Introduction
Current hypotheses of psychological mechanisms of psychosis have emphasized that the response to abnormal experiences is cognitively mediated by self-beliefs, maladaptive self-schema or appraisals (Garety, Kuipers, Fowler, Freeman and Bebbington, Reference Garety, Kuipers, Fowler, Freeman and Bebbington2001). Although the development of maladaptive schemas in people with psychosis has not been systematically examined, it has been well established in depression research through the work of Beck and other cognitive therapists that early development and, in particular, social adversities impact the development of maladaptive self-schemas and beliefs about the world, others and the self. In addition to the debate about the exact nature and significance of the schema construct, assessment of such schema is limited by existing measures (Fowler et al., Reference Fowler, Freeman, Smith, Kuipers, Bebbington, Bashforth, Coker, Hodgekins, Gracie, Dunn and Garety2006). Recently, Fowler and colleagues (Reference Fowler, Freeman, Smith, Kuipers, Bebbington, Bashforth, Coker, Hodgekins, Gracie, Dunn and Garety2006) developed The Brief Core Schema Scales (BCSS) to provide a theoretically coherent self-report assessment of schemata concerning self and others in psychosis.
The development of these scales has been well described elsewhere (Fowler et al., Reference Fowler, Freeman, Smith, Kuipers, Bebbington, Bashforth, Coker, Hodgekins, Gracie, Dunn and Garety2006). Briefly, the BCSS are quick and easy to administer. The scale assesses four dimensions of self and other evaluation: negative-self, positive-self, negative-other and positive-other. The BCSS have good psychometric properties and demonstrate more independence from mood than the Rosenberg self-esteem scale. Individuals with chronic psychosis reported extreme negative evaluations of self and others on these scales, but their levels of self-esteem and positive evaluation of self and others were similar to the normal control sample. Thus, the BCSS may provide a more useful measure of schemata about self and others than traditional measures of self-esteem.
An important focus currently in schizophrenia research is understanding the development of psychosis in individuals who are seen to be at clinical high risk for psychosis, i.e. putatively prodromal for psychosis. It has been demonstrated that a cognitive style characterized by worry, low self-esteem, neuroticism or depression may increase the risk for developing clinical psychosis (Krabbendam et al., Reference Krabbendam, Myin-Germeys, Hanssen, de Graff, Vollebergh, Bak and van Os2005). If maladaptive schemas and self-beliefs do play a role in the onset of psychosis these are potentially malleable factors for which we could have effective psychological interventions (Morrison et al., Reference Morrison, French, Walford, Lewis, Kilcommons, Green, Parker and Bentall2004). It would therefore be important to have a valid measure of schemata of self and others.
The purpose of this study was to administer the BCSS to a sample of individuals who are at clinical high risk for psychosis to determine if this may be a useful scale to identify targets for intervention in this population.
Method
Subjects
The sample consisted of 38 clinical high risk individuals (CHR) who are part of the PRIME clinic at the Centre for Addiction and Mental Health in Toronto. All CHR subjects met the Criteria of Prodromal States (COPS) using the Structured Interview for Prodromal Syndromes (SIPS; Miller et al., Reference Miller, McGlashan, Rosen, Cadenhead, Ventura, McFarlane, Perkins, Pearlson and Woods2003a). The COPS includes three criteria: attenuated positive symptom state (APS), brief intermittent positive symptoms (BIPS), and genetic risk and deterioration (GRD). All subjects in this study met APS criteria, which is based on duration and severity of prodromal symptoms and includes the emergence or worsening over the past year of a non-psychotic disturbance of thought content, thought process or perceptual abnormality. None of the CHR subjects met any DSM-IV criteria for any psychotic disorder.
The mean age of the subjects was 19.7 years (SD = 3.4); 74 % of the group was male (n = 28) and 26 % was female (n = 10). In terms of race 65.8% were Caucasian, 23.7% were Asian, 2.6% Black, and 7.9% were of mixed race.
Measures
The Brief Core Schema Scales (BCSS; Fowler et al., Reference Fowler, Freeman, Smith, Kuipers, Bebbington, Bashforth, Coker, Hodgekins, Gracie, Dunn and Garety2006) were used to assess self and other evaluation. The BCSS have 24 items concerning beliefs about the self and others that are assessed on a 5-point rating scale (0–4). Four scores, each with six items, are obtained: negative-self, positive-self, negative-others and positive-others.
The Young Schema Questionnaire–Short version (YSQ-S; Young, Reference Young1998; http://home.sprynet.com/sprynet/schema/ysqs1.htm) is a 5-item self-report inventory designed to assess 15 types of core schematic beliefs. As in the development of the BCSS (Fowler et al., Reference Fowler, Freeman, Smith, Kuipers, Bebbington, Bashforth, Coker, Hodgekins, Gracie, Dunn and Garety2006) we only administered the subscales that related to the BCSS – mistrust/abuse, social isolation, defectiveness/shame, failure, and self-sacrifice. Each is rated on a 6-point Likert Scale ranging from 1(strongly disagree) to 6 (strongly agree). Higher scores indicate a greater endorsement of a schema.
The Scale of Prodromal Symptoms (SOPS; Miller et al., Reference Miller, McGlashan, Rosen, Cadenhead, Ventura, McFarlane, Perkins, Pearlson and Woods2003a) was used to assess prodromal symptoms. Depression was measured with the Calgary Depression Scale for Schizophrenia (CDSS; Addington, Addington, Maticka-Tyndale and Joyce, Reference Addington, Addington, Maticka-Tyndale and Joyce1992). One of the unique features of the CDSS is that it differentiates between depressive and negative symptoms. Although these subjects do not have schizophrenia, they do present with negative symptoms (Miller et al., Reference Miller, Zipursky, Perkins, Addington, Woods, Hawkins, Hoffman, Preda, Epstein, Addington, Lindborg, Marquez, Tohen, Breier and McGlashan2003b).
Results
Reliability analysis was conducted by first assessing alpha co-efficients and item whole correlations. The alpha coefficients for the positive- and negative-self schema scales were 0.85 and 0.88 and for the positive- and negative-other schema scales were 0.94 and 0.92. All item total correlations were highly significant (p < .001). The median item total correlation was 0.75.
To check concurrent and discriminant validity, Spearman's correlations between the BCSS subscales and the YSQ subscales and CDSS were conducted. High ratings on the BCSS positive-self subscale and the BCSS positive-other scales were significantly associated with a lack of social isolation and failure and a low sense of defectiveness and shame on the YSQ. High ratings on the BCSS negative-self subscale and negative-other subscale were significantly associated with high levels of mistrust, social isolation, defectiveness, and failure on the YSQ and not with self-sacrifice. Only the BCSS negative-self subscale was significantly associated with depression as rated by the CDSS. Since there are concerns with multiple correlations we have indicated in Table 1 which of the correlations would no longer be significant if we used a Bonferroni correction. Even with applying a strict correction (which was not used in the original development of the scales paper) the results still support the validity of the scales.
Table 1. Spearman's bivariate correlations between Brief Core Schema subscales and the Young's Schema Questionnaire (YSQ) subscales and the Calgary Depression Scale for Schizophrenia (CDSS)
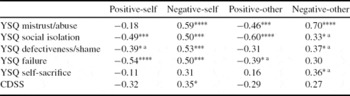
****p < .0001, ***p < .001, **p < .01, *p < .05
a no longer significant if Bonferroni correction is applied
An examination of the associations between the BCSS and SOPS positive symptoms (unusual thought content, suspiciousness, grandiosity, perceptual abnormalities and disorganized communication) revealed that unusual thought content was associated with negative-self (r = 0.41, p < .05) and negative-other (r = 0.44, p < .01); suspiciousness was significantly associated with negative-self (r = 0.39, p < .05) and negative other (r = 0.67, p < .01). The total positive symptom score was associated with negative-self (r = 0.47, p < .01) and negative-other (r = 0.68, p < .01). Low ratings on disorganized communication were related to positive-other (r = −0.33, p < .05) and perceptual abnormalities were related to negative-other (r = 0.46, p < .01).
Based on these significant associations we conducted standard regression analyses, first with unusual thought content, then suspiciousness, and thirdly with total SOPS positive symptoms as the dependent variables and depression, negative-self and negative-other as the explanatory variables. For unusual thought content, the model was significant but only 10% (adjusted r2) of the variance was explained by the model and none of the variables made a significant unique contribution. For suspiciousness, the model was significant, 35% (adjusted r2) of the variance was explained by the model. Negative-other made a significant unique contribution (Beta = 0.63, p = .002). For total positive symptoms, the model was significant, 41% (adjusted r2) of the variance was explained by the model. Negative-other made a significant unique contribution (Beta = 0.63, p = .001).
Discussion
The BCSS has been demonstrated to be a valid, yet quick and easy measure to use. In this sample with individuals who are at clinical high risk of developing psychosis, we have demonstrated that the BCSS have internal consistency, and similar concurrent and discriminant validity as in the original development study. Positive symptoms in general and suspiciousness in particular were uniquely predicted by negative-other evaluations although negative-self contributed to the model. These findings are similar to those reported by Fowler et al. (Reference Fowler, Freeman, Smith, Kuipers, Bebbington, Bashforth, Coker, Hodgekins, Gracie, Dunn and Garety2006). There were no associations in this sample between grandiosity and positive-self, but in this population grandiosity tends to be the least endorsed positive symptom (Miller et al., Reference Miller, Zipursky, Perkins, Addington, Woods, Hawkins, Hoffman, Preda, Epstein, Addington, Lindborg, Marquez, Tohen, Breier and McGlashan2003b). A major limitation of this study is the small sample size. However, subjects at risk of developing psychosis are hard to find and most single site studies usually report between 18 and 25 per annum (Addington et al., Reference Addington, Cadenhead, Cannon, Cornblatt, McGlashan, Perkins, Seidman, Tsuang, Walker, Woods and Heinssen2007, Reference Addington, Epstein, Reynolds, Furimsky, Rudy, Mancini, McMillan, Kirsopp and Zipursky2008).
In summary, the BCSS appear to be valid scales to use with this population. They may be particularly useful as research focuses more on the development of psychotic symptoms and an understanding of individuals' self and other evaluations may contribute valuable information. Furthermore, since psychological interventions may be more appropriate in this prepsychotic period, these scales can help identify targets for intervention.
Acknowledgements
This work was supported by NIMH grant U01MH066134 and a grant from Ontario Mental Health to Jean Addington.




Comments
No Comments have been published for this article.