reference Madigan and Neff18,Reference Jewes, Gillespie and Leadbetter19,Reference Bardsley23–Reference Tsan, Langberg and Davis26 Adult home-health CAUTI rates range from 2.7 to 4.5 per 1,000 device- days,Reference Weber, Brown, Huslage, Sickbert-Bennett and Rutala27,Reference Rosenheimer, Embry, Sanford and Silver28 and ambulatory adults requiring CIC have shown UTI rates of 2.27 infections per subject year.Reference Prasad, Cevallos, Riosa, Darouiche and Trautner29 Risk factors associated with ambulatory CAUTI, outcomes following ambulatory CAUTI, and ambulatory CAUTI incidence in children are unclear.
Given the number of ambulatory children using indwelling catheters or CIC, pediatric ambulatory CAUTIs need to be investigated further.Reference Larijani, Moghtaderi, Hajizadeh and Assadi16–Reference Jewes, Gillespie and Leadbetter19 In this study, we sought to determine the incidence of pediatric ambulatory CAUTIs, associated risk factors, and health outcomes in a retrospective, multisite epidemiologic analysis.
Methods
Setting and study design
This retrospective analysis was performed in 5 urban, pediatric, tertiary-care academic medical centers. These institutions were brought together as part of the New York City Clinical Data Research Network (NYC-CDRN).Reference Kaushal, Hripcsak and Ascheim30 The NYC-CDRN organized the creation of the electronic queries described below although all queries were run at the 5 individual sites on their site specific databases. All pediatric patients <22 years oldReference Hardin, Hackell, Committee On and Ambulatory31 with ambulatory visits between October 1, 2010, and September 30, 2015, were eligible for inclusion. The final date was the last day the International Statistical Classification of Diseases and Related Health Problems, Ninth Revision (ICD-9) codes were in use.
Potential patients were identified through 3 electronic queries of demographic characteristics, billing codes, and laboratory results. The complete query parameters are listed in the Appendix (online). The first query identified children with ICD-9 codes for CAUTIs or complications due to catheters billed in ambulatory settings or within 48 hours of hospital admission. The second electronic query identified patients who had a positive urine culture and either a diagnosis of neuromuscular disease, urinary disease, cerebral palsy, or vesicoureteral reflux or an ICD-9 code or current procedural terminology (CPT) code for catheter insertion, removal, or usage. The third electronic query identified patients who had an ICD-9 code or CPT code for urinary catheter insertion, removal, or usage. The second query excluded patients in the first query, and the third query excluded patients in the first 2 queries.
For all patients identified by the electronic queries, electronic health record (EHR) chart reviews were completed by chart abstractors to screen for urinary catheter usage and CAUTIs in the ambulatory setting at any time during the study window (using the CAUTI definition described below). Risk factors and outcome data were entered into a REDCap database.Reference Harris, Taylor, Thielke, Payne, Gonzalez and Conde32 Each patient’s first CAUTI event in the study window was matched with a control (up to 1:3). We tried to match all case patients with at least 1 control patient before a second control patient could be matched with any case patient. Control patients had an ambulatory catheter but did not experience a CAUTI and were matched to case patients by (1) their primary urinary catheter-related diagnosis ICD-9 diagnostic code group, (2) study site, and (3) the presence of a urinary catheter coincident in time with the case patient’s CAUTI. Chart abstractors identified a patient’s primary diagnosis that led the patient to need a urinary catheter, and this primary diagnosis was grouped into 1 of 17 top-level ICD-9 diagnostic code groups.33 This matching scheme accounted for changes in prevention strategies throughout the study window, but it allowed for broad assessment of potential risk factors. Additionally, by examining each patient’s first CAUTI in the study window, we reduced the risk of bias from patients who had >1 CAUTI.
Definitions
For this study, we modified the National Healthcare Safety Network (NHSN) 2015 CAUTI definition34 to include catheters present in the ambulatory setting (positive urine culture collected >48 hours after discharge or less than or equal to 48 hours after admission) and to include patients requiring CIC. Patients who did not catheterize via a native urethra were excluded. The 4 chart abstractors, all at the same institution, were able to access EHRs online and were trained to adjudicate CAUTIs by a single pediatric hospital epidemiologist who was part of the research team (L.S.). They frequently shared adjudication questions with each other, the lead investigator (M.L.R.), and the hospital epidemiologist.
Ambulatory CAUTI incidence is presented as CAUTIs per 1,000 ambulatory catheter days. A catheter day was any day a urinary catheter was present or CIC was performed in the ambulatory setting. If catheter insertion or removal dates were not clear in the chart, abstractors used date(s) of the first or last note or billing code referencing the catheter. If the insertion date was before the start of the study, cases were excluded from the time from insertion to CAUTI analysis but were included otherwise. Potential risk factors were based on literature reviews and expert consensus (Table 3). Outcomes for pediatric ambulatory CAUTIs were similarly chosen (Table 4). Outcomes were reviewed during the 30 days following CAUTI. Complex chronic conditions (CCCs) were defined as “any medical condition that can be reasonably expected to last at least 12 months … and to involve either several different organ systems or 1 organ system severely enough to require specialty pediatric care and probably some period of hospitalization in a tertiary care center.”Reference Feudtner, Christakis and Connell35 Nonprivate health insurance includes all patients that are not enrolled with private insurance companies, such as those enrolled in Medicaid, CHIP, Medicare, or military insurance or self-insured patients.
Statistical analysis
Descriptive statistics were used to assess CAUTI incidence, risk factors, and outcome data. Descriptive statistics present CAUTI incidence among ICD-9 diagnostic code groups aggregated from the underlying diagnoses that led to urinary catheterization and the most common underlying diagnoses that led to urinary catheterization. To test our hypothesis that indwelling catheters carry a greater risk for ambulatory CAUTI than CIC, we calculated the CAUTI incidence rate ratio (IRR) comparing the 2 methods of catheterization, and we applied a Poisson regression model to test its significance. We performed bivariate exact conditional logistic regression analyses to identify risk factors for CAUTI comparing patients with an initial CAUTI in the study window versus matched control patients. Conditional regression does not require a fixed number of matched controls per case.Reference Kleinbaum and Klein36 A multivariate, exact conditional, logistic regression model was developed, including in a full model of risk factors that includescatheter type.Reference Kleinbaum and Klein36 CAUTI outcomes are presented for all CAUTIs in the study window (ie, unique patients with >1 CAUTI are included more than once) and for initial CAUTI in the study window. A Kaplan-Meier curve was used to determine time to ambulatory infection for indwelling catheters with appropriate censoring when catheters were removed or when CIC was stopped for nonambulatory CAUTI reasons. For those categories with <10 patients, exact 95% confidence intervals were calculated; normal approximations were used in other instances. Statistical analyses were completed using SAS version 9.4 software (SAS Institute, Cary, NC). This study was approved by the Biomedical Research Alliance of New York (BRANY) and by the individual institutional review boards of the participating sites.
Results
Electronic queries from the 5 participating sites over 5 years yielded 3,598 unique patients, including 600 patients from the first query using ICD-9 codes for infection, 1,386 from the second query using positive urine cultures and either relevant diagnoses or codes for catheter usage, and 1,612 from the third query using codes for catheter usage (Fig. 1).

Fig. 1. Flow Diagram of Patients Entered into the Study 2010-2015.
CAUTI incidence
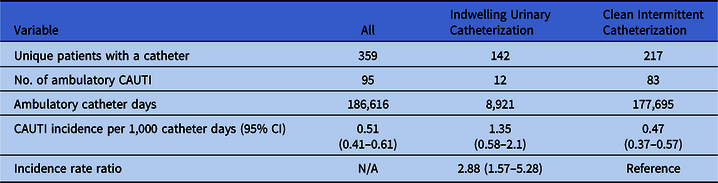
Manual chart review revealed that 359 of the 3,598 patients (10%) identified by the electronic queries had an ambulatory urinary catheter, comprising 186,616 ambulatory urinary catheter days. Moreover, 177,695 ambulatory urinary catheter days (95%) occurred in children with CIC. In addition, 63 patients (18%) experienced 95 ambulatory CAUTIs, for an ambulatory CAUTI incidence of 0.51 CAUTI per 1,000 catheter days (95% CI, 0.41–0.61). As presented in Table 1, the indwelling catheter CAUTI incidence was 1.35 per 1,000 catheter days (95% CI, 0.58–2.1) and the CIC CAUTI incidence was 0.47 per 1,000 catheter days (95% CI, 0.37–0.57), for an IRR of 2.88 (95% CI, 1.57–5.28; P = .0006). Furthermore, 5% of patients experienced ≥2 CAUTIs during the study period: 11 patients experienced 2 CAUTIs, 5 patients had 3 CAUTIs, 1 patient had 5 CAUTIs, and 1 patient had 8 CAUTIs.
Table 1. Total, Indwelling, and Clean Intermittent Catheterization Pediatric Ambulatory CAUTI Incidence per 1,000 Catheter Days

Note. CAUTI, catheter-associated urinary tract infection; CI, confidence interval; N/A, not available.
Table 2 presents CAUTI incidence by ICD-9 diagnostic code groups aggregated from the underlying diagnoses that led to urinary catheterization and the most common underlying diagnoses that led to urinary catheterization. The highest incidence was seen in ICD-9 diagnostic code groups of complications of pregnancy, childbirth, and the puerperium (10.75 CAUTIs per 1,000 catheter days) and endocrine, nutritional and metabolic diseases, and immunity disorders (3.81 CAUTIs per 1,000 catheter days), although both categories had relatively fewer catheter days. The highest incidence by underlying diagnosis occurred in patients with hypospadias (2.85 CAUTIs per 1,000 catheter days) and prune-belly syndrome (2.72 CAUTIs per 1,000 catheter days). The diagnosis of spina bifida was associated with the most catheter days, and these patients experienced a CAUTI incidence of 0.45 CAUTIs per 1,000 catheter days.
Table 2. Pediatric Ambulatory CAUTI Incidence per 1,000 Catheter Days by Diagnosis that Led to Urinary Catheterization
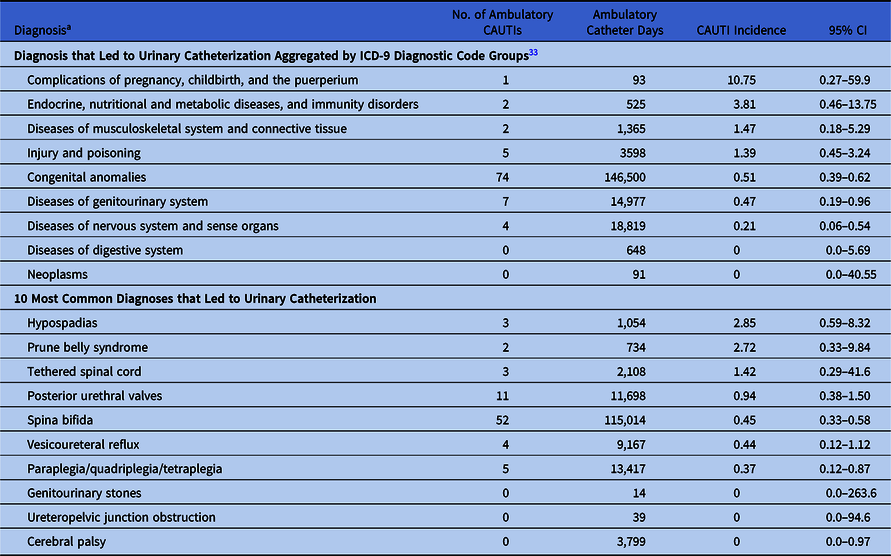
Note. CAUTI, catheter-associated urinary tract infection; CI, confidence interval.
a Diagnoses are ordered by decreasing CAUTI incidence.
Table 3. Risk Factors for Pediatric Ambulatory CAUTI in Bivariate Case-Control Analysisa

Note. CAUTI, catheter-associated urinary tract infection; CI, confidence interval; SD, standard deviation; Ref, reference; ICU, intensive care unit; ED, emergency department; ANC, absolute neutrophil count.
a Missing data varied by risk factor, so total no. varies. No variables were significantly associated with ambulatory CAUTI in multivariable analysis; the results are presented in the text.
b Only 53 of the 63 unique patients with ambulatory CAUTI were able to be matched to control patients.
c Did not include in multivariable model because 59% of patients had missing values.
d Variables without any positive cases or controls: neutropenic (ANC<500) within 30 d. Variables occurring in <3 cases or controls and not associated with ambulatory CAUTI (abnormal albumin within 30 d) (P = degenerate).
Table 4. Outcomes for All CAUTIs in Window and Unique Patients’ First CAUTI in Windowa
Note. CAUTI, catheter-associated urinary tract infection; IQR, interquartile range; ICU, intensive care unit; ED, emergency department.
a Missing data varied by outcome, so total no. varies.
b All CAUTI patients were discharged home and there were no mortalities in the 30 days following CAUTI.
c 1 patient required vasopressors for hypotension in each group.
d Patients may have received >1 imaging modality; no patients received interventional radiology imaging or a voiding cystourethrogram.
Risk factors
Of the 63 unique patients with a CAUTI, 3 control patients were matched to 22 case patients (35%); 2 control patients were matched to 12 case patients (19%); 1 control patient was matched for 19 case patients (30%); and zero control patients were matched for 10 case patients (16%). Of the 10 unmatched cases, 4 had indwelling catheters and 6 had a CIC. In the bivariate logistic regression analyses (Table 3), patients with nonprivate medical insurance (odds ratio [OR], 2.5; 95% confidence interval [CI], 1.1–6.3) had significantly increased odds for an ambulatory CAUTI. In addition, 3 other variables, body mass index (BMI), non-English preferred language, and premature birth had P < .075 in the bivariate analyses; BMI was not included in the multivariate analysis because 59% of patients had missing values for this risk factor. No risk factor had odds that were significantly associated with ambulatory CAUTIs in the multivariable model including non-private insurance status (OR, 2.0; 95% CI, 0.78–5.4), non-English preferred language (OR, 1.7; 95% CI, 0.55–5.5), or premature birth (OR, 2.2; 95% CI, 0.73–6.8). These results did not appreciably change when catheter type (CIC vs indwelling), which was not a matching variable, was included in the model.
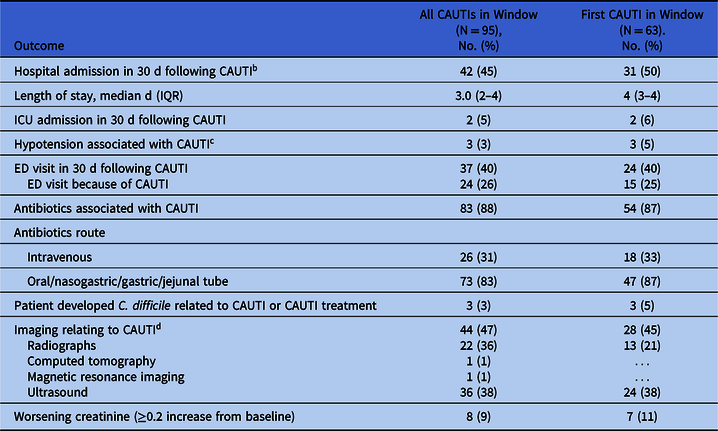
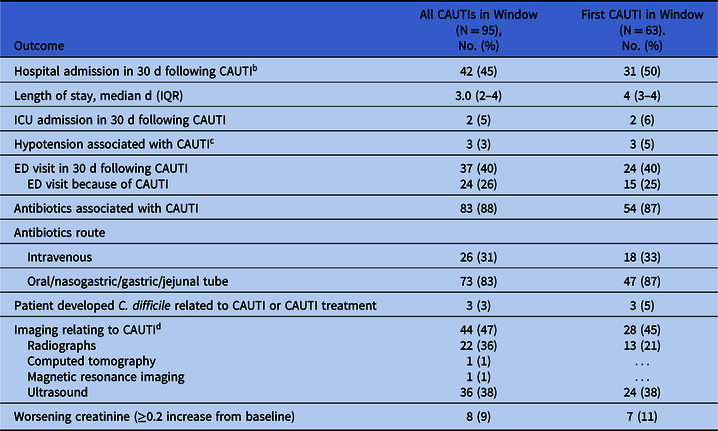
Outcomes for all CAUTIs in the study window
When considering all ambulatory CAUTI in the study window (n = 95), 45% of patients were hospitalized in the 30 days following their CAUTI and had a median length of stay of 3.0 days (IQR, 2–4). Moreover, 5% of patients required intensive care and 3% of patients were diagnosed with Clostridioides difficile infection in the 30 days following their CAUTI. Furthermore, 88% of patients received antibiotics associated with their CAUTI; 31% of whom received intravenous antibiotics. Also, 47% of patients underwent imaging associated with their CAUTI. No case patients had evidence of bacteremia, perinephric abscesses, or acute kidney injury according to the risk, injury, failure, loss of kidney function, and end-stage kidney disease (RIFLE) criteria.Reference Bellomo, Ronco and Kellum37 Finally, 10 case patients (16%) had a second CAUTI, separated in time, that was caused by the same microorganism cultured during their first CAUTI. The most common organisms isolated in urine cultures were Escherichia coli (63%) and Klebsiella pneumoniae (13%). Table 4 presents additional outcome data for all patients and for the 63 unique patients’ first CAUTI in the study window.
Time to infection for indwelling catheters
The Kaplan-Meier survival analysis of time to ambulatory CAUTI for patients with indwelling catheters presents frequent occurrences of infection within the first 40 days, after which only 1 infection occurred at day 705, with >70% survival probability with no infection (Fig. 2).

Fig. 2. Kaplan Meier Survival to Ambulatory CAUTI for Patients with Indwelling Catheters.
Discussion
In one of the first multisite studies to assess the burden of pediatric ambulatory CAUTIs, including the burden associated with CIC-related CAUTI, we identified a CAUTI incidence of 0.51 CAUTI per 1,000 catheter days. Patients using indwelling catheters had 2.9 times higher incidence of CAUTI than those using CIC, and they experienced an ambulatory CAUTI on average every 743 days at risk. No variables were identified as risk factors for CAUTIs in a multivariable model. Morbidity and healthcare utilization associated with CAUTIs were notable; 45% of all ambulatory CAUTI patients were hospitalized within 30 days of their CAUTI, including 5% admitted to an ICU, and 3% of patients developed C. difficile. These results suggest that pediatric ambulatory CAUTIs frequently occur and have associated morbidity, meriting further focus on defining, tracking, and reducing these infections.
A national network of children’s hospitals identified 1.07 CAUTIs per 1,000 indwelling catheter days in pediatric inpatients in 2018.15 In contrast, the pediatric ambulatory CAUTI incidence associated with indwelling catheters in this study (2010–2015) is 1.35 per 1,000 catheter days. Given the focus on inpatient pediatric CAUTI reduction, this study’s comparable pediatric ambulatory CAUTI incidence suggests that the risk of infection associated with urinary catheters used in ambulatory setting also merits reduction efforts. However, unlike the NHSN inpatient CAUTI definition,34 our catheter definitions included patients requiring CIC, who constituted 95% of pediatric ambulatory CAUTI at-risk catheter days in this study (177,695 of 186,616) occurred in patients using CIC. Based on the large number of at-risk CIC days, researchers and policy makers could consider including patients using CIC in CAUTI definitions, surveillance, and prevention efforts.
Notably, only 10% of patients in this study with relevant ambulatory ICD-9 and CPT codes had ambulatory indwelling or CIC catheters upon chart review. Thus, any work aimed at reducing ambulatory CAUTI would need to be supported by improved billing and coding efforts as well as increased ambulatory catheter surveillance. Although this resource investment may be daunting, we hypothesize that it is comparable to the resources required at the initiation of inpatient CAUTI surveillance. We further hypothesize that the sensitivity and specificity of ICD-10 codes for HAIs are similarly poor, but our data do not speak to this specifically.
When designating limited resources to ambulatory CAUTI reduction, it is important to target key ambulatory CAUTI risk factors. Risk factors for adult inpatient CAUTI include female sex, older age, neutropenia, and paraplegia.Reference Lo, Nicolle and Coffin38,Reference Letica-Kriegel, Salmasian and Vawdrey39 Risk factors for pediatric inpatient CAUTIs after congenital heart surgery have been identified as congenital abnormalities of the kidney and urinary tract.Reference Kabbani, Ismail and Fatima40 Hospitalized children who were diagnosed with CAUTIs were more likely to be female (75%) and to have complex chronic conditions (98%).Reference Davis, Colebaugh and Eithun5 We did not identify any risk factors for pediatric ambulatory CAUTIs in a multivariable model. The lack of significant associations may be due to insufficient power; even with 5 academic medical centers over 5 years, only 63 unique patients with ambulatory CAUTIs were identified and only 53 were able to be matched to controls. Furthermore, research in disease-specific groups may be required to identify risk factors because the risk factors for ambulatory CAUTI may differ in children with different pathophysiologies of disease. Although patients with nonprivate insurance are reasonable first targets for reduction efforts, national research can help identify more definitive pediatric risk factors for ambulatory CAUTI reduction interventions.
This study has several limitations. Most importantly, misclassification bias is possible across various domains of the study. Charting and coding was not consistent across the EHRs of these 5 institutions, and each site ran the queries on their site-specific databases, creating additional opportunities for variation. Efforts were made to train, standardize and monitor chart reviews from the data abstractors, but variation is always possible among 4 abstractors. Data abstractors were not certified infection preventionists, but a hospital epidemiologist did provide training and was available for CAUTI adjudication questions. Additionally, patients may have been colonized with bacterial organisms instead of experiencing true infection and CAUTI, and pregnant women with short-term catheterizations may have been included. Outcomes of patients may be unrelated to CAUTIs and just occurring frequently due to catheter-associated diagnoses in these patients. The NHSN definition for CAUTI was not developed for ambulatory catheters or for patients using CIC. Some patients with ambulatory urinary catheters may not have been identified by our electronic searches, although we believe this is less likely given the broad search strategies we used. Similarly, it is possible that retrospective chart review over- or under-estimates the number of catheter days, which would skew the incidence estimates presented in this manuscript. Our case-control matching schema did not identify any control patients for 16% of cases and identified only 1 control patient for 30% of patients. Patients with rare diagnoses, therefore, may have been underrepresented in our risk-factor analyses. Finally, all sites were tertiary-care, academic, pediatric medical centers, and it is unlikely these results are generalizable to non–tertiary-care centers. We believe that most patients with long-term ambulatory catheterization are followed in tertiary-care centers.
In conclusion, pediatric ambulatory CAUTI incidence is comparable to pediatric inpatient CAUTI incidence. This incidence varies by diagnosis and type of urinary catheterization used. These infections lead to patient morbidity, and more research is needed to understand and validate risk factors for pediatric ambulatory CAUTIs. Efforts should be focused on developing standardized ambulatory CAUTI case definitions and promoting strategies to reduce these infections.
Supplementary material
To view supplementary material for this article, please visit https://doi.org/10.1017/ice.2020.204
Acknowledgments
None.
Financial support
The authors were supported by the Agency for Healthcare Research and Quality (grant no. R01HS24432).
Conflicts of interest
No authors report a potential conflict of interest.