INTRODUCTION
The rectangularization of the survival curve in most industrialized countries means that a very large proportion of the population dies at a very advanced age. In Sweden, for example, ~50% of deaths occur at ≥80 years of age (National Board of Health and Welfare, 2006). It is therefore surprising that research on the end stage of life has focused mainly on young, middle-aged, or, at most, young-old people. Knowledge based on middle-aged or younger individuals or specific diseases may be of limited value for understanding of the end of life among the oldest old, who experience predominantly chronic illnesses (Hallberg, Reference Hallberg2006). Most studies about the elderly focus on special conditions such as cancer (Di Mauro et al., Reference Di Mauro, Scalia and Leotta2000; Sutton et al., Reference Sutton, Demark-Wahnefried and Clipp2003). There are many unmet needs among elderly, dying individuals, including symptom relief and emotional support. The few reviews addressing end-of-life care of elderly (Ahmed et al., Reference Ahmed, Bestall and Ahmedzai2004; Hallberg, Reference Hallberg2006; Liptzin, Reference Liptzin2006; National Board of Health and Welfare, 1997; Raymond & Woo, Reference Raymond and Woo2001) demonstrate a need for improved knowledge. Therefore, there is a need for more general investigations about the oldest old and end-of-life care.
Across cultures, there are differences in the typical locations where older people die. In Sweden, all eldercare is subsidized and provided almost entirely by municipal facilities; individuals' needs are always assessed before moving them to an institution. The municipalities also assess, subsidize, and run the Home Help Services, which is provided in the community, whereas county councils subsidized and ran medical care provided in the home of the elderly individuals in the community. Therefore, it is possible to study care trajectories during the last year of life and location at death without any economic considerations.
In Sweden, >50% of those who die at ≥ 65 years of age die in hospital; this number has remained quite stable during the last two decades (National Board of Health and Welfare, 2005, 2006). In a study of deceased persons ≥80 years of age, Andersson et al. (1999) found that even if 45% had been staying at a hospital at the time of death, 74% had lived in some kind of eldercare institution at one time. These findings are similar to other studies in Sweden (National Board of Health and Welfare, 2006; Rinell Hermansson, Reference Rinell Hermansson1990) and other countries (Teno et al., Reference Teno, Clarridge and Casey2004).
Research has identified several important long- and-medium term factors related to mortality with advancing age, including health, activities of daily life (ADL), and social networks. The ability to perform ADL tends to decline with advancing age (Allen et al., Reference Allen, Foster and Berg2001; Covinsky et al., Reference Covinsky, Palmer and Fortinsky2003a; Davey et al., Reference Davey, Johansson and Malmberg2006; Hellström & Hallberg, Reference Hellström and Hallberg2001), but the trajectory of this decline can vary. Covinsky et al. (Reference Covinsky, Eng and Lui2003b) found that it is slow and progressive, whereas Li (Reference Li2005) found it accelerates before death. A longitudinal study, performed over 4 years, of the oldest old (≥86 years of age) demonstrated significant declines in ADL and objective health over the 4 years that preceded mortality, whereas subjective health did not decline. However, survivors estimated their health as significantly better at baseline, suggesting a possible reduction in perceived health in relation to death, even if the pattern of terminal decline was more apparent for objective health and ADL (Ernsth Bravell et al., Reference Ernsth Bravell, Berg and Malmberg2007). Diehr et al. (Reference Diehr, Williamson and Burke2002) reported that the dying process has a significantly greater effect on health than does aging, suggesting that large declines in health are due to former and not the latter. Murata et al. (Reference Murata, Takaaki and Tamakoshi2006) demonstrated that there is a complex relationship between health, functional ability, and mortality among the oldest old.
Several studies have shown that social networks are related to mortality in the elderly (Augustsson et al., Reference Augustsson, Matousek and Eriksson2003; Eriksson et al., Reference Eriksson, Hessler and Sundh1999; Murata et al., Reference Murata, Takaaki and Tamakoshi2006). There are gender differences in the relationships between social networks and mortality in elderly individuals; social relationships may serve different functions for men and women (Avlund et al., Reference Avlund, Damsgaard and Holstein1998). Some research suggests that social ties can improve health or protect against disability in old age (Avlund et al., Reference Avlund, Lund and Holstein2004; LaPlante et al., Reference LaPlante, Kaye and Kang2004; Mendes de Leon et al., Reference Mendes de Leon, Glass and Beckett1999). Other research suggests that elderly who are disabled and ill receive more help from their social network, resulting in a higher frequency of contact with family, relatives, and friends (Bertera, Reference Bertera2003; Hyduk, Reference Hyduk1996). Poor functional capacity may be related to low levels of social activity (Litwin, Reference Litwin2003; Stuck et al., Reference Stuck, Walthert and Nikolaus1999).
Although there are a number of studies on predictors of survival in old age, only a few have focused on care trajectories, social networks, health, and functional ability of the oldest old during the last year(s) of life. The aim of this study was to describe the last year of life of a sample of the oldest old, focusing on end-of-life care and its trajectories, status of health, social networks, and ADL.
METHODS
Sample
Data originated from the NONA study, a longitudinal study of oldest old individuals living in a Swedish municipality. Three hundred people from the Swedish population registry, aged 86 years, 90 years, or 94 years (100 from each age group), were randomly selected; 193 agreed to participate in the study. One hundred fifty-seven could themselves provide information about their health, social network, ADL, and pattern of care. Thirty-six were unable to respond themselves due to severe illness and/or cognitive problems and instead participated by proxy. For this presentation, 102 relatives (referred to as proxies) to the oldest old individuals participated in a telephone interview, after the death of the oldest old individuals.
Procedures and Design
The main NONA study had longitudinal design with the first in-person interview in 1999 (where 157 participated on their own, and 36 by proxies), in addition, there were two in-person follow-up interviews in 2001 and 2003. The interview with the old individuals included a question about their closest relative, and asked if we were allowed to contact the relative for a telephone interview. In those 36 cases where proxies were used, they were asked if they were willing to participate in an interview after the oldest old individual's death.
Between 1999 and 2003, 109 respondents died. Approximately one month after the time of death, relatives were contacted and invited to participate in a telephone interview about the family member's/relative's/friend's last year of life. One hundred two proxies agreed to participate in the interview; most were relatives, primarily daughters (48) and sons (29), but also daughters-in-law (5), nieces and nephews (5), sisters (2), wives (2), sister-in-laws (1), and cousins (1). Eight proxies were guardians, and one was a good friend. The interviews with proxies to the deceased respondents were performed parallel to the NONA study, from 1999 to 2003. The oldest old individuals' situations at the time of death are presented in Table 1.
Table 1. Description of the old individual, based on the location at the time of death
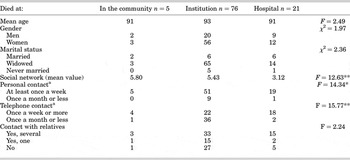
a with children, n = 86.
*p < 0.05.
**p < 0.01.
In-person Interview with the Oldest Old
Interviews with the oldest old individuals took place as part of the main NONA study and were performed at the place of residence by trained, registered nurses. The initial in-person interview took place in 1999 and follow-ups were performed in 2001 and 2003.
The oldest old individuals were asked to report the number of diseases and/or symptoms that they had, the number of medications taken, and whether they had stayed in a hospital or consulted a general practitioner in the last 2 years. The variables were dichotomized and combined into an objective health index ranging from 0 to 4, where higher values indicate better objective health. Perceived health was measured by the three questions concerning: perceived general health (2 = good, 1 = medium, and 0 = bad), perceived health compared to others of the same age (2 = better, 1 = similar, and 0 = worse), and perceived health-related limitation of desired activities (2 = not at all, 1 = to some extent, and 0 = yes). The variables were summed to form a perceived health scale, with a range of 0 to 6, where higher values indicate better subjective health.
ADL were measured with a more detailed scale than in the after-death proxy interview (described subsequently), including four questions about Instrumental ADL (IADL) such as cleaning their home, shopping, transportation, and cooking, added together to produce a scale with a total score that ranged from 0 to 4, and six Personal ADL (PADL) questions (about bathing, dressing, using the toilet, getting in and out of bed, continence, and eating), with a total score that ranged from 0 to 6. Higher values indicate better performance of ADL. Patterns of received help were measured by coding whether assistance with ADL came from informal sources, formal sources, or both, based upon responses to each of the 10 ADL items.
To assess the social network, the interview with the oldest old individuals included similar questions to those in the proxy interview after the oldest old individual's death (described subsequently) concerning personal and telephone contact with their children and personal contact with relatives. The answer alternatives had a range from: 6 = daily to 0 = never/not relevant for all three items. An index of objective social network was created in a manner similar to that for the proxy interview, with a range of 0 to 18, where higher values indicate more frequent social contact. The in-person interview with the oldest old respondents in the NONA study also included a three-item measure of perceived social network, including feelings of having acquaintances (range: 3 = to a great extent, 0 = not at all), feelings of belonging to a circle of friends (range: 3 = to a great extent, 0 = not at all), and feelings of having confidants (range: 3 = several, 1 = none). The three items were summed to form an index ranging from 0 to 9, where higher values indicate a more positive perception of the social network.
Proxy Interview
The telephone interview with the proxies took place ~1 month after the oldest old individual's death. It was performed by the same trained registered nurses who interviewed the oldest old individuals, or their proxies, before their death.
The proxy interview included questions about the location at the time of death: in the community, at a hospital, or at an eldercare institution (long-term geriatric care, nursing home, similar institutions for patients with dementia, or residential homes for individuals who cannot live in the community). The proxies were asked to estimate the time the elderly had spent at the location where they died, and if it was not in the community, to report where they had lived previously, and for how long. They were also asked to estimate use of formal and informal care in the last year of life and to evaluate the formal care given at the end of life, providing their general opinion about the care and the staff competence and attitudes toward, and treatment of, the old relative.
The proxies were also asked to estimate the health and memory status of the elderly individual 1 year, 6 months, and 1 month before their death (each coded as 3 = good, 2 = medium, and 1 = bad) and to describe the pattern of change in health (rapid deterioration or a more prolonged decline). In addition, they were asked to estimate how the old individual had managed their household (3 = totally independent, 2 = somewhat dependent, and 1 = totally dependent) and personal care (3 = totally independent, 2 = somewhat dependent, and 1 = totally dependent) at these same points in time.
The elderly individuals' social networks were assessed with questions concerning the frequency of contact with children and relatives, similar to the in-person-interview with the oldest old individual but with less detailed answer alternatives: “How often did NN have personal contact with her/his children?” (range: 3 = daily contact, 0 = never/seldom or not relevant), “How often did NN have telephone contact with her/his children?” (range: 3 = daily contact, 0 = never/seldom or not relevant), and “Did NN have contact with other relatives?” (2 = yes, two or more; 1 = yes, one; 0 = no). The interview also included one question concerning whether the children lived nearby. For some analyses, an index was created using the questions about contact with children and relatives, with a total score ranging from 0 to 8, where higher values indicate more social contacts.
Statistical Analyses
The χ2 test, t test, and one-way analysis of variance were used to assess differences in location at time of death (in the community, hospital, or eldercare institutions). Pearson's correlation was used to examine correlations among changes in health, functional ability, and memory during the last year.
In order to validate proxies' answers, they were matched with the oldest old individuals' answers from the last interview in which they had participated (1999, 2001, or 2003). Fifty of the deceased NONA subjects participated only in 1999; another 25 had had their last interview in 2001 and 1 participated on all three occasions (Table 2). Therefore, 76 of the deceased NONA subjects participated in interviews on their own, and 26 participated entirely by proxy, even earlier in the main NONA study. Therefore, the correlation analyses of answers provided by proxies (after the oldest old individuals' deaths), and the elderly themselves, were based on 76 cases.
Table 2. Correlations among proxies' estimates and the old individuals' last response in the NONA study (N = 76)

p < 0.05.
**p < 0.01.
Ethical Considerations
The participants were given written and oral information about the study, stressing the confidentiality and the voluntary nature of participation and they were included if they gave oral consent to participate. The research ethics committee at Linköping University has approved the study (Dnr: 99-078).
RESULTS
Description of the Deceased Elderly Individuals
Most of the elderly individuals were widows or widowers (82) and lived alone at institutions (65). Fourteen were still married at the time of death, but only eight lived with a husband or wife; six lived alone in institutions. Two lived with their children.
Health, Functional Ability, and Memory during the Last Year
As is shown in Table 3, nearly half of the proxies (49) estimated the health of their elderly relative as good 1 year before their death, but only 16 estimated the health as good 1 month before their death. Most of the proxies (75) thought that their relative's health had steadily deteriorated during the last year; six stated that their relative's health had been fluctuating. Eighteen proxies reported that their elderly relative had experienced a sudden death, with no remarkable deterioration in health beforehand. There was a significant difference in the pattern of changes in health before dying, based on location at time of death (χ2 = 10.93, p < 0.05); three of those dying at home died a sudden death, and all six elderly individuals whose health had been reported fluctuating were staying at institutions at the time of death.
Table 3. Estimates from proxies on health and functional ability during the last year of the old individuals' lives

Estimated changes in health correlated significantly with estimated changes in household management by the elderly individual (r = 0.47, p < 0.001) and management of personal care (r = 0.55, p < 0.001). Proxy estimates of the elderly relative's status 1 year, 6 months, and 1 month before death suggests a decline in household management and personal care during the last year of life. The proxies also reported a decrease in memory (Table 3). When asked if the elderly individual experienced dementia or similar symptoms during the last year, nearly half of the proxies (48) confirmed such problems. Significantly more of the elderly who suffered from dementia or similar symptoms died at eldercare institutions (χ2 = 15.54, p < .01).
Social Contacts
According to the proxies, 16 of the elderly had no children; of the 86 who had children, all had at least some children living relatively nearby, none further than 15 kilometers. Most of the elderly had frequent personal contact with their children (daily: 22; several times a week: 39; once a week: 14). Telephone contact was less common (daily: 17; several times a week: 18; once a week: 9; never or seldom: 39). Ten individuals never or seldom met with their children. Most of the elderly individuals had contact with at least one other relative. There was a significant difference in social contacts based on location at time of death (Table 1). Those elderly who died in the community or at a hospital met more frequently with their children and also talked with them on the phone more often; there was no such difference regarding contact with other relatives.
Patterns of Care during the Last Year of Life
Patterns of informal and formal care during the last year are described in Table 4. Many of the elderly lived in institutions during the last year (Figure 1) and therefore naturally received formal care. There was no significant difference in the number of individuals using formal or informal care 1 month versus 1 year before death. Three of the respondents stated that their elderly relative received help from outside the family (informal) or the municipality (formal). Very few of the proxies reported that the elderly received only informal care; most commonly, patients received both informal and formal care.

Fig. 1. Care trajectories at end of life in this sample of the oldest old (N = 102). aFour of them used a combination of both formal and informal care.
Table 4. Estimations of patterns of care. Number of elderly individuals using formal care, informal care or both
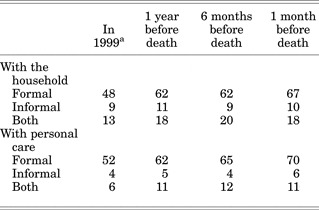
aAccording to interviews at baseline with the old individuals (n = 76) and proxy interviews (n = 26).
Location at Time of Death
Figure 1 illustrates where the elderly died and their care trajectories during the last year of life. Most individuals died at an institution; ~20% died at a hospital (21). Only five died in the community. For those who lived at institutions at the end of life and also died there, the mean length of stay at the institution was ~4 years (range: 2 days to 20 years). Most of the elderly had lived at the institution for >1 year, but five had lived in the institution for <l month. For the 21 individuals who died in a hospital, the duration of stay was ~1 week (range: 0.5 day to 3 weeks). The mean length of the stay was longer for elderly who had been living in the community than for institutionalized individuals, none of whom stayed at hospital for >10 days. For the seven elderly individuals who had lived in institutions before they came to the hospital and died there, the mean stay at the institution was ~2 years; however two individuals had lived in their institution for <3 weeks (Figure 1).
Estimations of the End-of-life Care
The proxies for the elderly who died at a hospital rated the hospital care as good (18) or fairly good (3). They rated the competence of the staff as very good (10), good (6), or fairly good (2). Their ratings of staff attitudes and treatment at the hospital were also high: very good (11), good (6), or fairly good (1). None of the proxies rated staff competence or treatment as bad, but three did not answer the questions.
Eighty-three elderly were living at an eldercare institution at the end of life. Most of their proxies rated the competence of the institutional staff as good (28) or very good (27); 12 rated the competence as medium, and 5 rated it as bad. They also rated the quality of treatment in the institution as high (very good, 37; good, 29; medium, 5; bad, 2). Some proxies (11 about the competence and 10 about the treatment) did not answer the questions.
As was demonstrated earlier, 19 of the oldest old in this sample were living in the community at the end of life, five of them died there, and 14 died at a hospital. Of these 19, four received help from the Home Help Services, three used both Home Help Services and Home Health Care, and four used Home Health Care only. Proxies rated the competence and treatment of the staff from the Home Help Services as very good (2), fairly good (2), and medium (2). They rated the competence of and treatment by the staff from the Home Health Care as very good (2), good (2), medium (1), and bad (1). One proxy could not make an evaluation.
All of the proxies were also asked if the elderly had received the care they needed. These questions were posed to all of the proxies, no matter where their relative had died, as many of the old individuals received care both in the community, at a hospital, and/or at an institution during their last year.
As is shown in Table 5, most proxies thought that the elderly received the care they needed. There were no significant differences in satisfaction with the care for elderly who died at a hospital, eldercare institution, or at home. All proxies were also asked about complications such as pain and pressure ulcers. None of the elderly who died at home were reported to have had pain problems or pressure ulcers. Thirteen of those 21 who died at a hospital were reported to have had problems with pain, but the proxies also reported that they received the pain relief they needed. Among those who died at institutions, 47 suffered from pain, and 46 received the pain relief they needed. Seventeen of those who died at an elder care institution and three of those who died at a hospital had pressure ulcers.
Table 5. Proxies' estimation of whether the old individual got necessary care at the end-of-life

The proxies were also asked how they were treated by the staff as relatives to the old individual. Most of them felt that they were treated well (85) or rather well (8). Two proxies thought that they had been treated poorly; both of them had elderly relatives who died at an eldercare institution. Six of the proxies would not answer the question, because they had had little contact with the staff.
DISCUSSION
Gerontological research has identified several factors that in a long or medium time perspective are associated with mortality or survival, including health, ADL, and social networks. Nevertheless, surprisingly few studies have focused on these factors during the end of life. Perhaps even more surprising is that few studies have focused on end-of-life care of the oldest old, a group of individuals with special needs and, often, special living conditions. Therefore, the results of this study contribute important knowledge, and it also highlights the challenge of end-of-life care for this group. There is a need for more research in this field.
Similar to others studies (Anderson et al., 1999; National Board of Welfare, 2005), most of this sample of the oldest old died at some kind of institution, despite the stay-in-place policy that exists in Sweden. However, the definition of end-of-life care could be challenged. For those elderly who died a sudden death, hospital care was end-of-life care, even if it only lasted for one day. The intention of the “stay-in-place-policy” is to avoid moves at end of life, and provide as good care as possible at the place of residence of the oldest old individual. The idea is that the elderly individual might feel more comfortable with such an arrangement. Although few elderly move to an institution or hospital shortly before their death, the necessity of some moves could be questioned.
End-of-life care is closely related to a country's economic, social, and cultural environment. It is therefore important to acknowledge that the present study was conducted in a relatively affluent welfare society. In Sweden, both eldercare at institutions and home help services provided in the community are subsidized and run by municipal or regional authorities; there are few other options for the elderly to choose from. However, end-of-life care, whether it is medically advanced or not, does not cause any economic problem for the family. Therefore, this study could be seen as an example of care flows free from economic considerations from the family point of view.
Our finding that the proxies seemed to be satisfied with the end-of-life care, regardless of where it was provided, is promising. For example, nearly all of the elderly who experienced pain received adequate pain relief, according to the proxies. However, problems with pain and pressure ulcers were more frequent among those elderly who died at an institution. This could be interpreted as a sign of maltreatment, but as pressure ulcers and pain often indicate severe illness, it could simply be indicative that the elderly who were in very poor health moved to institutions because they had an increased need for care.
Catt et al. (Reference Catt, Blanchard and Addington-Hall2005) found that when elderly were asked about where they would prefer to die, they preferred a hospital to home, and both young and old individuals preferred a hospice to home. As was mentioned earlier, a majority of our sample died at some kind of eldercare institution, and not at a hospital or a hospice. However, elderly are less likely to be referred to palliative care (Ahmed et al., Reference Ahmed, Bestall and Ahmedzai2004; Kessler et al., Reference Kessler, Peters and Lee2005). One explanation for this could be that the end-of-life period among the oldest old tends to be a prolonged period of co-morbidity, and it is hard to predict the duration of the care. Our results demonstrate that most proxies estimated that the health of the elderly had steadily deteriorated during the last year, or had fluctuated, which is similar to results presented by Rinell Hermansson (Reference Rinell Hermansson1990). Moreover, according to the proxies in our study, nearly half of the oldest old individuals suffered from dementia or similar symptoms. Much palliative care or hospice care is focused on special conditions or diagnoses such as cancer. The population of the oldest old, as in our sample, with prolonged dying, chronic illnesses (especially dementia), and co-morbidity, are probably difficult to accommodate within the palliative care model. This idea is supported by a study by Covinsky et al. (Reference Covinsky, Eng and Lui2003b) who concluded that end-of-life care targeting individuals with problems clearly suggestive of impending death (such as hospice care) is poorly suited to elderly dying people with progressive frailty. However, both Hallberg (Reference Hallberg2006) and Raymond and Woo (Reference Raymond and Woo2001) suggest that palliative care may be appropriate for long-term care of very old people, but that care provided to older people at the very end of life needs adjustment. For example, end-of-life care for the oldest old should consider the importance of the social network and the special needs caused by co-morbidity and reduced biological reserve capacity, which affect health and symptoms.
According to proxies in our study, end-of-life care was satisfactory, and most elderly individuals died where they wanted to. Most proxies also rated the quality of treatment and competence of the staff as high. However, one cannot ignore the possibility that these very positive ratings are some kind of defence mechanism. It is comforting to tell oneself that a relative was well taken care of. Also, the relatives (proxies) might have had lower standards and did not expect anything else, because their relatives were very old. Rinell Hermansson (Reference Rinell Hermansson1990) reported that relatives of older deceased patients were more satisfied with the circumstances of their death than were the relatives of younger deceased patients. Considering the special needs of the oldest old individuals, posed by co-morbidity and prolonged need of care, in Sweden today, eldercare institutions probably offer the most suitable care, and institutional care staff are probably the most competent in this regard.
An elderly person's social network affects the last year of life. In this sample, it seemed that most of the elderly had a good social network. Those who died at institutions had, however, less contact with their children than did those who died at home or at a hospital, similar to previous research. A possible explanation for this finding is that the elderly who are disabled but still live in the community, might receive more informal assistance, resulting in a higher frequency of contact with family, relatives, and friends, as suggested by Bertera (Reference Bertera2003) and Hyduk (Reference Hyduk1996). Previous analysis of the NONA sample showed that the elderly individuals living in the community received more informal care and therefore had additional opportunity to meet with their children and relatives. When the elderly individuals moved to institutions, informal care was replaced by formal care, which could account for the reduced number of in-person contacts from the informal network. Another possibility is that low levels of function are associated with low levels of social activity and few social contacts (Litwin, Reference Litwin2003; Stuck et al., Reference Stuck, Walthert and Nikolaus1999). Those elderly who moved to an institution and died there probably had worse conditions, severe problems with ADL, and in many cases dementia, as already mentioned. Whatever the reason are for changes in the social network, it is important to take the results seriously. Ringdal et al. (Reference Ringdal, Ringdal and JordhØy2007) found that in cancer patients social support might buffer against reactions to stressful events, such as terminal cancer. This result might also be applicable for the oldest old individuals, at end of life, as they probably have thought about death and dying.
Previous research has shown that there is a tendency to perceive the elderly as more accepting of death and less in need of support, but in fact they have the same thoughts as any person at any age (Ahmed et al., Reference Ahmed, Bestall and Ahmedzai2004; Hallberg, Reference Hallberg2006). Liptzin (Reference Liptzin2006) further suggests that aging confronts the older individual with death of friends and family, which allows them to anticipate and prepare for their own death. In this preparation, the social network that is left is probably of great importance. Our findings demonstrate that the proxies' estimates of social contacts were related to not only their relatives' objective estimates of their social network, but also to their more subjective ratings of belonging to a circle of friends and having confidantes. It is understandable that if the institutionalized elderly individuals are very ill and/or disabled, it might affect the frequency of social contact, and also probably the sense of having friends and acquaintances. Nevertheless, it is a sad fact that when you are approaching death, at the time when you most need a friend to talk to, they are fewer. This highlights the important challenge to increasing the involvement of relatives in the care of the oldest old.
In conclusion, most of the elderly in this study of the oldest old died at an institution and the relatives were mostly satisfied with the end-of-life care. The palliative care that they received was part of the ordinary care within the eldercare organization. Health decreased steadily during the last year of life, and there was a decline in the ability to perform daily life activities.
However, the eldercare system seems to have been able to meet the increasing demands during the last time of life of the oldest old.
ACKNOWLEDGMENTS
This study has been supported by the Swedish Council for Working Life and Social Research, the Swedish Council for Social Research, and the Vardal Foundation for Health Care and Allergy Research.








