The severe Ebola outbreak in West Africa has proven to be the worst in history and has required vast efforts from health care workers (HCWs). 1 HCWs are presented with the challenge of not only caring for their patients but also caring for themselves by minimizing their exposure to potential transmission of the Ebola virus. Personal protective equipment (PPE) provides HCWs with a barrier to prevent human contact with viruses like Ebola and potential transmission of the disease via mucous membranes such as in the nose, mouth, and eyes or disruptions in the skin such as cuts, scrapes, or cracked skin.Reference Fischer, Hynes and Perl 2 Additional protection is provided to HCWs via a respiratory protective device to prevent airborne transmission of the virus during aerosol-generating medical procedures.
While PPE provides advantageous protection from the transmission of viruses to the HCW, it can also introduce an additional physiological burden from potentially increased heat stress. The semipermeable or impermeable nature of some of the PPE reduces the wearer’s ability to stay cool by decreasing the body’s ability to release heat through the normal physiological strategies of sweat evaporation, convection, and radiation. In addition, the wearer experiences increased physiological burden because he or she must bear the extra weight of the PPE (3.8–4.2 kg), which can increase workload and heat generation compared to normal working clothes. Because of the increased heat stress experienced in West Africa, HCWs may not be able to work continuously for longer than 40 minutes in one bout.Reference Wolz 3 , Reference Chertow, Kleine and Edwards 4 Possible solutions, such as frequent shift rotation and cooling periods throughout the workday, have practical limitations in disease control and response work such as encountered in West Africa. Frequent donning and doffing of PPE, for increased breaks and cooling periods, potentially increase the risk of contamination for HCWs. High patient loads reduce the staff’s schedule flexibility for cooling periods or similar strategies. Finally, the limited availability of single-use PPE limits the number of PPE changes that can be completed throughout the day. These specific PPE challenges extend beyond HCWs who are working on Ebola relief to workers in industries such as infection control, construction, agriculture, hazardous materials response, manufacturing, and wildland firefighting who wear PPE ensembles with similar characteristics.Reference Applebaum, Graham and Gray 5
While proper protection from viral contamination must be prioritized, the possible burden of heat stress that may accompany certain PPE must be considered. Heat stress can lead to decreased physical performance and increased risk for heat-stress-related injuries.Reference Cheuvront, Kenefick and Montain 6 To ensure continued proper use of PPE and the safety of HCWs from heat stress, a greater understanding of the heat stress presented by various types of PPE must be developed. The materials chosen for different types of PPE attempt to balance the physiological burden with protection from viral contamination. Generally, an impermeable clothing layer would provide the greatest protection from viral contamination. However, a completely impermeable PPE clothing layer would greatly increase the heat stress to the wearer.Reference Coca, DiLeo and Kim 7 , Reference Potter, Gonzalez and Xu 8 A balance must be achieved between these 2 variables to minimize heat stress as well as the potential for contamination. It is vital to understand the heat stress properties of various garments to make educated decisions about this practical balance.
The purpose of this study was to evaluate the human physiological and subjective responses to continuous light exercise within environmental conditions similar to those in West Africa while wearing 3 different, commonly used PPE ensembles.
MATERIALS AND METHODS
Subjects
Six healthy male subjects (height=1.84±0.09 m, weight=75.05±10.27 kg, body mass index [in kg/m2]=22.15±2.31) completed a general health screening by a licensed physician and were cleared for exercise testing. All subjects were given orientation to the testing protocol, the purpose of the study, and any potential risks involved with their participation before beginning testing. The study was approved by the National Institute for Occupational Safety and Health’s (NIOSH) Human Subjects Review Board and written informed consent was obtained prior to study participation. Subjects were instructed to abstain from alcohol, caffeine, and strenuous exercise for at least 24 hours prior to their test visit.
Testing Protocol
Each of the 6 participants was tested a total of 3 times, once for each ensemble (ensemble 1 [E1], ensemble 2 [E2], and ensemble 3 [E3]). Each test was completed within environmental conditions that represented conditions similar to those of Ebola-stricken countries in West Africa. The exercise protocol consisted of 60 minutes of continuous walking, within an environmental chamber, on a treadmill at an intensity of 3 METs (2.5 mph, 0% grade). This exercise intensity was chosen to represent the working intensity seen in hospital nurses during patient care, such as walking, standing, and carrying light objects.Reference Ainsworth, Haskell and Herrmann 9 Each testing protocol consisted of a 15-minute preexercise stabilization period (22°C, 50% relative humidity [RH]) and a 60-minute exercise period (32°C, 92% RH), followed by a 30-minute recovery period in ambient conditions (22°C, 50% RH). During the stabilization period, each subject was instructed to sit quietly in a chair as the chamber environmental conditions were stabilized. Individual testing days of the same subject were separated by a minimum 48-hour washout period to minimize confounding effects of heat acclimation, dehydration, or fatigue. If predetermined termination criteria were met (rectal temperature [Tre] ≥39°C, heart rate [HR] ≥95% of maximum heart rate [HRmax] for greater than 2 minutes, volitional fatigue [rating of perceived exertion ≥19], subject’s desire to stop)Reference Borg 10 the testing was stopped immediately.
Testing Garments
Three different PPE ensembles were tested on each subject: E1, E2, and E3. The testing order of the garments was counterbalanced to minimize possible effects on outcome variables.
E1 consisted of medical scrubs; socks and rubber boots; a mid-calf-length disposable, fluid-resistant surgical gown (High Performance Surgical Gown 7696C; 3M, St. Paul, MN); polyethylene surgical apron (A70; KleenGuard, Kimberly Clark); face shield (FisherBrand Anti-Fog 19-460-10; Fisher Scientific, Pittsburgh, PA); disposable nitrile examination inner gloves (Better Touch; CABVI, Utica, NY); heavy-duty nitrile outer gloves (Assurance model 50-N-242064; Protective Industrial Products, Inc, Latham, NY); duckbill N95 surgical filtering face piece respirator (Kimberly Clark model 46828); and fluid-resistant surgical cap (Kimberly Clark KCH69240) (weight: 3.8 kg) (Figure 1).

Figure 1 Subject Outfitted to Start a Test Wearing the E1 Personal Protective Equipment Ensemble.
E2 consisted of medical scrubs, socks and rubber boots, Microgard coverall (Microgard, Kingston Upon Hull, United Kingdom) and separate custom-made Tyvek hood with integrated splash-resistant surgical mask (DuPont, Wilmington, DE), rubber surgical apron (Europrotex, La Bernadière, France), splash-resistant goggles (Bollè Duo, Oyonnax, France), surgical nitrile inner gloves, heavy-duty nitrile outer gloves, duckbill N95 filtering face piece respirator (Kimberly Clark model 46828), and fluid-resistant surgical cap (Kimberly Clark KCH69240) (weight: 4.1 kg) (Figure 2).
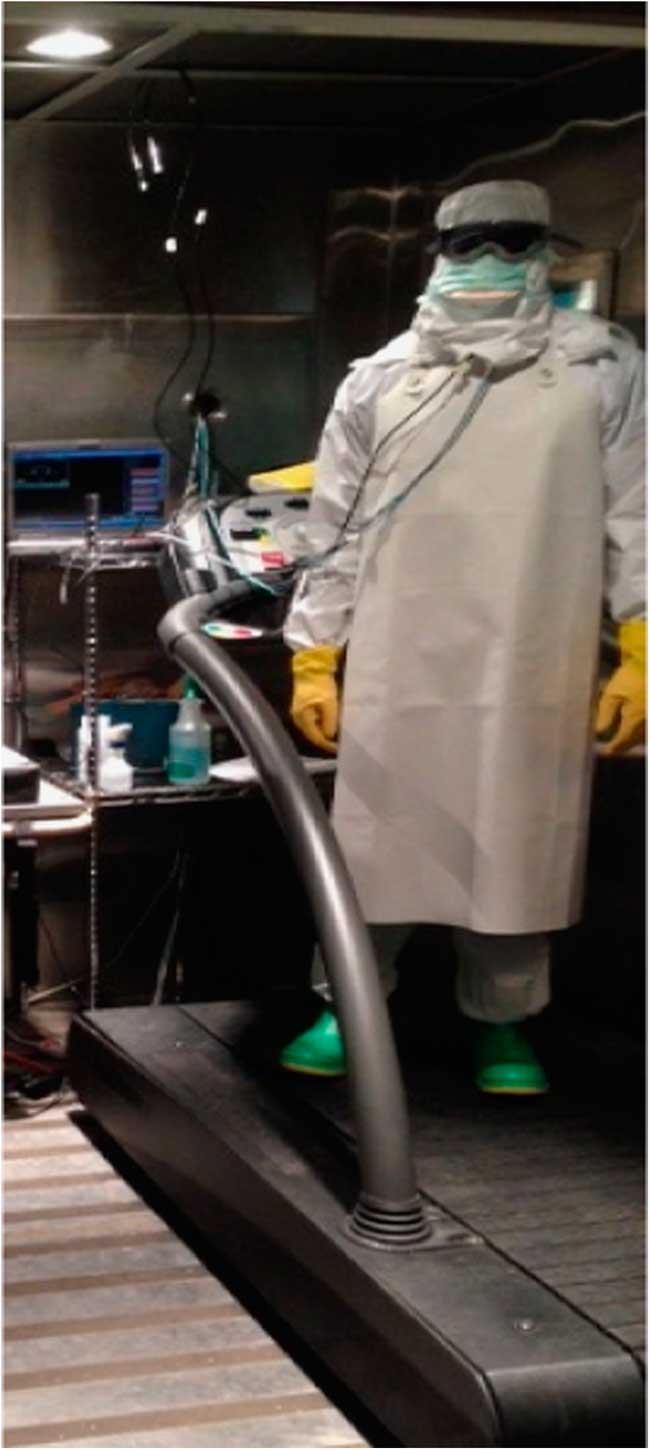
Figure 2 Subject Outfitted to Start a Test Wearing the E2 Personal Protective Equipment Ensemble.
E3 consisted of medical scrubs, socks and rubber boots, Tychem QC highly impermeable coverall (DuPont), Médecins Sans Frontières (MSF) custom-made Tyvek (DuPont) hood with integrated splash-resistant surgical mask, rubber surgical apron, splash-resistant goggles, surgical nitrile inner gloves, heavy-duty nitrile outer gloves, duckbill N95 filtering face piece respirator (Kimberly Clark model 46828), and fluid-resistant surgical cap (Kimberly Clark KCH69240) (weight: 4.2 kg) (Figure 3).
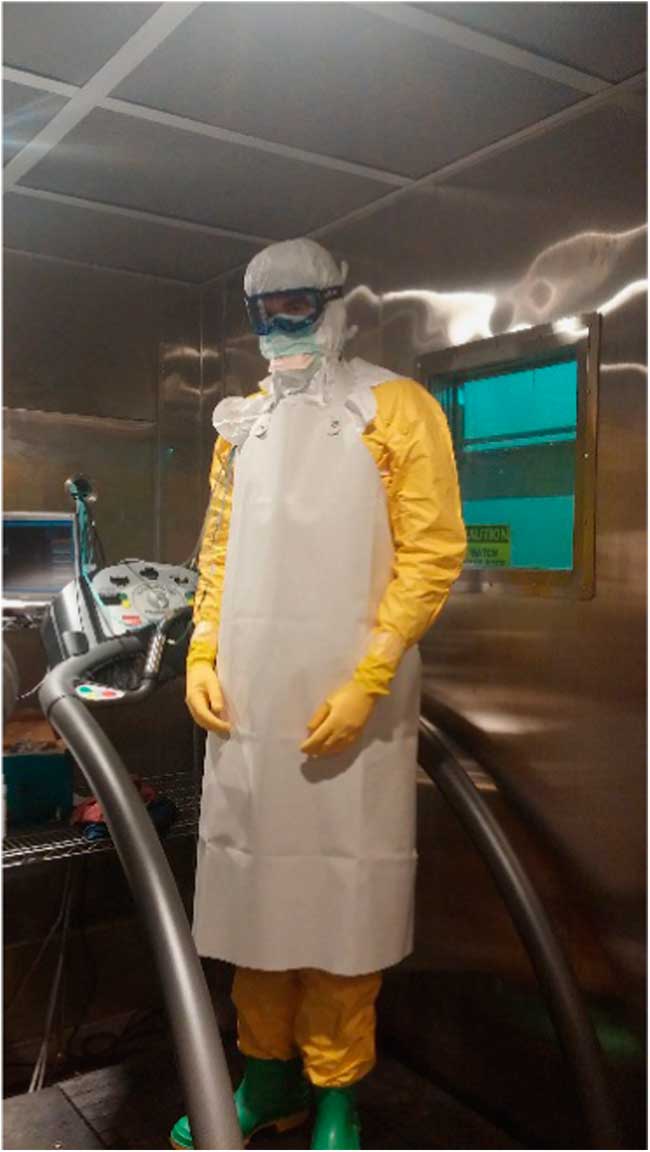
Figure 3 Subject Outfitted to Start a Test Wearing the E3 Personal Protective Equipment Ensemble.
Test Measurements
Semi-nude weight (kg) was measured both before and after exercise to evaluate sweating weight loss throughout testing. Tre was monitored continuously by using a rectal thermistor (model: REF-4491; YSI Temperature, Dayton, OH) inserted 13 cm beyond the anal sphincter. Skin temperature (Tsk) was measured by using 2.54-cm diameter T-type (copper/constantan) thermocouples (Concept Engineering, Old Saybrook, CT) that were placed on 4 body sites (upper chest, scapula, calf, and anterior thigh) with transparent dressing film (Tegaderm, 3M, St. Paul, MN). Average Tsk was calculated by using the standard International Standards Organization body site weighting formula below (Equation 1).Reference Ramanathan 11
HR was measured continuously by using the Zephyr BioHarness 3 (Zephyr Technology Corp, Annapolis, MD). Five subjective variables were taken every 15 minutes throughout exercise and recovery: heat sensation, thermal comfort, rating of perceived exertion (RPE), breathing comfort, and wetness. Subject measurement of heat sensation was measured on a scale of 4 to -4 (where 4=very hot, 0=neutral, and -4=very cold).Reference Coca, DiLeo and Kim 7 , 12 Subjective thermal comfort was measured on a scale of 1 to 4 (where 1=not uncomfortable and 4=very uncomfortable). 13 RPE was measured by using the OMNI 6-20 exertional scale.Reference Borg 10 Breathing comfort was measured by using a scale of 1 to 7 (where 1=no discomfort and 7=intolerable discomfort). Subjective wetness was measured by using a scale of 1 to 5 (where 1=dry and 5=soaked).
Statistical Analysis
Each measurement variable was calculated for mean and standard deviation for 3 time periods: start of exercise, end of exercise, and end of recovery. Two-way repeated-measures analysis of variance (ANOVA) was used to determine main effects of time on each ensemble. Time points of start of exercise, end of exercise, and end of recovery were considered for Tre, HR, and all subjective measurements except for wetness. Tsk and wetness were tested across start of exercise and end of exercise. Significant differences in mean weight loss across ensembles was tested by using a two-sided t-test. The least significant difference method was used to evaluate individual differences across ensembles in post-hoc pairwise comparisons. The alpha level was set at p<0.05 for all tests.
RESULTS
Average weight loss per hour (kg) was greatest for E3 (1.48±0.47 kg), followed by E2 (1.26±0.53 kg) and E1 (0.94±0.40 kg) (Figure 4). Weight loss for E1 was significantly lower than for E2 (P=0.032) and E3 (P=0.000). Average HR during the start and end of exercise was highest for E3 and in the order E3>E2>E1 (Table 1), and a significant main effect of ensemble and time on HR was found (P=0.001 and p=0.000, respectively). HR at the start of exercise was significantly higher for E3 than for E1 (P=0.010) and E2 (P=0.000) and at end of exercise was significantly higher for E2 than for E1 (P=0.006) and significantly lower for E1 than for E3 (P=0.000).

Figure 4 Average Sweat Loss With the 3 Personal Protective Equipment Ensembles. n=6. Pairwise significance (P<0.05): acompared to ensemble 1, bcompared to ensemble 2, ccompared to ensemble 3.
Table 1 Skin and Core Temperatures

a-cPairwise significance (P<0.05): acompared to ensemble 1; bcompared to ensemble 2; ccompared to ensemble 3.
A significant main effect of both ensemble and time on Tre was found (P=0.002 and P=0.000, respectively). The highest Tre was reached at the end of exercise for the ensembles in the following order: E3>E2>E1. Tre at the end of exercise was significantly lower with E1 than with E2 (P=0.001) and E3 (P=0.000). The highest average Tsk at the end of exercise was observed in the order E3>E2>E1, and a significant main effect of time on Tsk was seen (P=0.003), with no main effect of ensemble on Tsk noted (Table 1).
Subjectively, at the end of exercise, perceived heat sensation was lower with E1 in the order E1<E2, E3, and a significant main effect of time (P=0.000) but not of ensemble was shown for heat sensation. Significant main effects of both time (P=0.000) and ensemble (P=0.006) were also found on thermal comfort score. Perceived thermal comfort score at the end of exercise was highest for E2 and E3>E1 and significant main effects of both time (P=0.000) and ensemble (P=0.006) on thermal comfort score were found. Significant pairwise comparisons showed that E1 had a lower perceived thermal comfort score than did E2 (P=0.045) and E3 (P=0.017). End of exercise RPE was highest for E3 in the order E3>E2>E1 and was significantly lower for E1 than for E2 (P=0.049) and for E1 than for E3 (P=0.004). Significant main effects of time and ensemble on breathing comfort score were found (P=0.000 and 0.021, respectively). Pairwise comparisons of breathing comfort showed that, at the end of exercise, breathing comfort was significantly lower with E1 than with E2 and E3 (P=0.001 and 0.025, respectively). At the start and end of exercise, perceived wetness was the same across all 3 garments (Table 2).
Table 2 Subjective Measurement Variables (Average Score±SD)

a-cPairwise significance (P<0.05): acompared to ensemble 1; bcompared to ensemble 2; ccompared to ensemble 3.
DISCUSSION
We tested the thermal stress characteristics of 3 PPE ensembles in human participants. The PPE ensembles tested were commonly used in West Africa during the health care effort to fight the Ebola outbreak. The 3 ensembles displayed varying heat stress characteristics in the human subjects that were very similar to the heat stress shown for those same ensembles in previous studiesReference Coca, DiLeo and Kim 7 , Reference Potter, Gonzalez and Xu 8 using thermal manikins. Generally, E1 had lower thermal stress properties following the 60-minute exercise bout than did E2 or E3. However, all 3 ensembles displayed potential for thermal stress over the exercise bout. Data from this human subjects study indicated that the E3 and E2 PPE ensembles increase Tre close to a critical level of 39°C more rapidly than the E1 ensemble. These results support anecdotal reports that HCWs are unable to wear this type of PPE for longer than 40 minutes without a break or cooling period. Furthermore, the 38.9°C Tre at the end of 60 minutes for E3 in this study shows the development of heat stress that could be exacerbated when HCWs need to have several 1-hour shifts within a day. Even though a recent studyReference Morley, Beauchamp and Suyama 14 showed that changes in neurocognitive performance during or immediately after 50 minutes of exercise in the heat wearing PPE are not noted, and another studyReference Schlader, Temple and Hostler 15 showed that risk-taking behavior is not affected by mild heat stress, it has been demonstrated that reaching Tre of 39°C over 1 hour is associated with decrements in simple mental performance.Reference Hancock and Vasmatzidis 16 This is very important information for HCWs in West Africa to determine work-rest cycles. One key consideration is the need to provide quality supportive care to patients, which is impeded by short work periods unless additional staff is available. During the Ebola outbreak, it became clear that the quality of care is crucial for improving survival rates. HCWs should consider heat stress development when using these ensembles in West Africa for their safety and as well as to provide the best quality of care for patients.
Drawing from these conclusions, HCWs must be trained and educated in the proper use and potential risks of using PPE ensembles, such as the ones tested in the current study, in hot and humid environments. As seen in the weight-loss data, 60 minutes of low-intensity exercise could result in a person losing 0.94 to 1.48 kg of sweat (about 1.3% to 2.2% of body weight lost). Even though 2 recent field studiesReference Grélot, Koulibaly and Maugey 17 , Reference Maynard, Kao and Craig 18 reported slightly lower weight loss (average, 0.6 kg/h and 0.84 kg/h) than our data in HCWs caring for Ebola patients in Conakry, Guinea, and Kerry Town, Sierra Leone, the environmental conditions differed from our laboratory study. One of the studies found that the weight loss was dependent on the time of the day, being significantly higher from 11:00 AM to 14:59 PM than the rest of the day. Because of this, hydration strategies and hydration education must be emphasized to these HCWs to prevent dehydration-associated issues such as fatigue, dizziness, and decreased performance. Again, training on potential risks (dehydration, recognizing the signs of heat stress, limiting time using PPE in harsh conditions) could be key for HCW. Training raises awareness and reinforces good behaviors.
This physiological evaluation of PPE was supported by the subjective measurements as well. Participants showed an increased heat perception for E2 and E3 compared to E1, which could make HCWs not feel comfortable when working in conditions similar to the current study. They also reported higher perceived exertion with E2 and E3 than for E1, which demonstrates that wearing those ensembles could increase fatigue and heat stress as shown by the values for HR and Tre at the end of exercise. These increased heat perceptions, increased RPE, and increased breathing discomfort at the end of exercise are other reasons for heat stress training and PPE training. Such training would greatly improve the HCWs’ knowledge of potential risks, allowing them to counteract any adverse and potentially unsafe situations.
Finally, a recent studyReference Quinn, Kim and Strauch 19 reported a potential heat mitigation strategy using cooling vests under the PPE. Depending on the technology used in the cooling vests (from phase-change materials to liquid cooling devices), the time to reach a critical level of 39°C core temperature could be increased by 20 to 30 minutes (respectively) compared with not using cooling. It is clear that the use of any cooling strategy can be advantageous in decreasing the negative physiological and subjective responses to the heat stress encountered by HCWs while wearing PPE in hot and humid environments.
CONCLUSIONS
Because the PPE ensemble configurations studied are similar to the ensembles worn in West Africa for the Ebola outbreak, heat stress and PPE training is recommended for HCWs serving in those and similar conditions. The implementation of a work-rest ratio that avoids dehydration and possible heat stress issues is also recommended, as well as the implementation of possible cooling and heat mitigation strategies and other precautions that would alleviate the heat stress faced by HCWs. Such measures will help to achieve thermal relief during the recovery periods and allow for possibly longer, but safer, work periods.
Acknowledgments
The authors are sincerely grateful for the technical and experimental support in conducting the present study from NIOSH’s Emergency Preparedness and Response Office (Chad Dowell and Lisa Delaney), the CDC foundation, Susan Lovasic (DuPont), and the in-depth review and helpful comments from Rosa Costanza Vallenas (World Health Organization) and Ying Ling Lin (University of Toronto). Photos courtesy of NIOSH.
Disclaimer
The findings and conclusions in this report are those of the authors and do not necessarily represent the views of the National Institute for Occupational Safety and Health. Mention of company names or products does not constitute endorsement by NIOSH.








