Background
Myocarditis is an important cause of morbidity and mortality in children and young adults, and patients surviving the acute phase may develop chronic heart failure and dilated cardiomyopathy.Reference Drory, Turetz and Hiss 1 , Reference Ghelani, Spaeder, Pastor, Spurney and Klugman 2 The gold standard for definitive diagnosis has traditionally been endomyocardial biopsy and the Dallas criteria;Reference Aretz 3 , Reference Mason and O’Connell 4 however, because of the invasive nature of the biopsy and the risks associated with it, the diagnosis of myocarditis remains mainly clinical, with the use of symptoms, electrocardiographic changes, biomarkers, viral serology, or polymerase chain reaction for diagnosis.Reference Canter and Simpson 5 Utilisation of biopsies for diagnosis varies among centres and may be appropriately restricted to patients with atypical clinical presentations, ambiguity in diagnosis, and to patients in whom an important alternative diagnosis is plausible, such as giant-cell myocarditis or pseudo-infarction.
Cardiac MRI was first described as a diagnostic tool for children with acute myocarditis in 1991,Reference Gagliardi, Bevilacqua, Di Renzi, Picardo, Passariello and Marcelletti 6 and continues to evolve in that respect.Reference Friedrich, Sechtem and Schulz-Menger 7 , Reference Levine, Klugman and Teach 8 It is an inherently attractive replacement for biopsy for the diagnosis of myocarditis, and multiple studies have attempted to validate cardiac MRI for the diagnosis of myocarditis.Reference Friedrich, Sechtem and Schulz-Menger 7 , Reference Levine, Klugman and Teach 8 However, there are very limited data in the paediatric literature about the role and utility of cardiac MRI in myocarditis.Reference Canter and Simpson 5 A recent paediatric study demonstrated late gadolinium enhancement during cardiac MRI to be a predictor of poor outcome,Reference Sachdeva, Song, Dham, Heath and DeBiasi 9 and a recent study in adults showed that patients who had a normal cardiac MRI in the setting of clinical evidence for myocarditis had a good prognosis, independent of their clinical presentation.Reference Schumm, Greulich and Wagner 10 Prognostic evidence is conflicting, however, as another adult study showed that the presence and extent of myocardial oedema or fibrosis on cardiac MRI did not predict an adverse clinical outcome.Reference Sanguineti, Garot and Mana 11 Similarly, a more recent multi-centre paediatric study described various techniques for assessing the myocardium in patients with myocarditis, such as gadolinium enhancement (early or late), but was unable to find any correlation with left-ventricular dysfunction.Reference Banka, Robinson and Uppu 12 The goal of our descriptive, retrospective study was to assess the utility of cardiac MRI, characteristics of patients who underwent cardiac MRI, and the predictive ability of cardiac MRI findings. In addition, our hypothesis was that cardiac MRI is a poor predictor of clinical outcomes.
Methods
Patient selection
Patients with a clinical diagnosis of myocarditis at a tertiary care paediatric hospital between August, 2008 and July, 2015 were identified by the International Classification of Diseases, ninth revision codes, for discharge diagnosis. The attending cardiologist clinically diagnosed myocarditis on the basis of clinical signs and symptoms and on evidence of acute cardiac dysfunction along with a history of a viral prodrome. Findings supporting a diagnosis of myocarditis included tachycardia, ventricular ectopy, electrocardiographic changes, and changes in levels of biomarkers such as C-reactive protein or brain-type natriuretic peptide. A sub-cohort of patients who had undergone cardiac MRI at the time of clinical presentation was identified. The decision to perform cardiac MRI was dependent on the attending physician. Cardiac MRI was used most commonly when there was a question regarding the aetiology of a patient’s presentation. Medical records were examined to obtain demographic data, and clinical data at baseline, discharge, and at 1-year follow-up.
Cardiac MRI technique
Cardiac MRI studies with vectorcardiogram triggering were performed using 1.5 T systems (Signa TwinSpeed; General Electric Medical Systems, Milwaukee, Wisconsin, United States of America until October, 2010 and from MAGNETOM Aera; Siemens Healthcare, Erlangen, Germany, from October, 2010 to the present). In older patients, breath-holding was used, and in younger children either free-breathing with multiple signal averages or respiratory navigation was used. Parallel imaging was used with an integrated Parallel Acquisition Technique, Generalized autocalibrating partially parallel acquisitions (iPAT GRAPPA) factor of 2 for all imaging sequences, and the field of view was adjusted to avoid phase wrap on a patient-specific basis but was generally 280–400 mm with phase field of view of 70–100%. Functional imaging was performed in the two-chamber, four-chamber, and short-axis geometries using cine steady-state free precession contiguous 6–10 mm slices with no slice gap and with an inplane resolution of ~1.4 mm2. T1- and T2-weighted turbo-spin echo pre-contrast imaging was performed with 8 mm slices and a gap of 2 mm in the short-axis geometry, with an inplane resolution of 1.3 mm. For T1-weighted images, time to echo was 20 ms, flip angle was 180°, and trigger pulse was 1. For T2-weighted images, time to echo was 90 ms, flip angle was 180°, and trigger pulse was 2. Early post-gadolinium T1 turbo-spin echo imaging was performed in the short-axis geometry 3–5 minutes after the administration of 0.1 mmol of gadopentetate dimeglumine or gadobenate dimeglumine using parameters identical to those of the pre-contrast T1 turbo-spin echo images. Late post-gadolinium enhancement imaging was performed 10–20 minutes after the administration of contrast using either a single-shot or a phase-sensitive inversion-recovery technique. Regardless of the late post-gadolinium enhancement sequence used, images were obtained in the short-axis and four-chamber geometries with the inversion time set using a look-locker sequence, with 8 mm slices and a 2 mm slice gap. Cardiac MRI studies were reviewed for evidence of myocarditis. Cardiac MRI results were considered consistent with myocarditis if the Lake Louise Consensus CriteriaReference Friedrich, Sechtem and Schulz-Menger 7 were met. Cardiac MRI results were considered equivocal if there was evidence of oedema, hyperaemia, or fibrosis on cardiac MRI, and the Lake Louise Consensus Criteria were not met.
Statistical methods
Statistical analyses were performed using SAS® version 9.4 (SAS Institute, Cary, North Carolina, United States of America). Statistical significance was assessed at the 0.05 level unless otherwise noted. Descriptive statistics were calculated for all variables of interest and included medians and interquartile ranges, and counts and percentages, as appropriate. Normality of continuous variables was assessed using histograms, normal probability plots, and the Anderson–Darling test for normality. Tertiles of continuous measures were also fit to determine whether the association between predictors and outcomes was non-linear. Characteristics of patients who had undergone cardiac MRI and those who had not were compared using the χ2 test for categorical variables or the Wilcoxon rank-sum test for continuous variables. When expected cell counts were small (<5), the Fisher exact test was used in place of the χ2 test. Odds ratios and 95% confidence intervals were used to compare risks of predictors for each different outcome (cardiac death/transplant, discharge on heart failure medications, and use of heart failure medications at 1 year) using logistic regression models. Odds ratios and 95% confidence intervals were computed for tertiles of echocardiographic left-ventricular ejection fraction using the highest level as the reference group (⩾55.57%). Similarly, odds ratios and 95% confidence intervals were computed for tertiles of peak C-reactive protein levels using the lowest level as the reference group (⩽2.2 mg/dl).
Results
Utilisation of cardiac MRI
A total of 44 patients with a clinical diagnosis of myocarditis were identified. A sub-cohort of 20 patients had undergone cardiac MRI as a part of their diagnostic workup. All patients had undergone multiple echocardiographies including during the follow-up period, but none of the patients had undergone follow-up cardiac MRI. The clinical characteristics of both patient cohorts are listed in Table 1.
Table 1 Demographics of patients who underwent cardiac MRI and those who did not.

ECMO=extracorporeal membrane oxygenator; IVIG=intravenous immunoglobulin; VAD=ventricular-assist device
Values presented as median (25th–75th) or n (%)
Bold values represent statistically significant p values <0.05
Patients who had undergone cardiac MRI were older compared with the rest of the cohort, with a median age of 15.6 versus 11.1 years (p=0.003). Patients who had undergone cardiac MRI had overall less-severe illness as evidenced by overall shorter length of hospital stay (4.0 versus 12.5 days, p=0.004), higher left-ventricular ejection fraction on initial echocardiography (56.8 versus 28.6%, p<0.001), and lower peak brain-type natriuretic peptide levels (136 versus 2690 pg/ml, p<0.001), compared with the rest of the cohort. There were no significant differences in peak troponin levels or peak C-reactive protein levels between the two groups, although patients undergoing cardiac MRI tended to have higher peak troponin levels (median 13.9 versus 3.8 ng/ml, p=0.09). Patients who underwent cardiac MRI were less likely to require advanced support with inotropes, extracorporeal membrane oxygenation, antiarrhythmic medications, or a ventilator, compared with those who did not undergo cardiac MRI. There were no patients who required ventricular assist devices. Patients who underwent cardiac MRI were no more likely to receive therapy with intravenous immunoglobulins, steroids, antivirals, or other immunosuppressant medications than the rest of the cohort. Of all aforementioned therapies, only the use of steroids showed a trend towards significance with a p value of 0.05, with less use in patients undergoing cardiac MRI compared with those who did not undergo a cardiac MRI.
Patients who had undergone cardiac MRI were less likely to have an outcome of cardiac death at the time of discharge from the hospital (0 versus 25%, p=0.025) compared with those who had not undergone cardiac MRI. There were no significant differences in the proportion of patients discharged on heart failure medications or requiring readmission within 1 year of discharge between the two groups.
Cardiac MRI findings
Cardiac MRI findings are summarised in Table 2 and the percentage of patients with individual cardiac MRI findings are illustrated in Figure 1. Representative images from a child with cardiac MRI-confirmed myocarditis are shown in Figure 2. The median time from admission to cardiac MRI was 2 (1–3) days. The median left-ventricular ejection fraction was 57.1% (53.5–63.5%). Less than half of the patients who underwent cardiac MRI had significant left-ventricular dysfunction. Studies conducted before the publication of the Lake Louise Consensus CriteriaReference Friedrich, Sechtem and Schulz-Menger 7 did not uniformly have T2 pre-contrast, T1 early post-contrast, and late gadolinium enhancement sequences performed, but did include most or all of these sequences. In all, five patients (41.7%) had findings of oedema (areas of high T2 signal intensity), nine (50.0%) patients had findings of hyperaemia (areas of increased early gadolinium enhancement), and nine (47.4%) patients had findings of irreversible cell injury or fibrosis (areas of late gadolinium enhancement). Although all patients in his cohort had a clinical diagnosis of myocarditis, only seven (35.0%) had cardiac MRI findings consistent with myocarditis according to the Lake Louise Consensus Criteria. An additional six patients (30.0%) had cardiac MRI findings characterised as equivocal, having only one of the characteristic cardiac MRI findings. The remaining seven patients (35.0%) did not exhibit any of the three characteristic findings for myocarditis, but were still thought to have myocarditis on the clinical evaluation and thus were included in this analysis. It is noteworthy that only 10 patients (22.7%) from the larger cohort of 44 underwent an endomyocardial biopsy for diagnostic confirmation. Of these patients, five demonstrated biopsies consistent with the diagnosis of acute myocarditis based on the Dallas criteria.

Figure 1 Cardiac MRI findings. GE=gadolinium enhancement.
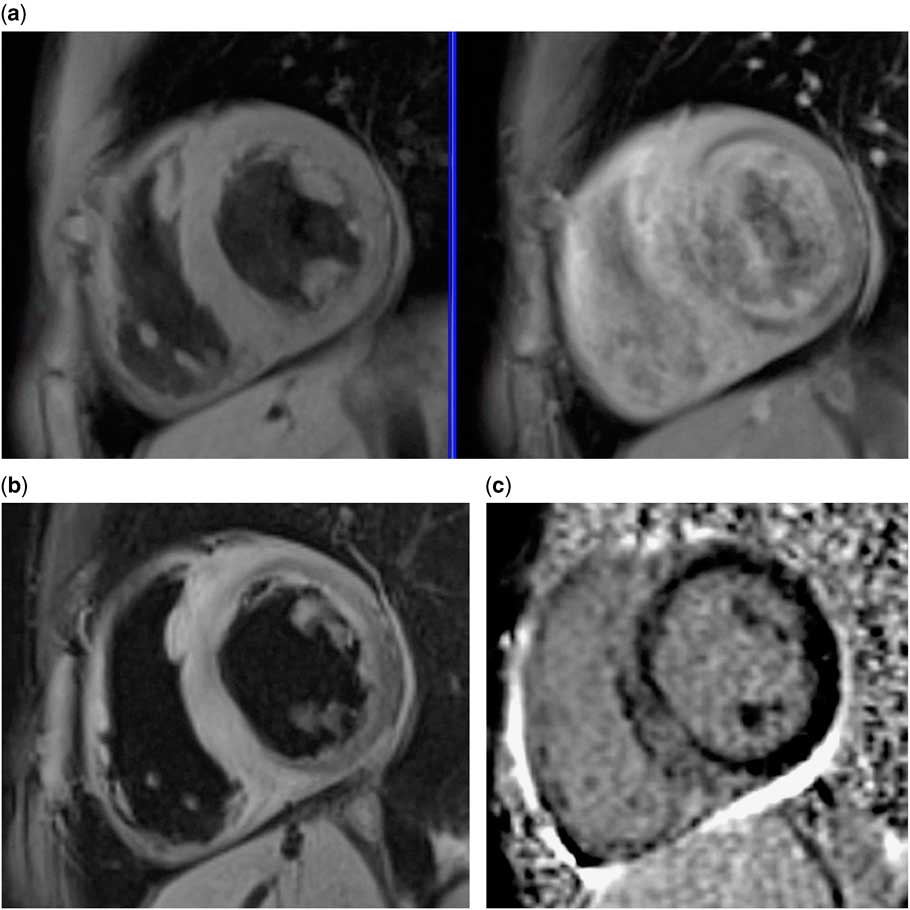
Figure 2 Representative images from a child with cardiac MRI-confirmed myocarditis. ( a ) T1 pre- and post-contrast imaging, with early gadolinium enhancement demonstrating myocardial hyperaemia. ( b ) T2 pre-contrast imaging demonstrating myocardial oedema. ( c ) Late gadolinium enhancement demonstrating myocardial fibrosis.
Table 2 Cardiac MRI results (n=20).

Values presented as median (25th–75th) or n (%)
Predictors of outcomes
The outcomes of interest were death, discharge with heart failure medications, and alive with heart failure medications at 1 year. The predictors of each outcome determined using logistic regression analysis are shown in Table 3. Cardiac MRI findings consistent with the Lake Louise Consensus Criteria did not predict worse outcomes. In fact, a predictor for discharge on heart-failure medication after initial hospitalisation was the absence of oedema as confirmed by cardiac MRI (odds ratio=24.0, 95% confidence interval 1.1–505.2, p=0.041). Presence of ventricular dysfunction on echocardiography (ejection fraction), high level of C-reactive protein on admission, and need for mechanical ventilation were all associated with cardiac death at primary hospitalisation. The odds of cardiac death (patient death or heart transplant) before discharge was 16.1 times higher for patients who required a ventilator compared with those who did not require a ventilator (odds ratio= 16.1, 95% confidence interval: [1.7–156.5], p=0.017). The odds of being discharged home on heart-failure medication was 4.1 times higher for patients who required antiarrhythmics compared with the odds for those who did not (odds ratio=4.1, 95% confidence interval 1.1–14.9, p=0.033). Presence of left-ventricular dysfunction on echocardiography was associated with an increased risk for cardiac death, such that a 10% decrease in ejection fraction on admission was associated with odds of 2.2 (95% confidence interval: 1.1–4.7).
Table 3 Predictors of each outcome (odds ratio (OR) 95% confidence intervals (CI)).

ECG=electrocardiogram; ECMO=extracorporeal membrane oxygenator; GE=gadolinium enhancement; IVIG=intravenous immunoglobulin; LV=left ventricle; Ref.=referent values; RV=right ventricle; VAD=ventricular-assist device
Bold values represent statistically significant p values <0.05
* OR based on 10 unit decrease
** OR based on 5 unit increase
*** Unable to estimate 95% confidence interval
Patients with the lowest left-ventricular ejection fraction on echocardiography at admission demonstrated a trend towards increased risk for cardiac death and the need for heart-failure medications at 1 year, but these were not statistically significant (p=0.133). Patients who received intravenous immunoglobulin did not have significantly different outcomes from those who did not receive intravenous immunoglobulin.
Finally, a composite model was developed using the initial risk factors obtained using univariate analysis from Table 3. A final model (Table 4) consisting of four specific risk factors – decreased left-ventricular function on echocardiography, ventilator requirement, inotrope requirement, and high C-reactive protein – is suggested. Using this model, patients were predicted to have an increased risk for cardiac death when all four risk factors were present compared with having <4 risk factors (odds ratio=6.6, 95% confidence interval: [1.03–42.2], p=0.046).
Table 4 Risk factors for cardiac death (death or heart transplant).

CI=confidence interval
Bold values represent statistically significant p values <0.05
* Odds ratio (OR) for having 4/4 risk factors versus having <4 risk factors (may have 3, 2, 1 or none)
** OR for having 3/4 risk factors versus having <3 risk factors (may have 2, 1, or none)
Discussion
In this retrospective series of 44 patients with clinical myocarditis, cardiac MRI was utilised in 45% (20/44) of cases. Although low, this rate of utilisation is higher than previously reported rates of 5–28%.Reference Ghelani, Spaeder, Pastor, Spurney and Klugman 2 Initial utilisation analysis demonstrated that the patients who had undergone cardiac MRI had significantly less-severe illness at presentation as evidenced by length of hospital stay, higher left-ventricular ejection fraction on echocardiography, lower levels of peak brain-type natriuretic peptide, and lower requirement of support with inotropes, antiarrhythmics, and ventilators. Patients with higher acuity of illness were often precluded from travelling outside the cardiac intensive care unit to undergo cardiac MRI during the acute phase of illness. Therefore, the primary physician caring for the patient would make a clinical decision to forego cardiac MRI in patients in whom the clinical diagnosis is highly likely and/or patient acuity does not allow travel outside the ICU for an hour-long study. This selection bias is, however, well acknowledged in other studies, including the multi-centre Pediatric Health Information System-based study of administrative reporting and billing, which demonstrated significantly lower mortality and need for transplantation in patients undergoing cardiac MRI, leading the authors to hypothesise that the population represented a less-sick cohort of myocarditis patients. In addition, there is wide variation in the rate of utilisation of cardiac MRI from region to region. This selection bias therefore limits the analysis of cardiac MRI-based predictors of outcomes.
In this study, cardiac MRI findings consistent with the Lake Louise Consensus Criteria for acute myocarditis were not predictive of worse outcomes, although only seven patients met all criteria. These findings are in agreement with a recent study in adults by Sanguineti et al,Reference Sanguineti, Garot and Mana 11 which showed that the presence and extent of myocardial oedema or fibrosis on cardiac MRI did not predict an adverse clinical outcome. In addition, the outcomes of studies that actually utilised the Lake Louise Consensus Criteria are inconsistent, especially retrospective studies. Our study data are therefore comparable to the larger multi-centre study in which only 39/141 MRI studies included all of the components, and of them only 29 MRI studies met the Lake Louise Consensus Criteria for diagnosis.Reference Banka, Robinson and Uppu 12
Cardiac MRI provides far more data than echocardiography alone, and has successfully detected oedema and hyperaemia in many patients who did not reveal dysfunction on either echocardiography or cardiac MRI. The sensitivity of cardiac MRI allows for the detection of subtle changes in the myocardium in the absence of dysfunction. The clinical relevance of these findings, especially when patients show almost complete clinical recovery, is not clear because of significant variations in the patient population across studies, variations in inclusion criteria including biases, and variations in techniques. The relative value of added information from cardiac MRI beyond that obtained from clinical diagnosis and echocardiograms, which are standard practices, needs to be established with appropriately designed studies. Although cardiac MRI is very sensitive, findings from it are likely not specific enough to predict outcomes, and data continue to be very equivocal. In a retrospective study of 58 children with myocarditis, of whom 34 underwent cardiac MRI, Sachdeva et al demonstrated late gadolinium enhancement in 50% of patients (17/34). Although patients who did not undergo cardiac MRI had much worse outcomes, with 10 of 16 demonstrating poor outcomes, those who underwent cardiac MRI showed the presence of late gadolinium enhancement along with a severely depressed left-ventricular ejection fraction and peak brain-type natriuretic peptide >10,000 ng/L, which were risk factors for poor outcomes.Reference Sachdeva, Song, Dham, Heath and DeBiasi 9 Similarly, studies in adults have also shown late gadolinium enhancement as a predictor of chronic left ventricle dysfunction and dilations as well as of all-cause mortality in patients with biopsy-proven viral myocarditis.Reference Mahrholdt, Wagner and Deluigi 13 , Reference Grun, Schumm and Greulich 14 Although 50% of the cardiac MRI patients in our study had findings of hyperaemia (areas of increased early gadolinium enhancement), and nine (47.4%) patients showed late gadolinium enhancement, these findings were not predictive of worse outcomes. This is again in line with the study by Banka et al,Reference Banka, Robinson and Uppu 12 in which abnormalities on early gadolinium enhancement, late gadolinium enhancement, T2-weighted imaging as well as first-pass perfusion were not associated with left-ventricular dysfunction at follow-up. With continued advances in technology, newer imaging techniques are being tested to assess the superiority of certain sequencing methods over others in order to improve the diagnostic yield of cardiac MRI. For example, native T1 mapping is a quantitative technique that has been suggested as a useful tool for imaging myocardial oedema – either related to infarction or inflammation. In a recent study, Ferreira et alReference Ferreira, Piechnik and Dall’Armellina 15 demonstrated that quantitative T1 mapping had a superior diagnostic yield for adult myocarditis versus healthy controls, compared with other standard MRI sequences such as gadolinium enhancement or T2-weighted imaging. On the other hand, a study of adult myocarditis patients by Bohnen et al showed a contradictory result. They found that clinical features, standard MRI including the Lake Louise Consensus Criteria, T1 mapping, or extracellular volume fraction were not able to differentiate between patients with or without myocarditis. They, however, found that the global myocardial T2 was the only predictor of myocarditis. They provide a global myocardial T2 threshold of >60 ms as being highly sensitive for myocarditis but with marginal specificity.Reference Bohnen, Radunski and Lund 16 The prognostic utility of global T2 time was recently assessed in adults with myocarditis who met a combined endpoint of major adverse cardiovascular events after initial diagnosis of myocarditis. In this study, elevation and persistence of T2 time during acute illness predicted the occurrence of the combined endpoint. It is also noteworthy that a simple MRI-based ejection fraction of <30% at presentation was a stronger predictor of the combined endpoint in the same study with an odds ratio of 6.8 (range 1.56–24.12).Reference Spieker, Haberkorn and Gastl 17 Studies such as these need further validation to assess the true utility of these varied sequencing techniques in specific patient populations including children, as thus far the results have been inconsistent.
It is therefore not surprising that our current study has produced some results that are consistent with previous studies and others that are in conflict. The characteristics of the patients in our study who underwent cardiac MRI, having overall less-severe illness at presentation, likely account for the differences in the findings. A second possible explanation is the timing of carrying out cardiac MRI. Patients underwent cardiac MRI in our study relatively early, on average at 2 days from admission. In the aforementioned studies, the cardiac MRI timing was variable and often late. In the paediatric study by Sachdeva et al,Reference Sachdeva, Song, Dham, Heath and DeBiasi 9 the average time to cardiac MRI was <2 weeks and up to 3 weeks after the onset of symptoms, whereas in a similar adult study by Grun et alReference Grun, Schumm and Greulich 14 the average time was 4 weeks after the onset of symptoms. It is plausible that the sensitivity and specificity of cardiac MRI changes as the pathology evolves in acute myocarditis. This is suggested by and is similar to the study on suspected myocarditis by Sanguineti et al, which showed that when cardiac MRI was performed early – that is, at 3±2 days after presentation – the only parameter predictive of a poor outcome was a decreased left-ventricular ejection fraction at presentation, whereas gadolinium enhancement was not related to the outcome. Finally, because of the wide variation in clinical presentation and pathology, utilisation of a combined score may be a valuable matrix for outcome prediction. Various studies have identified individual risk factors such as hypotension, tachycardia, and elevated enzyme levels, along with decreased functioning and need for mechanical support as risk factors or poor outcomes. Our composite scoring model using four specific risk factors – decreased left-ventricular function on echocardiography, ventilator requirement, inotrope requirement, and high levels of C-reactive protein – demonstrated a six-fold increase in the risk for cardiac death. This may be a valuable, early tool for patient risk stratification and needs further validation. We suggest using a tool such as the one described by us that uses clinical data and echocardiographic data as points of comparison when designing cardiac MRI studies for myocarditis if the superiority of this modality is to be established.
Limitations
There continues to be wide variation in clinical practices in the management of paediatric myocarditis. Lack of guidelines or clinical protocols as well as inadequate supportive evidence has led to variation in the utilisation of modalities such as cardiac MRI in this patient group. This is a major limitation of the study, which has also been acknowledged in larger registry studies as well as in other single-centre studies. The small number of patients as well as the retrospective nature of the study inherently limits the strength of the findings, although the granularity of the data is an important strength. We, however, think that the study continues to add cumulative evidence to research on risk factors for outcomes and describes the evolving role of cardiac MRI in this population.
Conclusions
The diagnosis of myocarditis continues to be made primarily on clinical findings, but the use of cardiac MRI is increasing. Predictors of poor outcomes in paediatric myocarditis include low left-ventricular ejection fraction and high acuity at presentation. There appears to be a selection bias in the utilisation of cardiac MRI with lower acuity patients undergoing cardiac MRI and higher acuity patients not undergoing it. Although cardiac MRI is a sensitive tool, the relationships between various abnormalities detected using MRI and outcomes, such as long-term ventricular dysfunction, continue to be weak. Further research is needed to examine the utility of cardiac MRI findings above and beyond clinical and echocardiographic data in paediatric myocarditis patients.
Acknowledgements
The authors acknowledge the Emory+Children’s Pediatric Biostatistics Core for their help with analysis of the data.
Financial Support
This research received no specific grant from any funding agency, commercial or not-for-profit sectors.
Conflicts of Interest
None.









