Pulmonary atelectasis is common after surgical procedures and may result in impaired gas exchange. It is frequently observed in post-operative patients with excessive and viscous pulmonary secretions. In congenital heart surgery, inflammatory response involving the airways after cardiopulmonary bypass causes respiratory dysfunction owing to post-operative tissue oedema and excessive mucus secretion. Atelectasis is more frequently observed in patients who are given limited amounts of liquids or diuretic therapy following a cardiac surgery, which in turn prolongs duration of intensive care unit stay and mechanical ventilation.Reference Riethmueller, Kumpf and Borth-Bruhns 1 – Reference Peroni and Boner 3 These further contribute to recurrent respiratory infection and decreased lung function. Although respiratory physiotherapy, inhaled bronchodilators, and mucus softening treatments are preferred traditionally in post-operative atelectasis, these treatment methods are not always effective.
Mucolytic therapy is one of the major components of the management of bronchopulmonary disease, pulmonary complications of cystic fibrosis, atelectasis, or pulmonary complications related to surgery. This helps to decrease viscosity of secretions, promoting secretion removal through coughing, postural drainage, and mechanical means. Recombinant human DNase is an enzyme that cleaves the deoxyribonucleic acid that builds the structure causing mucus to be viscous and cohesive.Reference Riethmueller, Borth-Bruhns and Kumpf 2 , Reference Boeuf, Prouix, Morneau, Marton and Lacroix 4 Similar to this agent, dornase alpha cause mucolysis, and it has been shown to be effective in other problems of the respiratory system such as cystic fibrosis.Reference Quan, Tiddens and Sy 5 Specifically, it has been reported that rescue treatments using dornase alpha have been effective in restoring airway continuity in children with post-operative atelectasis.Reference Riethmueller, Kumpf and Borth-Bruhns 1 , Reference Riethmueller, Borth-Bruhns and Kumpf 2 However, there are only limited data on the adjunctive therapy of atelectasis with dornase alpha in children after congenital heart surgery.
The purpose of this study was to investigate the efficacy of dornase alpha on pulmonary functions of children who developed post-operative pulmonary atelectasis following congenital heart surgery.
Materials and methods
This retrospective observational study was approved by the Institutional Review Board. Between July, 2011 and July, 2012, 41 patients who underwent operations due to congenital heart disease were included in the study. Of these patients with X-ray evidence of atelectasis, 26 received dornase alpha treatment. As a control group, 15 patients who were treated with conventional medications were chosen. All patients in the study protocol were under conventional treatment methods to prevent and clean mucus plug, such as frequent changing of positions, chest physiotherapy, endotracheal and tracheal aspiration, and inhaled salbutamol and inhaled N-acetylcysteine during the post-operative follow-up. If the patient did not respond to the conventional treatment methods after 24 hours, they were treated with dornase alpha according to the attendant's choice. Whether or not a cardiopulmonary bypass was involved was considered irrelevant to the study. Exclusion criteria included premature birth (n = 3), congenital pulmonary problems (n = 4), tracheal malformations (n = 2), and neurological problems causing respiratory distress (n = 6). The dornase alpha was not delivered to patients with pneumothorax and haemoptysis.
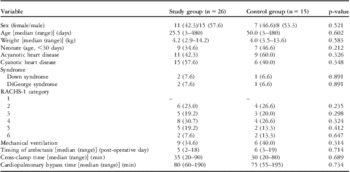
Pre-operative diagnoses of patients are presented in Table 1. The data were collected from the medical records of the paediatric cardiovascular surgery intensive care unit. The data reviewed included age, sex, weight, associated syndromes, mechanical ventilation support, the type and diagnosis of congenital anomalies, timing of post-operative atelectasis, and atelectasis scores. The operative data included lesion and type of repair by Risk Adjustment for Congenital Heart Surgery-1 risk category.Reference Jenkins, Gauvreau, Newburger, Spray, Moller and Iezzoni 6
Table 1 Pre-operative cardiac diagnoses of patients.

Data are presented as the number of patients (%)
In the study group, a single dose of 0.1 mg/kg dornase alpha (Pulmozyme®; Roche, Basel, Switzerland) was administered twice daily intratracheally in intubated patients and 2.5 mg of dornase alpha was delivered twice daily by nebulisation.Reference Boeuf, Prouix, Morneau, Marton and Lacroix 4 , Reference Merkus, de Hoog, van Gent and de Jongste 7 , Reference Hendriks, de Hoog, Lequin, Devos and Merkus 8 Medication was diluted with 5 ml of 0.9% NaCl, and administered endotracheally or as an inhalant using a jet nebuliser and high-flow oxygen for at least 30 minutes. For intubated patients, the respiratory rate per minute was determined as the total number of assisted and detected respirations while mechanical ventilator was set to the trigger 2 setting. In the study group, dornase alpha treatment was given 2 or 3 days depending on the improvement of atelectasis. If no improvement was observed, the delivery of dornase alpha was stopped after 3 days. Pulmonary findings of atelectasis were scored using anteroposterior chest X-rays 24 hours after administering the last dose of dornase alpha in all patients. The scores after treatment with dornase alpha were compared with the scores before treatment. In the control group, atelectasis scores before the diagnosis of atelectasis and 3 days after conventional treatment were compared. All patients received dornase alpha while they were in the intensive care unit.
Post-operative anteroposterior chest X-rays were taken before and 24 hours after treatment with dornase alpha. They were taken with the patients in the supine position using a portable X-ray machine. Results were scored by two independent radiologists unaware of group assignment using a Radiological Atelectasis Scoring system.Reference Hendriks, de Hoog, Lequin, Devos and Merkus 8 This system scored atelectasis, hyperinflation, and mediastinal shift. A partial atelectasis of one pulmonary lobe was scored as 1 point, and complete atelectasis of one lobe was marked as 2 points. The distinction between infiltrate and atelectasis was made by the radiologist. The presence or absence of hyperinflation was marked as 1 point or 0 points, respectively. The presence or absence of a mediastinal shift was scored as 1 or 0. The scores were then summed for each chest X-ray in each patient.
The results of blood gas analysis including pH, pO2, pCO2, and lactate levels were recorded in both groups. In all patients, heart rate, oxygen saturation, respiratory rate, arterial blood pressure, mechanical ventilator parameters, arterial blood gases, and lactate values were assessed before and 2 hours after the treatment. The results of blood gas analysis of the control groups were compared with the results of study group, which were recorded 24 hours after administering the last dose of dornase alpha. Charts were reviewed to identify potential side effects – voice alteration, laryngitis, pharyngitis, dyspepsia, and facial oedema – of dornase alpha.
Statistical analyses were performed using SPSS for Windows (Version 11.5, SPSS Inc., United States of America) software package. Fisher's χ2 and Mann–Whitney U tests were used for the comparison of groups, and Wilcoxon test was used for repeated consecutive measurements. Statistical significance was set to p < 0.05.
Results
Pre-operative cardiac diagnoses of patients are presented in Table 1. In the study group, 15 (57.7%) patients were operated on because of cyanotic and 11 (42.3%) patients were operated on because of acyanotic congenital heart disease. In the study group, nine (60.0%) patients were operated on because of cyanotic and six (40.0%) patients were operated on because of acyanotic congenital heart disease.
In the study group, pulmonary atelectasis was diagnosed at a median period of 5 (2–18) days after operations. In the control group, atelectasis was diagnosed at a median period of 6 (3–19) days after operations. There were no significant differences in terms of age, weight, gender, and the number of patients who were under mechanical ventilation between the study and control groups. Pre-operative characteristics are presented in Table 2.
Table 2 Pre-operative characteristics.

RACHS-1 category = risk adjustment for congenital heart surgery
Data are presented as the number of patients (%)
There was no difference in the operative data and Risk Adjustment for Congenital Heart Surgery-1 category between the groups (Table 2). Median and range value of Risk Adjustment for Congenital Heart Surgery-1 category in the study and control groups were 4 (2–6) and 4 (2–6), respectively. Cardiopulmonary bypass was used in 19 (73.0%) patients in the study group and in 12 (80.0%) patients in the control group (p < 0.05). There were no significant differences in cross-clamp and cardiopulmonary bypass times between the study and control groups.
There was a statistically significant decrease in heart rate and respiratory rate per minute, and a significant increase in oxygen saturation following dornase alpha administration (p < 0.05). In the control group, the changes were not statistically significant.
Comparison of arterial blood gas analysis and atelectasis scores before and after treatment in the groups is presented in Table 3. Although a significant decrease in atelectasis scores and increase in arterial pO2 level were observed following the administration of dornase alpha, there was no significant change in the control group. In the study group, the median atelectasis score decreased from 3.4 (1–6) to 0.8 (0–3) (p = 0.001). The median pO2 level increased from 69 (17–142) mmHg to 89 (30–168) mmHg (p = 0.04).
Table 3 Comparison of blood gas analysis and atelectasis scores.

Data are presented as median (minimum–maximum) values
In the study group, post-operative atelectasis was observed in the superior-right lobe in 12, middle-right lobe in 19, inferior-right lobe in 20, superior-left lobe in 11, and inferior-left lobe in 15 patients. Of 26 patients, 20 received 3 days of dornase alpha treatment, four received 2 days, and two received 1 day of treatment. After dornase alpha treatment, there was an improvement in chest X-rays in 21 (80.7%) out of 26 patients in the study group. The remaining five patients showed no significant change. In the control group, atelectasis was observed in the superior-right lobe in six, middle-right lobe in two, inferior-right lobe in two, superior-left lobe in three, and inferior-left lobe in two patients. Chest X-rays improved in eight patients, but it did not change in the remaining seven patients.
Side effects of dornase alpha were also checked in patient charts. In the study group, oedema involving the face was observed after administering dornase alpha in one case, which subsided following treatment with antihistamines and steroids. There were three patients who required intubation because of persistent atelectasis during dornase alpha administration. Although there were no improvements in the chest X-rays of two patients, chest X-ray of the third patient worsened. A significant increase in acute phase reactants was observed in all three of these patients, and empirical broad spectrum antibiotic treatment considering the possibility of infection was started. One of these patients with transposition of the great arteries died a week after the dornase alpha treatment because of severe septicaemia. The other two patients were discharged with a favourable outcome.
Discussion
Atelectasis is a clinical condition, particularly observed frequently in neonates and children who underwent congenital heart surgery. This morbidity can be associated with excessive and viscous pulmonary secretions and it presents with associated respiratory symptoms. Accumulation of mucus causes susceptibility to pulmonary and systemic infections, causing prolonged need for mechanical ventilation and hospitalisation.Reference Riethmueller, Kumpf and Borth-Bruhns 1 – Reference Boeuf, Prouix, Morneau, Marton and Lacroix 4 Therefore, the efficacy of dornase alpha as a mucolytic agent in the treatment of atelectasis is of clinical importance for improved post-operative outcome of patients who underwent congenital heart surgery.
Hyperviscosity is the most important factor in the development of atelectasis, and its aetiopathology is multifactorial. Various factors such as pneumonia-related surfactant deficiency, systemic inflammatory response following cardiopulmonary surgery, barotrauma from mechanical ventilation, young age, low blood count, and use of diuretics may lead to development of atelectasis.Reference Merkus, de Hoog, van Gent and de Jongste 7 – Reference Erdeve, Uras, Atasay and Arsan 9 As a frequent component of pulmonary atelectasis, mucus plugs contain high amounts of deoxyribonucleic acid. As a polyanion molecule complex, deoxyribonucleic acid is responsible for the viscosity and cohesiveness of pulmonary secretions. The recombinant human DNase or dornase alpha transforms mucus from a viscous gel to liquid by hydrolysing the extracellular deoxyribonucleic acid in the mucus.Reference Riethmueller, Borth-Bruhns and Kumpf 2 – Reference Boeuf, Prouix, Morneau, Marton and Lacroix 4
In the management of pulmonary secretions, respiratory physiotherapy and inhaled bronchodilator treatment are not always sufficient to treat mucus plugs, and thus alternative options need to be evaluated. Recent studies in the literature showed that dornase alpha can be used for the treatment of mucus plugs in cases other than cystic fibrosis.Reference Merkus, de Hoog, van Gent and de Jongste 7 – Reference Erdeve, Uras, Atasay and Arsan 9 Merkus et alReference Merkus, de Hoog, van Gent and de Jongste 7 indicated that atelectasis improved following dornase alpha in patients, who developed atelectasis owing to serious respiratory syncytial virus infection. Erdeve et alReference Erdeve, Uras, Atasay and Arsan 9 reported that 10 out of 12 cases (83%) included in their study showed rapid clinical and radiological improvement, and the remaining two cases, who did not respond to the 3-day nebule treatment, improved after endotracheal application of mucolytic agent. The use of dornase alpha clinically decreased respiratory rate and O2 need in neonates with resistant atelectasis, and laboratory work-up showed improved chest X-ray atelectasis scores and arterial blood gas levels.Reference Erdeve, Uras, Atasay and Arsan 9 Hendriks et alReference Hendriks, de Hoog, Lequin, Devos and Merkus 8 used a single nebule dose of dornase alpha per day in a total of 16 children without cystic fibrosis. Of these cases, five were operated on because of congenital heart disease, and 11 had non-cardiac conditions. It was reported that clinical and radiological improvements were observed 2 hours after the treatment with dornase alpha.Reference Hendriks, de Hoog, Lequin, Devos and Merkus 8 Moreover, in a study of 63 patients by Riethmueller et al,Reference Riethmueller, Borth-Bruhns and Kumpf 2 56 patients who underwent congenital heart surgery were given dornase alpha intratracheally. The authors reported that the treatment with dornase alpha shortened duration of hospitalisation.Reference Riethmueller, Borth-Bruhns and Kumpf 2
In our study, all of the 26 cases who underwent congenital heart surgery were between the ages of 3 and 480 days. There were significant improvements in the pulmonary and clinical findings of the patients following treatment with dornase alpha. Of these patients, 21 showed radiological, and 18 showed clinical improvements. There were four cases who had no radiological improvements, and five cases showed no clinical improvements. There was one case who showed radiological and three cases who showed clinical worsening. The acute phase reactant levels were increased in these radiologically and clinically worsened patients. Therefore, the emergence of these worsenings leads us to consider concomitant infections, even though blood culture results showed no growth. After 1 week of completion of the dornase alpha treatment, one of the patients died. All patients who received dornase alpha while intubated were disconnected from mechanical ventilators within 24 to 72 hours. There were three cases who received dornase alpha while extubated who required mechanical ventilator support.
In the literature, there is still no consensus on the dosage and administration method of dornase alpha that is used for the treatment of atelectasis. Boeuf et alReference Boeuf, Prouix, Morneau, Marton and Lacroix 4 instilled 0.1 mg/kg rhDNase intratracheally twice daily. Hendriks et alReference Hendriks, de Hoog, Lequin, Devos and Merkus 8 used two separate methods: 2.5 mg dornase alpha twice daily by spontaneous respiration through a nebuliser, and endotracheal administration of 10% of the dose in 5 ml 0.9% NaCl twice daily in the form of small droplets. El Hassan et alReference El Hassan, Chess, Huysman, Merkus and de Jongste 10 administered 1.25 mg/dose twice daily with a nebuliser for over 15 minutes, or 1.25 mg single dose endotracheally in the liquid form. In our study, a single dose of 0.1 mg/kg dornase alpha was administered twice daily intratracheally in intubated patients and 2.5 mg of dornase alpha was delivered twice daily by nebulisation.Reference Boeuf, Prouix, Morneau, Marton and Lacroix 4 , Reference Merkus, de Hoog, van Gent and de Jongste 7 , Reference Hendriks, de Hoog, Lequin, Devos and Merkus 8 Medication was diluted with 5 ml of 0.9% NaCl, and administered endotracheally or as an inhalant using a jet nebuliser and high-flow oxygen for at least 30 minutes. It has been reported that dornase alpha can cause various side effects, such as changes in vocal sounds, laryngitis, dyspepsia, and facial oedema.Reference Bryson and Sorkin 11 We observed only one case with facial oedema in our study.
Study limitations
The current study was conducted at a single centre with a limited number of cases. The retrospective nature of the study is another limitation. It would be more valuable to study this topic in a prospective randomised protocol with a larger patient population. The lack of an ideal scoring system for the evaluation of atelectasis affects objective assessment.
In conclusion, we suggest that the use of dornase alpha can be effective for the management of pulmonary atelectasis that develops following congenital heart surgery.
Acknowledgements
The authors thank Dr Burak Onan for assistance with design of the manuscript.
Financial Support
The authors received no financial support for the research and/or authorship of this article.
Conflict of Interest
None.
Ethical Standards
The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national guidelines on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008, and has been approved by the Institutional Committees of Istanbul Mehmet Akif Ersoy Thoracic and Cardiovascular Surgery Education and Research Hospital.