Introduction
Hallucinations constitute a common and distressing symptom of schizophrenia and numerous cognitive studies have aimed to investigate the mechanisms involved in their formation. The concept of source monitoring (Johnson et al. Reference Johnson, Hashtroudi and Lindsay1993) has been used repeatedly as a theoretical framework for these studies. This concept includes diverse functions such as reality monitoring, reality discrimination and self-monitoring, and has enabled the development of various paradigms (Larøi & Woodward, Reference Larøi and Woodward2007). Notably, one line of research has used the signal detection paradigm to investigate the propensity to report erroneously events that did not occur. Hallucinations, both clinical and non-clinical, have been linked to abnormal decision bias in acoustic signal detection tasks, resulting in increased rates of false detections of the signal (Bentall & Slade, Reference Bentall and Slade1985; Rankin & O'Carroll, Reference Rankin and O'Carroll1995; Barkus et al. Reference Barkus, Stirling, Hopkins, McKie and Lewis2007; Varese et al. Reference Varese, Barkus and Bentall2011). Our group has observed that hallucinations in schizophrenia patients or hallucination-prone participants are also associated with false recognitions of non-presented items in verbal memory and source memory tasks that required the recognition of target items among distracters (Brébion et al. Reference Brébion, Smith, Amador, Malaspina and Gorman1998, Reference Brébion, Amador, David, Malaspina, Sharif and Gorman2000, Reference Brébion, Larøi and van der Linden2010a). Thus, hallucinations seem to be linked to a liberal response bias in both online detection (reality discrimination) and memory (reality monitoring) of the events. The increased rate of false alarms in people with hallucinations suggests that the internal representations are mistaken for real occurrence of the events.
Considering the frequency of verbal hallucinations in schizophrenia, another fruitful approach has consisted of focusing on self-monitoring of language. Hallucinations have been related to misattribution of self-generated verbal material to another person in tasks that required remembering the source of the verbal items produced. The association was observed in schizophrenia patients (see Ditman & Kuperberg, Reference Ditman and Kuperberg2005 for a review) and also in non-clinical hallucination-prone participants (Larøi et al. Reference Larøi, van der Linden and Marczewski2004). Furthermore, clinical and non-clinical hallucinations have been associated with mistaking imagined or silently read verbal material for overtly spoken speech (Rankin & O'Carroll, Reference Rankin and O'Carroll1995; Franck et al. Reference Franck, Rouby, Daprati, Daléry, Marie-Cardine and Georgieff2000). All these studies corroborate the notion that hallucinated voices arise from defective monitoring of inner verbal thoughts (Jones, Reference Jones2010).
Another underdeveloped but potentially promising approach is to focus on the contextual information, which may be spatial or temporal, associated with the events. Processing or remembering the context in which the events have been encoded is essential to source monitoring (Johnson et al. Reference Johnson, Hashtroudi and Lindsay1993). Failure to integrate contextual information to form a complete memory representation of the events has been shown to be a core deficit in schizophrenia (Diaz-Asper et al. Reference Diaz-Asper, Malley, Genderson, Apud and Elvevåg2008; Talamini et al. Reference Talamini, de Haan, Nieman, Linszen and Meeter2010). It has been suggested that context-processing impairments are involved in the formation of certain psychotic symptoms including hallucinations (Servan-Schreiber et al. Reference Servan-Schreiber, Cohen and Steingard1996; Hemsley, Reference Hemsley2005). Despite scant experimental data regarding this issue, auditory hallucinations have been found to be associated with impairment in remembering the context – who performed the action and when – of the pairing of objects in two different sessions (Waters et al. Reference Waters, Badcock, Michie and Maybery2006). Our group observed previously that hallucinations were linked to list errors in free recall, a confusion that reflects failure to remember the temporal context of presentation of the stimuli (Brébion et al. Reference Brébion, Gorman, Amador, Malaspina and Sharif2002). More work is warranted to explore the link between hallucinations and context-processing impairment.
Source monitoring deficits of various kinds have been associated consistently with hallucinations and other positive symptoms. Their associations with negative symptoms might also be worthy of investigation. In our previous research on verbal and source memory, we observed, as we expected, that all the memory errors derived from our tasks were related to hallucinations and/or delusions (Brébion et al. Reference Brébion, Gorman, Amador, Malaspina and Sharif2002). An unexpected finding was that these errors were also inversely associated with certain negative symptoms, such as affective flattening and anhedonia from the Scale for the Assessment of Negative Symptoms (SANS) and emotional withdrawal, social withdrawal and lack of spontaneity from the Positive and Negative Syndrome Scale (PANSS). Higher ratings of these negative symptoms were associated with fewer memory errors, all stemming from self-monitoring, reality-monitoring or context-monitoring failure. In particular, negative symptoms were associated with fewer extra-list intrusions and list errors in free recall, and fewer false recognitions of non-produced items. They were also associated with fewer misattributions of one's own items to an external source and with a reduced tendency to remember mental visual images as perceived pictures. Although these findings are difficult to interpret, other groups have revealed similar inverse associations with negative symptoms. Recall intrusions were inversely associated with a global negative symptom score by Heinrichs & McDermid Vaz (Reference Heinrichs and McDermid Vaz2004) and with affective flattening by Turetsky et al. (Reference Turetsky, Moberg, Mozley, Moelter, Agrin, Gur and Gur2002). Stirling et al. (Reference Stirling, Hellewell and Ndlovu2001) reported that positive and negative symptoms had an opposite association with self-monitoring performance, negative symptoms being associated with less impairment.
In broad research on source memory in schizophrenia, we attempted to relate certain types of memory error with either auditory/verbal or visual hallucinations. We also wanted to replicate prospectively the finding of inverse associations between memory errors and certain negative symptoms, and extend it to other types of error. We used free recall of lists of words to investigate self-monitoring of language. Reality monitoring was studied through false recognitions of non-target words and pictures, and also through a paradigm designed to investigate confusion between imagined and perceived pictures. We put emphasis on the role of contextual information. Memory for temporal context was studied by requesting participants to remember the temporal locus of the presentation of target words, and memory for spatial context was studied by requesting participants to remember the setting of target pictures.
The general hypothesis underlying this work was that source memory errors were positively associated with hallucinations and inversely associated with affective flattening and/or anhedonia. The results derived from this study were published separately. In the current paper we synthesized all the data to provide a cohesive account of the pattern of associations of source memory errors with hallucinations and negative symptoms.
Method
Subjects
Forty-one patients with schizophrenia (eight in-patients) were recruited from the South London and Maudsley National Health Service (NHS) Foundation Trust, London. Sociodemographic and clinical information on the participants is presented in Table 1. Diagnosis was made on the basis of DSM-IV criteria by two experienced psychiatrists who used clinical interview, patients' history and chart review to reach a consensus. The patients were suffering primarily from chronic schizophrenia, with a disease duration of >12 months. Exclusion criteria for the study were any evidence of alcohol or drug abuse (DSM-IV criteria), organic mental illness or mental impairment, history of brain injury, and current severe physical illness. All but three patients were on daily antipsychotic medication.
Table 1. Sociodemographic data for the schizophrenia patients and healthy control subjects, and clinical data for the schizophrenia patients

M, Male; F, female; NART, National Adult Reading Test; SAPS, Scale for the Assessment of Positive Symptoms; SANS, Scale for the Assessment of Negative Symptoms.
Values given as mean (standard deviation), range.
Forty-three healthy control subjects were recruited by local advertisements and were screened by telephone interview to rule out any current or recent psychiatric history. The two groups were not significantly different with respect to age, gender distribution, ethnicity, education level and verbal IQ as assessed by the National Adult Reading Test (NART), which provides an estimation of pre-morbid IQ (p > 0.10 for all comparisons). Ethical approval for the study was obtained from the local hospital Research Ethics Committee. After a full explanation of the study, subjects provided written informed consent to participate.
Clinical ratings
Clinical assessments were conducted by psychiatrists. Videotape training in the relevant clinical rating scales was undertaken to achieve >90% inter-rater agreement in assigning subscale scores. Positive symptoms were assessed using the Scale for the Assessment of Positive Symptoms (SAPS). A global hallucination score was computed by summing the subscores for all types of hallucinations. Twenty-four patients had significant hallucinations in some modality, as reflected by a score ⩾2 on one or more of the hallucination items from the scale. In addition, scores obtained on the ‘auditory hallucinations’ item were tallied. Seventeen patients presented auditory hallucinations (score ⩾2 on the ‘auditory hallucinations’ item). A verbal hallucination score was computed by summing the scores obtained on the second and third items of the hallucination subscale (‘voices commenting’ and ‘voices conversing’). Twelve patients were classified as ‘voice hearers’ with a verbal hallucination score ⩾2. The ‘visual hallucinations’ score was also tallied and eight patients were classified as ‘visual hallucinators’ with a score ⩾2. Negative symptoms were assessed using the SANS, which includes affective flattening, alogia, avolition, anhedonia and disorders of attention. A score for each negative symptom was computed by summing the relevant subscale scores. Clinical symptom assessment and cognitive testing were conducted on the same day for most of the patients, and in all cases within a week of each other. The psychiatrists were blinded to cognitive results during clinical assessment. The experimenter (G.B.) was blinded to patients' symptoms during cognitive testing.
Verbal memory
The subjects were presented with four lists of 16 concrete mono- or bisyllabic words, equivalent in average number of syllables. Two of these lists were organizable into four semantic categories, with typical instances for one list and atypical instances for the other. The last two lists were non-organizable and were made up of eight high-frequency words and eight low-frequency words in random order. Two other equivalent non-organizable lists were used as distractors in the recognition task.
The lists of words were printed out. The subjects were presented with one list and informed that they had 45 s to learn the words. They were required to read the list aloud at least once so that the experimenter could ensure that all the items had been processed. The two non-organizable lists were administered first. Written free recall and recognition were required after the presentation of each list, following a 5-min delay for the first list and immediately after learning for the second. After the recognition of the second non-organizable list, a list discrimination task was administered. The subjects were read aloud in random order all the target words from both non-organizable lists and were required to indicate for each word whether it had been presented in the first or second list. Then the semantically organizable lists were administered and immediate written free recall was required after the presentation of each.
Measures
Free recall
The number of correctly recalled words was tallied for each list. The total numbers of extra- and intra-list intrusions across the four lists were also tallied.
Recognition
The number of correctly recognized target words and erroneously recognized distractor words were tallied. These measures were combined to compute for each condition (high- versus low-frequency words × immediate versus delayed recognition) a recognition index (Pr) reflecting the ability to discriminate target words from distractors and a response bias index (Br) reflecting the propensity to make false recognition of non-target words in case of uncertainty. Global Pr and Br indices were derived by averaging the indices across all conditions.
List discrimination
The number of list discrimination errors (items from the first list misattributed to the second list and vice versa) was computed for high- and for low-frequency words.
Visual memory
The subjects were presented with 16 pictures: eight of these were black and white (b/w) and eight colored. The pictures were laid on the table in groups of four mixed b/w and colored pictures, and displayed over 20 s. Each picture was placed next to a small card that constituted the spatial context, at four locations (top left, top right, bottom left, bottom right).
The subjects were instructed to watch the presented pictures, and informed that they would have to recognize them afterwards. They were also required to pay attention to the spatial context of each picture. After a delay of about 5 min, the 16 target pictures mixed with 16 equivalent distractor pictures were presented one by one in random order. The subjects were required to indicate for each picture whether it had been presented during the acquisition phase or was new. The recognition task was followed by a spatial context memory task. The four small cards that constituted spatial context were laid on the table again, at the same location as previously. The subjects were shown the 16 target pictures one by one in random order, informed that all of them had been presented, and required to remember for each picture which card it was associated with at the presentation phase.
Measures
Recognition
The numbers of recognized target pictures and false recognitions of new pictures were used to compute, for b/w and for colored pictures, a recognition index Pr reflecting the ability to discriminate target pictures from distractors and a response bias index Br reflecting the tendency to make false recognitions of non-target pictures.
Spatial context
The number of spatial context errors was tallied for b/w and for colored pictures.
Source memory
The participants were presented with two common instances from 16 semantic categories (for example PLUM and GRAPES for the category ‘Fruit’). One instance was presented as a picture with its verbal label whereas only the verbal label was displayed for the other instance. The subjects were requested to produce a third instance of the same semantic category and were not informed that they would have to remember the presented items afterwards. After a few minutes delay, the experimenter read aloud a list of 64 words including in random order the 32 target items mixed with 32 distractors from the same categories. The subjects were required to indicate for each item whether it had been presented as a picture, presented as a word or was new (recognition test). Then the experimenter read aloud the list of the 32 target items in random order. The subjects were informed that all of them had been presented and were required to indicate for each item whether it had been presented as a word or as a picture (reality monitoring test).
Measures
Recognition
The number of omissions for both types of item (word-stimuli and picture-stimuli reported as new) and the number of false recognitions for both types of item (new items reported as words and new items reported as pictures) were used to compute two recognition indices reflecting the ability to discriminate the target words and target pictures from distractors (Pr-words and Pr-pictures) and two response bias indices reflecting the tendency to report new items as words or as pictures (Br-words and Br-pictures).
Reality monitoring
The misattributions of target items to the wrong mode of presentation were combined according to the same formula. We computed a Pr index reflecting the ability to discriminate the items presented as words from those presented as pictures (Pr-imagination) and a Br index reflecting the tendency to report as pictures items that had been presented as words (Br-imagination).
Typicality of the category examples
The typicality of each of the 16 category examples provided by the subject during the presentation phase was rated according to norms, wherein a higher score is given for a more atypical response. An averaged typicality score was computed across the 16 responses.
The scores that did not follow a normal distribution were normalized by square-root or log transformation before data analysis. The relevant memory efficiency measures were controlled in all the presented correlations with the memory errors to ensure that the symptoms were specifically associated with the memory errors rather than with a general memory deficit. The NART score was also controlled in the tasks with verbal material to avoid confound of pre-morbid verbal IQ. Lastly, considering the expected opposite associations of hallucinations and certain negative symptoms with the memory errors, the sum of affective flattening and anhedonia scores was controlled in the study of the associations with hallucinations whereas the hallucination score was controlled in the study of the associations with negative symptoms.
Results
The various memory scores for patients and healthy controls are presented in Table 2. Most of the following associations with hallucinations and negative symptoms have already been published (see below). The figures might be slightly different from those presented in the original papers because of small differences in sample size or in the variables used as covariates. Indeed, in the current paper, we have controlled systematically the same variables to make the data analysis homogeneous. Novel complementary analyses were conducted on the number of temporal context errors to study their association with certain specific symptoms that were not investigated in the original report.
Table 2. Memory scores for the schizophrenia patients and healthy control subjects (mean and standard deviation). Positive associations of memory errors with hallucinations scores and inverse associations with negative symptoms (affective flattening and anhedonia)
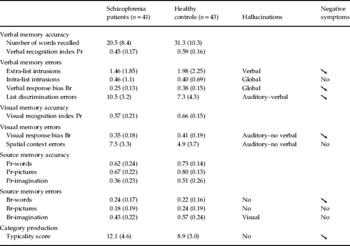
An arrow signifies that the memory error is inversely associated with affective flattening and anhedonia.
Verbal memory
Extra-list intrusions
In the subsample of 26 patients who made at least one extra-list intrusion error, the number of extra-list intrusions was strongly correlated with the verbal hallucination score (r = 0.60, p < 0.005), after controlling for the number of correctly recalled words, the NART score and the sum of affective flattening and anhedonia scores. The correlation with the visual hallucination score was near zero.
A negative correlation between anhedonia score and number of extra-list intrusions emerged in this subsample of 26 patients, after controlling for the number of correctly recalled words, the NART score and the verbal hallucination score (r = − 0.52, p < 0.015). In the subsample of 29 patients who did not suffer from verbal hallucinations, a significant negative correlation between affective flattening and number of extra-list intrusions was revealed after controlling for the number of correctly recalled words and the NART score (r = − 0.38, p < 0.05).
No significant association between the number of correctly recalled words and verbal hallucination, affective flattening or anhedonia scores was revealed.
Intra-list intrusions
In the subsample of 24 patients who presented hallucinations, a significant correlation between number of intra-list intrusions and global hallucination score emerged after controlling for number of correctly recalled words, NART score and sum of affective flattening and anhedonia scores (r = 0.52, p < 0.015). The correlation with verbal hallucination score did not reach statistical significance (r = 0.36, p > 0.11). No significant association between global hallucination score and number of correctly recalled words was revealed.
After partialling out the number of correctly recalled words, NART score and global hallucination score, the number of intra-list intrusions was not correlated with either affective flattening or anhedonia score in the whole sample. Furthermore, no correlation emerged in the subsample of patients without significant hallucinations.
The associations with extra- and intra-list intrusions have been reported in Brébion et al. (Reference Brébion, David, Bressan, Ohlsen and Pilowsky2009).
Response bias
In the subsample of 24 patients with hallucinations, we observed a significant correlation between the response bias Br and the global hallucination score, after controlling for the recognition index Pr, the NART score and the sum of affective flattening and anhedonia scores (r = 0.55, p < 0.01). The direction of this correlation indicates that higher hallucination scores were associated with an increased tendency to make false recognitions of non-presented words.
In the whole patient sample, after controlling for Pr, NART score and global hallucination score, the expected negative correlation between Br and affective flattening score only approached significance (r = − 0.30, p < 0.07). A significant negative correlation between Br and anhedonia score was revealed (r = − 0.36, p < 0.05). The direction of these correlations indicates that higher levels of affective flattening and anhedonia were associated, or tended to be associated, with fewer false recognitions of non-presented words. The magnitude of the correlation with affective flattening was increased in the subsample of 17 patients without hallucinations (r = − 0.47) whereas the correlation with anhedonia remained unchanged (r= −0.35).
The recognition index Pr was not significantly associated with either hallucination, affective flattening or anhedonia score. These results have been reported in Brébion et al. (Reference Brébion, David, Jones and Pilowsky2005) in 40 of the patients, with slight differences in the variables used as covariates.
Temporal context errors
We have reported (Brébion et al. Reference Brébion, David, Jones, Ohlsen and Pilowsky2007a) the results of a regression analysis conducted on the total number of list misattributions in the patient sample. The predictors were auditory/verbal hallucinations, visual hallucinations, delusions, alogia, avolition, sum of affective flattening and anhedonia scores, total number of recalled words and NART score. The auditory/verbal hallucination score was computed as the sum of three items: the ‘auditory hallucination’ item and the two items pertaining to voices. This auditory/verbal hallucination score made a significant contribution to the total number of list misattributions (β = 0.47, p < 0.025). We conducted complementary analyses, entering the ‘auditory hallucination’ item score and the verbal hallucination score alternately in the regression analysis instead of the global auditory/verbal hallucination score. Both of these hallucination scores made a significant contribution to the total number of list misattributions (β = 0.41, p < 0.05 in both cases). No significant association with the visual hallucination score emerged.
The sum of affective flattening and anhedonia scores was inversely associated with the total number of list misattributions, as expected, but only at a trend level of significance (β = − 0.34, p < 0.10). Analyses of the word frequency effect revealed that the sum of affective flattening and anhedonia scores was a strong significant negative predictor of the list misattributions of the high-frequency words (β = − 0.59, p < 0.01), but did not contribute to the misattributions of the low-frequency words (β = 0.09). In complementary analyses we replaced the sum of affective flattening and anhedonia scores by each of these symptom scores, alternately. The contribution of affective flattening to the list misattributions of the high-frequency words was marginally significant in the whole patient sample (β = − 0.45, p = 0.051) and enhanced in the subsample of 23 patients who did not present auditory/verbal hallucinations (β = − 0.60, p < 0.05). The contribution of anhedonia was significant in the whole sample (β = − 0.46, p < 0.025) and the magnitude of this inverse association was not altered in the subsample of patients without auditory/verbal hallucinations (β = − 0.46). The number of recalled high-frequency words was not significantly associated with either affective flattening or anhedonia score.
Visual memory
These results have been reported in Brébion et al. (Reference Brébion, David, Ohlsen, Jones and Pilowsky2007b).
Response bias
We computed the correlations between response bias and hallucination scores, after partialling out the Pr indices and the sum of affective flattening and anhedonia scores. In the subsample of 24 hallucinators, the average Br was significantly correlated with the auditory hallucination score (r = 0.45, p < 0.05). The direction of the correlation indicates that higher ratings of auditory hallucinations were associated with increased tendency to make false recognitions of non-target pictures, as expected. The correlation between average Br and the verbal hallucination score did not reach statistical significance (r = 0.16). The visual hallucination score was unrelated to the average Br (r near zero).
In the whole sample, after partialling out the Pr indices and the auditory hallucination score, affective flattening was not significantly associated with the average Br (r = − 0.14). A significant negative correlation between anhedonia and average Br was revealed (r = − 0.46, p < 0.005). This indicates that anhedonia was associated with reduced tendency to make false recognitions of non-target pictures, as expected. After controlling for the auditory hallucination score, anhedonia was not correlated with the Pr indices. We recomputed the correlations of response bias with affective flattening and anhedonia in the subsample of 17 patients who did not present any significant hallucinations, after removing the auditory hallucination score from the covariates. The negative correlation between Br and anhedonia was strengthened (r = − 0.64, p < 0.01). A trend for a negative correlation between Br and affective flattening emerged (r = − 0.48, p < 0.07).
Spatial context errors
We conducted correlational analyses between the total number of spatial context errors and the hallucination scores, after partialling out the Pr indices and the sum of affective flattening and anhedonia scores. In the subsample of 24 hallucinators, the total number of spatial context errors was significantly correlated with the auditory hallucination score (r = 0.49, p < 0.025). Thus, higher ratings of auditory hallucinations were associated with more errors in remembering the spatial context of picture presentation, as expected. The correlation between total number of spatial context errors and the verbal hallucination score was not significant (r = 0.19). No correlation with the visual hallucination score emerged.
Contrary to our expectations, the total number of spatial context errors was not significantly associated with either affective flattening or anhedonia score, in either the whole patient sample or the subsample of patients without hallucinations.
Source memory
These results have been reported in Brébion et al. (Reference Brébion, Ohlsen, Pilowsky and David2008), although the current analyses involve small modifications.
Recognition test
Recognition accuracy
Repeated-measure ANOVAs were used to compare the Pr indices for the recognition of words and pictures in each subgroup of patients with versus without auditory and visual hallucinations. When the eight patients with visual hallucinations were compared to the 33 other patients, the ANOVA did not reveal any significant effect of subgroup (F 1,39 = 0.14, n.s.). However, the interaction between subgroup of patients and presentation mode was significant (F 1,39 = 5.55, p < 0.025). Examination of the Pr indices indicates that the patients without visual hallucinations recognized the pictures better than the words (Pr-words = 0.62, Pr-pictures = 0.70), a picture superiority effect also observed in the healthy controls. By contrast, the patients with visual hallucinations recognized the words better than the pictures (Pr-words = 0.66, Pr-pictures = 0.59). When the 17 patients with auditory hallucinations were compared to the 24 other patients, the ANOVA revealed no effect of subgroup (F 1,39 = 0.06, n.s.) or interaction between subgroup and presentation mode (F 1,39 = 0.11, n.s.).
Response bias
Correlations between hallucination scores and response bias were computed in the subsample of 24 patients with hallucinations. The NART score, the corresponding Pr index and the sum of affective flattening and anhedonia scores were partialled out. The visual hallucination score was not significantly correlated with Br-words and its correlation with Br-pictures was near zero.
We then computed the correlations between response bias and affective flattening and anhedonia scores, after controlling for the NART score and the corresponding Pr index. No significant correlation with either Br-words or Br-pictures was revealed in the whole sample. In the subsample of 17 patients without hallucinations, after the Br indices were normalized, Br-words correlated negatively and significantly with affective flattening (r = − 0.61, p < 0.025) and with anhedonia (r = − 0.53, p < 0.05). No significant correlation with Br-pictures was revealed. There was no association between Pr-words and affective flattening or anhedonia.
Reality-monitoring test
After controlling for the NART score, Pr-imagination and the sum of affective flattening and anhedonia scores, the correlation between Br-imagination and auditory hallucination score was near zero in the subsample of 24 patients with hallucinations. By contrast, a significant correlation between Br-imagination and the visual hallucination score was revealed (r = 0.56, p < 0.01), indicating that higher ratings of visual hallucinations were associated with an increased tendency to remember the target words as pictures. The visual hallucination score was not associated with Pr-imagination.
Associations between Br-imagination and negative symptoms were studied in the whole patient sample after controlling for the NART score, Pr-imagination and visual hallucination score. Contrary to our expectations, Br-imagination was not associated with either affective flattening or anhedonia. Furthermore, there was no association in the subsample of patients without hallucinations.
Typicality of the category examples
The category examples produced by the patients at the presentation phase were more atypical than those produced by the healthy controls [mean = 12.1 (s.d. = 4.6) v. mean = 8.9 (s.d. = 3.0), t(82) = 3.75, p < 0.0001]. The typicality score was not associated with hallucinations in patients. Regression analyses involving depression score, NART score, and each negative symptom alternately, revealed that affective flattening (β = − 0.32, p < 0.05), alogia (β = − 0.38, p < 0.025) and anhedonia (β = − 0.51, p < 0.001) made significant negative contributions to the typicality score. The direction of the association indicates that higher ratings of these symptoms were associated with more typical responses. These results are reported in Brébion et al. (Reference Brébion, Bressan, Ohlsen, Pilowsky and David2010b).
Discussion
The integrative source monitoring framework, with its various components, has provided a fruitful approach to the investigation of the cognitive bases of hallucinations. In line with the reality-discrimination/reality-monitoring theory, several studies have revealed an association between hallucinations and false detections of acoustic signals (Bentall & Slade, Reference Bentall and Slade1985; Rankin & O'Carroll, Reference Rankin and O'Carroll1995; Barkus et al. Reference Barkus, Stirling, Hopkins, McKie and Lewis2007; Varese et al. Reference Varese, Barkus and Bentall2011). Our group had previously reported that hallucinations are associated with false recognitions of words in a memory task (Brébion et al. Reference Brébion, Smith, Amador, Malaspina and Gorman1998, Reference Brébion, Amador, David, Malaspina, Sharif and Gorman2000, Reference Brébion, Larøi and van der Linden2010a). The current findings corroborate this latter observation (Brébion et al. Reference Brébion, David, Jones and Pilowsky2005) and extend it to false recognitions of pictures (Brébion et al. Reference Brébion, David, Ohlsen, Jones and Pilowsky2007b). The association between hallucinations and liberal response bias towards either detecting or remembering events therefore seems to be a consistent result, encompassing a variety of materials and procedures. This suggests that, in people with hallucinations, the internal representations of the events are readily mistaken for real events. It should be noted that, in our previous studies as well as in the current one, the correlation between hallucination score and response bias in yes/no recognition tasks emerged only (Brébion et al. Reference Brébion, Amador, David, Malaspina, Sharif and Gorman2000, Reference Brébion, David, Ohlsen, Jones and Pilowsky2007b, Reference Brébion, Larøi and van der Linden2010a), or was greatly enhanced (Brébion et al. Reference Brébion, Smith, Amador, Malaspina and Gorman1998, Reference Brébion, David, Jones and Pilowsky2005), in a subsample of participants with significant clinical or non-clinical hallucinations. This might partially explain the negative results in certain studies.
Numerous studies have shown an association between auditory–verbal hallucinations and disruption in the self-monitoring of language. Examples of such disruption are the extra-list intrusions in free recall, which reflect misattribution of internally produced words to the experimental list. In our data, extra-list intrusions were associated with verbal hallucinations (Brébion et al. Reference Brébion, David, Bressan, Ohlsen and Pilowsky2009). Moritz et al. (Reference Moritz, Heeren, Andresen and Krausz2001) reported an association between intrusions and positive symptoms in a schizophrenia sample. Intrusions have been associated with hallucinations in adolescents with psychosis (Doré et al. Reference Doré, Caza, Gingras, Maziade and Rouleau2009) and with proneness to hallucinations in a non-clinical sample (Brébion et al. Reference Brébion, Larøi and van der Linden2010a). These findings are compatible with the view that verbal hallucinations arise from confusion between internal verbal thoughts and perceived speech. Such confusion might stem from anomalous auditory imagery or unawareness of self-generated speech (Seal et al. Reference Seal, Aleman and McGuire2004). Brain imaging studies of patients with auditory–verbal hallucinations have shown attenuated activation of areas putatively involved in the self-monitoring of inner speech (Allen et al. Reference Allen, Larøi, McGuire and Aleman2008). A recent meta-analysis indicates that patients with auditory hallucinations are especially impaired in recognizing their own items or actions as being self-generated, relative to the other patients (Waters et al. Reference Waters, Woodward, Allen, Aleman and Sommer2012).
Visual hallucinations are less prevalent than voices and their cognitive correlates have received little investigation. However, it might be assumed that visual hallucinations similarly consist of the mistaking of mental visual images for real events. Accordingly, we observed that our patients with visual hallucinations showed a propensity to report that they had seen pictures of items whereas only the verbal label of these items had been displayed (Brébion et al. Reference Brébion, Ohlsen, Pilowsky and David2008). This suggests that the conveyed mental images were later remembered as perceived pictures. Moreover, in the recognition component of the task, the patients without visual hallucinations and the healthy controls unsurprisingly recognized the target pictures better than the target words. The patients with visual hallucinations, however, failed to demonstrate this classic picture superiority effect. In fact, they were poorer in recognizing the pictures than in recognizing the words. This might suggest that the abnormal salience of mental visual images stored in memory interferes with the encoding of presented common pictures. Thus, visual hallucinations might be linked to either excessive production of visual imagery or readiness to mistake mental images for percepts. Both verbal and visual hallucinations in schizophrenia would therefore be the product of internally generated material: speech or visual images (Bentall, Reference Bentall1990). This internal/external confusion might also apply to healthy individuals prone to hallucinations. Aleman et al. (Reference Aleman, Nieuwenstein, Bocker and de Haan2000) reported that these individuals demonstrated closer intercorrelations between imagery and perception performance compared with the other healthy participants. Our data have extended to internal visual images the previously reported conclusions on the alleged involvement of internal speech. It would be interesting to corroborate this theory by investigating the contribution of imagery for odors to the formation of olfactory hallucinations.
An innovative aspect of our work was to explore the failure to remember contextual information as another potential cognitive substrate of hallucinations. We observed that auditory hallucinations were associated with errors in remembering the temporal context of word presentation (Brébion et al. Reference Brébion, David, Jones, Ohlsen and Pilowsky2007a). This is in agreement with Waters et al. (Reference Waters, Badcock, Michie and Maybery2006) who reported that auditory hallucinations were associated with impairment in remembering the context of performing actions, although in their task ‘context’ referred not only to the temporal locus of the action but also to its agent. Auditory hallucinations in our study were also associated with errors in remembering the spatial context of picture presentation (Brébion et al. Reference Brébion, David, Ohlsen, Jones and Pilowsky2007b). Failure to process the context in which the events are presented might be crucial in the formation of auditory hallucinations. Patients suffering from this symptom seem unable to properly bind the encoded information with its particular context when they recall the event. Memory for contextual information in schizophrenia patients should be the object of further research.
Although the source monitoring framework has been used repeatedly for the study of hallucinations, associations with negative symptoms are generally not sought. In previous research we observed that certain negative symptoms were associated with fewer of a variety of memory errors (Brébion et al. Reference Brébion, Gorman, Amador, Malaspina and Sharif2002). These associations were unexpected and might have been an artifact. However, in the current study, affective flattening and anhedonia were indeed associated with decrement in various types of memory error, including errors not investigated in our previous study. They were associated with a decreased tendency to make false recognitions of words in both a word-recognition (Brébion et al. Reference Brébion, David, Jones and Pilowsky2005) and a source-recognition (Brébion et al. Reference Brébion, Ohlsen, Pilowsky and David2008) task, in line with our previous results. We extended these findings on response bias by showing that affective flattening and anhedonia were also associated with a decreased tendency to make false recognitions of pictures (Brébion et al. Reference Brébion, David, Ohlsen, Jones and Pilowsky2007b). Furthermore, they were associated with fewer extra-list intrusions (Brébion et al. Reference Brébion, David, Bressan, Ohlsen and Pilowsky2009), corroborating our previous observation and also that from other groups (Turetsky et al. Reference Turetsky, Moberg, Mozley, Moelter, Agrin, Gur and Gur2002; Heinrichs & McDermid Vaz, Reference Heinrichs and McDermid Vaz2004). Temporal context errors were also inversely associated with affective flattening and anhedonia (Brébion et al. Reference Brébion, David, Jones, Ohlsen and Pilowsky2007a), although spatial context errors were not. Lastly, these negative symptoms were associated with decrement in a type of abnormality unrelated to source memory dysfunction, namely atypicality in category instance production (Brébion et al. Reference Brébion, Bressan, Ohlsen, Pilowsky and David2010b). Minor et al. (Reference Minor, Cohen, Weber and Brown2011) recently reported that atypicality of produced semantic exemplars was inversely related to a negative symptom score made up of the ‘no close friends’ and ‘constricted affect’ subscales, in schizotypal individuals.
The inverse association between certain negative symptoms and cognitive abnormalities therefore seems to be a genuine phenomenon. Nonetheless, understanding its meaning is challenging. This association is opposite to that of hallucinations, which have been consistently related to more memory errors. It could be argued that chronic patients with prominent negative symptoms make fewer memory errors merely because they are more likely to have their positive symptomatology stabilized with medication. However, this does not seem to be the case in our sample because affective flattening and anhedonia were, on the contrary, associated with more hallucinations. The inverse association with negative symptoms does not seem to be contingent upon the existence of an association with hallucinations in any event. Indeed, all the associations of memory errors with affective flattening, and certain associations with anhedonia, were either observed exclusively or enhanced in the subsample of the patients who did not present the target hallucination symptom. Furthermore, the associations of memory errors with negative symptoms did not always mirror their associations with hallucinations. Certain errors were increased along with hallucinations but did not decrease along with negative symptoms, and vice versa (see Table 2). Thus, although hallucinations and negative symptoms showed opposite associations with most of the errors studied, these opposite associations seem to be independent of each other.
Considering the whole pattern of data, it might be concluded that these negative symptoms are associated with decrement in three types of cognitive abnormality: (1) false recognitions in a yes/no recognition task. The observed decrement might be due to strengthened inhibition of the mechanisms that allow commission errors; (2) certain of the errors that stem from source memory failure rather than from poor inhibition; we would tentatively propose that the inverse association with negative symptoms emerges when the source memory error in question is positively associated with hearing voices (as was the case for extra-list intrusions and list misattributions of target words) but not when hearing voices is unrelated to it (as was the case for intra-list intrusions, spatial context errors and remembering the verbal referents of items as if they were pictures); and (3) atypicality in the production of category examples. Other types of cognitive abnormality might be investigated. It would also be worth determining the associations with a broader range of negative symptoms to confirm our observation that only the negative symptoms reflecting diminished emotion or social interactions are involved in these inverse associations.
An important limitation of the study is the relatively small number of participants, especially when subdivided according to specific symptoms. Our reliance upon correlations is another limitation because correlations cannot, of course, provide definite evidence of causality. Furthermore, the procedure did not enable us to determine whether the observed aberrations in patients with hallucinations are trait or state related. A large number of analyses was also presented, raising the issue of spurious significant results, although we obtained a consistent and meaningful pattern of findings that is unlikely to arise by mere chance. Finally, we cannot rule out a possible role of medications on the observed associations.
In summary, this study has enabled better characterization of the associations between hallucinations and source memory failure in schizophrenia. We have extended the role of reality discrimination of ongoing events to that of reality monitoring of past events. Our results further suggest that, whereas verbal hallucinations arise from failure to monitor internal thoughts, visual hallucinations arise from failure to monitor internal visual images. The study also demonstrates the contribution of impaired processing or remembering of contextual information. In addition, our findings reveal that several of the tallied source memory errors are inversely related to affective flattening and anhedonia.
Further studies might manipulate the emotional valence of the experimental stimuli to incorporate the role of emotion in the associations between clinical symptoms and memory errors (Larøi & Woodward, Reference Larøi and Woodward2007). Although the involvement of source monitoring in the formation of hallucinations finds support in many studies, other potential cognitive underpinnings should be investigated as well, such as cognitive disinhibition (Waters et al. Reference Waters, Badcock, Maybery and Michie2003; Soriano et al. Reference Soriano, Jiménez, Román and Bajo2009; Badcock & Hugdahl, Reference Badcock and Hugdahl2012). Finally, longitudinal studies could be conducted with patients being tested both in the acute state of hallucinations and after their remission. This would enable us to determine which mechanisms are specific to the hallucinations themselves compared with the predisposition to hallucinations.
Acknowledgments
This study was conducted in collaboration with Professor L. Pilowsky. The work was supported by grants from the Bial Foundation, the British Academy, the National Alliance for Research on Schizophrenia and Depression, and the Wodecroft Foundation.
G. Brébion is currently affiliated with the Unit of Research and Development, Parc Sanitari Sant Joan de Déu and Cibersam, Barcelona, Spain.
Declaration of Interest
None.




