Neurodevelopmental delay has been described in children with critical CHD. Neurological and radiological research resultsReference Brosig, Mussatto and Hoffmann1–Reference Rychik7 show that neonates with hypoplastic left heart syndrome carry an abnormal cerebral microstructure, and their intrauterine brain growth may be delayed. Postnatal treatment of hypoplastic left heart syndrome includes extensive cardiac surgery in the neonatal period using cardiopulmonary bypass often followed by long intensive care stays with haemodynamic instabilities.Reference Hoffmann, Brosig, Mussatto, Tweddell and Ghanayem8–Reference Tabbutt, Nord and Jarvik10 Later, these children undergo at least two further cardiac bypass surgeries (bi-directional Glenn and Fontan operation).Reference Brosig, Mussatto and Hoffmann11–Reference Gaynor, Ittenbach and Gerdes13 Whether neurodevelopmental problems are caused primarily by prenatal or postnatal factors is still unclear. On this basis, a poor quality of life and low social integration could be presumed. Many of these patients with hypoplastic left heart syndrome have now reached school age. Children born with CHDs who have had several surgical interventions and numerous hospital stays have experienced very difficult challenges – some as a result of overly lenient (inconsistent) parenting, and others due to excessive demands by their day-to-day educational environment (cognitive and/or social challenges), and others again as a result of dealing with the frustrations of having to interact with healthy peers of the same age.Reference Fteropoulli, Stygall, Cullen, Deanfield and Newman14–Reference Ferry19 Furthermore, these patients are at risk for thromboembolic events including cerebral infarction both before and after completion of a Fontan circulation. These patients may be particularly vulnerable as a result of the technically difficult first-stage Norwood procedures. Finally, altered cerebral blood flow in utero in hypoplastic left heart syndrome-fetuses and a postnatal reduced head circumference have been shown to potentially affect neurodevelopmental outcome.Reference Donfrio, Bremer and Schieken20,Reference Kaltmann, Di, Tian and Rychik21 Single-centre neurocognitive follow-up studies report these patients to have normal intelligence quotient scores.Reference Oberhuber, Huemer, Mair, Sames-Dolzer, Kreuzer and Tulzer22–Reference Wernovsky25 Nevertheless, in several centres around the world, comfort care is still offered to parents of newborn with hypoplastic left heart syndrome or, if diagnosed prenatally, abortion because of an expected unfavourable outcome. In these centres, it is still an ethical question if children with this diagnosis should undergo complex cardiac surgery having the prognosis only to suffer.
Therefore, especially for prenatal counselling, information on quality of life of patients with hypoplastic left heart syndrome is important to help couples make well-informed decisions about their pregnancy.
Thus, the aim of this study was to
- survey the assessments of quality of life from the patients’ view and the viewpoint of their parents;
- survey the quality of life scores (total, physical, mental, emotional, social, academic) in comparison with healthy children, and
- survey children with other heart diseases (mild, moderate, and severe heart defects, heart defects in total).
Over the past decades, the concept of quality of life has been of paramount importance for evaluating the quality and outcome of health care.Reference Moons, Budts and De Geest26 The first study on quality of life in patients with CHD was published more than 40 years ago.Reference Bratt and Moons27 It is known that quality of life is a complex construct with no uniform definition which causes a conceptual haziness, and quality of life research has been criticised for a lack of conceptual clarity and clear definition of quality of life. This may result in inaccurate measurements of “true” quality of life and in inconclusive study findings. To direct more attention to this phenomenon, Gill and FeinsteinReference Gill and Feinstein28 evaluated the quality of existing quality of life research. On the basis of the Gill and Feinstein criteria and the findings in previous reviews,Reference Moons, Budts and De Geest26,Reference Bratt and Moons27,Reference Haraldstad, Wahl and Andenaes29 there are proposals for recommendations for quality of life.
Therefore, we used a very clear research design by comparing our results with well-defined studies and a valid, reliable, and objective measurement as it will be mentioned.
Knowledge about quality of life is important for understanding the consequences of illness and treatment and for medical decision making across age groups and culture. Quality of life is an important endpoint in medical and health research, and quality of life research involves a variety of target groups and research designs. The term health-related quality of life is described as referring to the health aspects of quality of life (and is used as a scale unit in Varnis Pediatric Quality of Life), generally considered to reflect the impact of disease and treatment on disability and daily functioning; it has been considered to reflect the impact of perceived health on an individual’s ability to live a fulfilling live. However, more specifically, health-related quality of life is a measure of the value assigned to duration of life as modified by impairments, functional states, perceptions, and opportunities, as influenced by disease, injury, treatment, and policy.Reference Gill and Feinstein28
Material and methods
Patients
From 1997 to 2009, 149 children (n = 149) with hypoplastic left heart syndrome were admitted to the Children’s Heart Center Linz. Sixty-four patients died before entering school. Of these, 25 newborns died before surgical treatment due to circulatory collapse or because the parents chose comfort care. All other patients (n = 124) underwent a Norwood Stage I operation in the newborn period, a bi-directional Glenn at the age of 3–4 months, and a Fontan operation around the age of 3 years, all at our institution. About 39 children (31%) died before entering school; 24 between stage 1 and 2; 14 children died after bi-directional Glenn surgery between stages 2 and 3; and 1 child died after Fontan operation; of the remaining 85 patients, 42 patients did not participate in the study: 33 children whose parents denied informed consent (without giving reasons, mean age 10.2 ± 3.14 years; range: 7.5–16.5 years, 12 male, 21 female), 1 boy with severe hypoxic encephalopathy after the Fontan procedure, and 11 children from non-German-speaking foreign countries. Thus, 41 patients (mean age 10.3 ± 3.16 years; range: 6.3–16.9 years) and 44 parents underwent tests and questioning for our empirical research. We obtained complete results for 41 patients and 44 parentsReference Lambert, Minich and Newburger30 (see Figure 1).
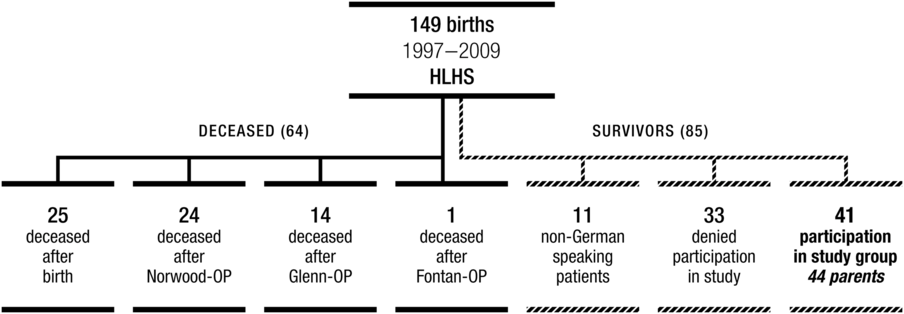
Figure 1. Sample, hypoplastic left heart syndrome 1997–2009.
Twenty-one children had been diagnosed prenatally; 26 were male; 33 had received a Sano-shunt at the time of the Norwood operation and 8 had a modified Blalock-Taussig shunt; 26 patients had aortic atresia; 15 had aortic stenosis; 5 were operated in deep hypothermic circulatory arrest; 9 patients were operated using antegrade cerebral perfusion, and 27 patients underwent double perfusion technique.
There were no data in the investigated group concerning morphological changes of the brain, no sonographic or MRI examinations which could be related to the results. Patients with hypoplastic left heart syndrome who participated in the study attended the following school types: primary school (n = 20), secondary school (n = 8), academic secondary school (n = 2), special needs school (n = 4), secondary school with a business emphasis (n = 2), apprenticeship (n = 1), Montessori or Freinet school (n = 2), and unemployed after compulsory schooling (n = 2).
Three patients were diagnosed with attention-deficit hyperactivity disorder, 2 with protein-losing enteropathy, 8 with sensorimotor disorders (such as problems with coordination of sensory and motor signals while writing, holding crayon; spatial orientation deficits, etc.), 2 with seizures, and 1 with autism (see Table 1).
Table 1. Sample description

HLHS = hypoplastic left heart syndrome
This study was approved by the local IRB (ID-number J16-01).
Pediatric quality of life inventory
Health-related quality of life is defined as the impact of a specific illness, medical therapy, or health services policy on a patient’s ability to function in various life contexts and draw personal satisfaction from physical, psychological, and social functioning perspectives.Reference Mellion, Uzark and Cassedy31,Reference Drotar32 The Pediatric Quality of Life Inventory Version 4.0 Generic Core Scales (PedsQL) is a reliable, valid generic health-related quality of life measurement tool that is widely used in paediatric populations to determine health-related quality of life in patients with chronic disease and healthy controls.Reference Varni, Burwinkle, Seid and Skarr33 The Pediatric Quality of Life Inventory can be used to characterise the impact of therapies and disease processes on the health-related quality of life of children and adolescents with CHD and to compare impacts with those in children and adolescents with other chronic diseases. Using the Pediatric Quality of Life Inventory, children self-reports, and parent reports from Varni,Reference Varni, Limbers and Burwinkle34 a health-related quality of life measurement by means of patient self-assessments and parent assessments was used to obtain patients’ quality of life ratings for physical, social, emotional, and school areas. The questionnaire comprised 23 items that contribute to four subscales: physical, emotional, social, and school functioning. Maximum score is 100, and minimum score is 0. The three latter subscales can be combined as psychosocial functioning. The questionnaire was translated into German according to the guidelinesReference Varni, Limbers and Burwinkle34 and approved by the authors of the questionnaire. The Pediatric Quality of Life Inventory scales are composed of parallel child self-report and parent proxy-report formats, and the wording and content are as similar as possible across formats. The reliability and validity of the Pediatric Quality of Life Inventory generic core scales have been demonstrated in healthy and patient populations and their parents.Reference Mellion, Uzark and Cassedy31,Reference Varni, Seid and Kurtin35 HaraldstadReference Haraldstad, Wahl and Andenaes29 showed in a systemic review of quality of life research in medicine and health science that the Pediatric Quality of Life Inventory was used most frequently as an instrument to measure health-related quality of life. We used the cardiac module by Varni.Reference Varni, Limbers and Burwinkle34
Comparison
The health-related quality of life scores of patients with hypoplastic left heart syndrome as well as parent assessments were compared with Pediatric Quality of Life Inventory results of the general population of primary school children according to the 2008 Felder-Puig studyReference Felder-Puig, Baumgartner, Topf, Gadner and Formann36 and to the results of a comprehensive survey conducted by Mellion (healthy sample and samples with different heart diseases, mild defects, CHD 1, biventricular heart defects, CHD 2, and single ventricle, CHD 3).Reference Mellion, Uzark and Cassedy31 Both studies used the same questionnaire and investigated comparable samples with healthy children from Austria and healthy children and healthy adolescents and children and adolescents with different heart diseases all over the world. Our sample was divided into a children group, n = 28, 6–12 years, and an adolescent group, n = 13, 13–16 years.
A study by Felder-Puig et al
In total, 1412 children from Austrian public schools (age 8–12 years) and 1185 parents completed child- and parent-versions of the Pediatric Quality of Life Inventory. These children demonstrated a good health-related quality of life. About 15% of children showed a notably low health-related quality of life, 47% of parents had higher school education, 85% were Austrian citizens, and 54% had a good to very good household income. Their Pediatric Quality of Life Inventory scores were similar to those of children from other developed countries (Cincinnati Urban Area, United States of America, n = 525 children aged 6–13 years; South Wales, Great Britain, n = 1033 children aged 8–18 years; 3 urban and 2 rural areas in Norway, n = 419 adolescents aged 13–15 years; San Diego school district, United States of America, n = 2435 children aged 8–18 years; State of Victoria, Australia, n = 1456 children aged 9–12 years).Reference Felder-Puig, Baumgartner, Topf, Gadner and Formann36
A comprehensive survey conducted by Mellion et al
Pediatric clinics in Cincinnati, Philadelphia, Boston, Dallas, Waco, Milwaukee, Phoenix: Healthy probands (healthy children: n = 445, youth: n = 202), patients with mild heart defects (CHD mild, septal defects, pulmonary venous anomaly, right heart lesions, left heart lesions, children: n = 99, youths: n = 94), patients with biventricle heart defects (CHD bi-ventricular, children: n = 371, youths: n = 333), patients with single ventricle (CHD single ventricle, children: n = 123, youths: n = 72), all heart defects combined (CHD composite, children: n = 593, youths: n = 499) were compared with the results of children (6–12 years, n = 27) and youth (13–16 years, n = 13) from our normative sample of hypoplastic left heart syndrome patients. By means of a 95% confidence interval, the d-value was calculated to show a given or non-given significance between the respective groups.Reference Mellion, Uzark and Cassedy31
Performed data collection
The psychological assessments for children living at some distance from the Children’s Heart Center in Linz were combined with medical check-up appointments and took place between November 2014 and April 2015. (Psychological care is a part of the holistic concept in our Children’s Heart Center since families of a child with CHD know about the heart problem. Children with CHD who come to the medical check-up are invited to undergo and follow psychological counselling and were asked to participate in the study.)
The parents were notified of the results in May 2015.
Statistical analysis
The data are presented as mean ± standard deviation. For comparison of the Pediatric Quality of Life Inventory scores of the hypoplastic left heart syndrome group with published Pediatric Quality of Life Inventory scores of healthy children and children with other chronic diseases, Hedges’ g (bias-corrected) and its 95% confidence interval were calculated.Reference Kline37 Group differences are considered statistically significant if the 95% confidence interval does not include 0.
Results
Health-related quality of life: patients and parents, descriptive statistics
The results for 41 children with hypoplastic left heart syndrome aged 6.3–16.9 years showed self-assessments of health-related quality of life on a scale from 0 to 100 ranging from a minimum of 5.00 (social functioning) to 100 (physical health-related summary score, emotional functioning, social functioning, school functioning), with 98.44 as a total score (74.64 ± 15.17). The parents’ assessments (proxy) were quite similar, showing a range from 10 (social functioning) up to 100 (72.38 ± 16.57) (see Table 2).
Table 2. Descriptive Statistics: Health-Related Quality of Life Score/patients (n = 41, n = 40) and parents (n = 44)

HSS = health summary score
Twenty-one patients had a prenatal diagnosis and 22 were diagnosed after birth. However, there was no significant difference in all health-related scores between both groups. Also, we did not find any significant difference between shunt types and perfusion techniques at the time of the Norwood operation, hypoplastic left heart syndrome anatomy, gender, and types of school.
Pediatric Quality of Life Inventory results compared with the 2014 Mellion analysis and the 2008 Felder-Puig study
Healthy children from both studies (Mellion, Felder-Puig) aged 6–12 years showed, in their self-assessments as well as in assessments by their parents, significantly higher health-related quality of life scores in all parameters (total score, physical HSS, psychosocial health summary score, social functioning, school functioning) than the hypoplastic left heart syndrome probands except for in emotional functioning, where a small difference was noted, g = −0.34 (see Table 3).Reference Mellion, Uzark and Cassedy31,Reference Felder-Puig, Baumgartner, Topf, Gadner and Formann36
Table 3. PedsQL-Scores – HLHS-Children versus Healthy Samples

CI = confidence interval; ES = effect size (hedges g); HLHS = hypoplastic left heart syndrome; HSS = health summary score; PedsQL = Pediatric Quality of Life Inventory
Self-assessments by adolescents (ages 13–16 years), compared to the Mellion study, showed, in their self-assessments as well as in assessments by their parents, marginal significant differences (g = 0.5 ≤ 0.8) between healthy youths and hypoplastic left heart syndrome adolescent patients, except in emotional functioning: g = −0.105 (see Table 4).
Table 4. PedsQL-Scores – HLHS-Adolescents versus Healthy Sample

CI = confidence interval; ES = effect size (hedges g); HLHS = hypoplastic left heart syndrome; HSS = health summary score; PedsQL = Pediatric Quality of Life Inventory
Children with less severe heart defects (CHD Mild) gave themselves higher health-related quality of life scores (without emotional and school functioning) than children with hypoplastic left heart syndrome from our sample as well in assessments by their parents (see Table 5).
Table 5. PedsQL-Scores – HLHS-Children versus Chronic Heart Disease
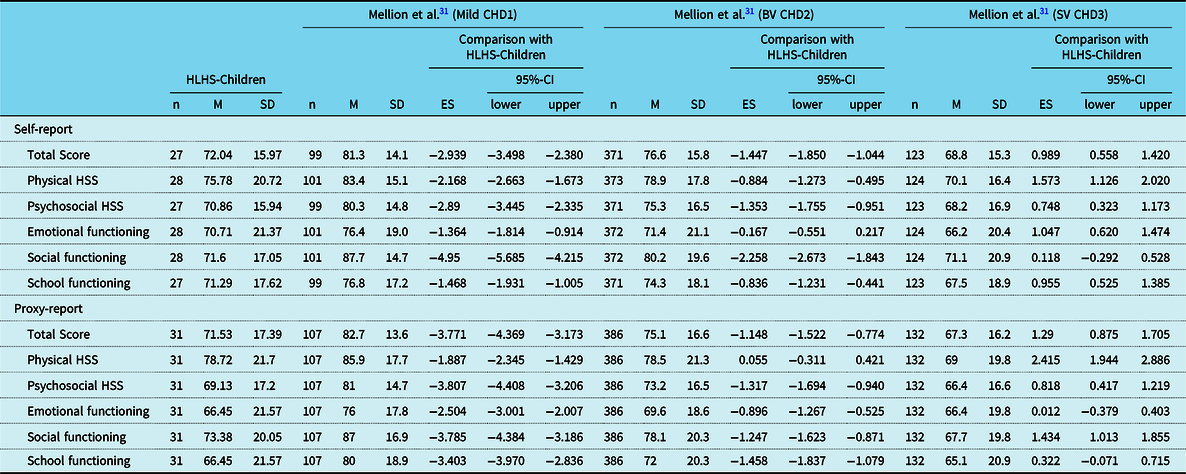
CI = confidence interval; ES = effect size (hedges g); BV = biventricular; SV = single ventricle; HLHS = hypoplastic left heart syndrome; HSS = health summary score; PedsQL = Pediatric Quality of Life Inventory
There were no significant differences between our sample and children with biventricular CHD and children with single ventricle defects. A tendency was observed that children with hypoplastic left heart syndrome from our sample and their parents gave higher scores than patients with CHD with single ventricle physiology from the Mellion study, but without significance (see Table 5).
Comparing our hypoplastic left heart syndrome adolescent sample (n = 13) with the different heart defect groups (CHD 1, CHD 2, and CHD 3) by Mellion, there was no significant difference to be seen. However, again there was a tendency that patients with hypoplastic left heart syndrome and their parents showed higher health-related quality of life scores than adolescents with single ventricle defects (CHD 3) (see Table 6).
Table 6. PedsQL-Scores – HLHS-Adolescents versus Chronic Heart Disease

CI = confidence interval; ES = effect size (hedges g); BV = biventricular; SV = single ventricle; HLHS = hypoplastic left heart syndrome; HSS = health summary score; PedsQL = Pediatric Quality of Life Inventory
Compared to youths with single ventricle (86.3 ± 14.34), youths with hypoplastic left heart syndrome rated themselves significantly higher in the physical area (physical HSS), g = 0.723 (see Table 6).
Discussion
Several studies have explored quality of life (not health-related quality of life!) of Fontan patients. Some reported normal quality of lifeReference Pike, Evangelista, Doering, Eastwood, Lewis and Child38,Reference d’Udekem, Cheung and Setyapranata39 and others reduced quality of life.Reference Marino, Sher and Wernovsky40,Reference McCrindle, Williams and Mitchell41 However, differences in patient age and in quality of life assessment instruments being employed together with quality of life being a highly subjective matter and differing among individuals make the comparison between studies difficult.
In general, findings from quality of life research in CHD have been inconsistent.Reference Drotar32,Reference Latal, Helficht, Fischer, Bauersfeld and Landolt42 This may, in part, not only be due to methodological issues such as small sample sizes, use of proxy reports, and variable assessments of quality of life, but may also reflect the fact that psychological responses to the stress of chronic illness are highly individualised and influenced by many factors such as personal perceptions, expectations, presence of functional limitations, cognitive delay, and comorbid conditions. Severity of disease is not a reliable predictor of quality of life.Reference Moons, Van, Budts and De43
Advances in diagnosis, medical management, and surgical intervention have improved the longevity and quality of life for children with CHD. Despite this, there are few research studies specifically examining the psychosocial concerns of adolescents and young adults with CHD. For the purpose of exploring the subjective experiences and dilemmas of this population during the transition from adolescence to young adulthood, nine adolescents and young adults were interviewed by Tong et alReference Tong, Sparacino, Messias and Foote44 using a semi-structured protocol. An understanding of these experiences by health professionals can be beneficial in helping this clinical population as they grow up and face the challenges of an uncertain yet promising future.
Children with CHD requiring open-heart surgery are a group at high risk for health-related sequelae. Little consensus exists regarding their long-term psychological adjustment and health-related quality of life. Thus, Latal et alReference Latal, Helficht, Fischer, Bauersfeld and Landolt42 conducted a systematic review to determine the current knowledge on long-term outcomes in this population. Randomised controlled trials, case–control, and cohort studies published between 1990 and 2008 evaluating self- and proxy-reported psychological adjustment in patients aged between 2 and 17 years with follow-ups of at least 2 years after open heart surgery for CHD were included. A significant proportion of survivors of open-heart surgery for CHDs are at risk for psychological maladjustment and impaired quality of life. Future research needs to focus on self-reports, quality of life data, and adolescence.Reference Latal, Helficht, Fischer, Bauersfeld and Landolt42
It was shown that a worse medical history and worse present medical status did not only predict worse physical parent-reported and self-reported health-related quality of life but also worse psychosocial health-related quality of life and subjective cognitive functioning.Reference Dulfer, Bossers, Utens and Duppen45
The results of this study showed that the spectrum of self-assessments and external evaluations by parents with regard to the health-related quality of life of hypoplastic left heart syndrome survivors (ages 6 through 16) is very broad. These data show that several children from our sample have developed quite a high quality of life; on the other hand, there are some children who rate their own quality of life as rather low, or their quality of life is assessed as rather low by others. Thus, the necessity for providing extra support to hypoplastic left heart syndrome patients may be considered an additional psychological and educational result of this study.
Looking into more detail, it was interesting to note that:
Patients with hypoplastic left heart syndrome with high health-related quality of life scores in physical areas also assessed psychosocial areas as high. Equally, high values given by the children corresponded to high values given by their parents. There were no significant differences between patient self-assessments and parents’ assessments. When stabilisation of physical areas is achieved in the life of an hypoplastic left heart patient, psychosocial areas become stabilised as well. When hypoplastic left heart syndrome patients have developed a high quality of life, they are able to adequately deal with the challenges that severe heart defects and their accompanying medical and surgical interventions involve. This is reflected in high scores of psychosocial quality of life. The fact that physical stability and the promotion of cognitive skills are the basis for psychosocial quality of life for patients with hypoplastic left heart syndrome was shown by Oberhuber et al.Reference Oberhuber, Huemer, Mair, Sames-Dolzer, Kreuzer and Tulzer22
Our survey shows that the children from our normative sample attend a broad spectrum of schools within the Austrian educational system. The quality of life scores show no significant correspondence with the school type. In description, it can be noted that youths with hypoplastic left heart syndrome who are attending a college of higher vocational education recorded the highest quality of life scores (97.5) in the Pediatric Quality of Life Inventory level, whereas children with special education needs recorded the lowest (48.86).
The comparison of health-related quality of life scores from hypoplastic left heart syndrome patients and parents’ assessments with the Pediatric Quality of Life Inventory results from children and their parents from the Austrian Felder-Puig-studyReference Felder-Puig, Baumgartner, Topf, Gadner and Formann36 and children and youths and their parents who were taken from the comprehensive survey by Mellion et alReference Mellion, Uzark and Cassedy31 showed significantly higher health-related quality of life scores for all parameters (total score, physical health summary score, psychosocial health summary score, emotional functioning, social functioning, school functioning) than the hypoplastic left heart syndrome probands in healthy children (6–12 years) and in children with mild heart defects (CHD Mild), based on self-assessment and parents’ assessments. But adolescent hypoplastic left heart syndrome patients (13–16 years) showed no significant differences compared to all other comparison groups except for in the social area; this finding suggests that they learnt to cope with a severe heart defect; however, this did not hold true for the parents’ assessment as compared to the group of healthy youths.
Limitations and strengths
The major limitation of this study is the small sample size. Several parameters might become significant with larger patient numbers, which can only be achieved by multicentre studies. One strength of this study, however, is that all patients were treated at the same centre and that all stage I Norwood procedures were performed by one single surgeon (RM). Another limitation is the retrospective analysis of the anatomy and the clinic course which involved at least three surgeries. Further alternatives of analysis (multivariate methods) are limited due to the small sample. Possible covariates could not be monitored. It is well known that patients with serious diseases can reach a high quality of life by increasing resilience and coping strategies. It is new that adolescent patients with hypoplastic left heart syndrome treated by one surgical team can get similar health-related quality of life scores as healthy adolescents.
Conclusion
From a psychological viewpoint, these data suggest that a substantial number of patients with hypoplastic left heart syndrome have developed a high level of quality of life behaviour and have improved markedly in dealing with the challenges of living with a life-threatening heart defect. High quality of life may be possible for patients with hypoplastic left heart syndrome in physical and psychosocial areas. Pedagogic and educational assistance and support systems can build on first-class medical treatment; children with hypoplastic left heart syndrome and their families can receive support in successfully coping with life and in achieving the full potential of children and adolescents with hypoplastic left heart syndrome. The finding that adolescent patients with hypoplastic left heart syndrome estimated themselves similar to healthy adolescents suggests that they learnt to cope with a severe heart defect.
Authors’ Contributions
R.D.O. developed the research protocol, collected and analysed the data, and is the main author of this manuscript.
S.H. tested all patients and parents.
R.M., E.S.-D., and M.K. are the heart surgeons and supervised the development of the research protocol, interpretation of the results, and writing of the manuscript.
G.T. was primarily responsible for the study. He supervised the development of the research protocol, data analysis and interpretation of the results, and writing of the manuscript. R.O. and G.T. had full access to the data. They take responsibility for the integrity of the data and the accuracy of the data analysis. All authors read and approved the final manuscript.
Acknowledgements
The authors thank Judith Hansen for translation and Christoph Weber for providing statistical support.
Financial Support
This research received no specific grant from any funding agency, commercial, or not-for-profit sectors.
Conflicts of Interest
None.
Ethical Standards
The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national guideline on human experimentation – IRB (ID-number J16-01), ethical review committee, Kepler University Hospital – and have been approved by the institutional committee.
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and /or national research committee and with the 1975 Declaration of Helsinki, as revised in 2008, and its later amendments or comparable ethical standards.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Perspectives/Translational Outlook
The children with hypoplastic left heart syndrome can accomplish successful school careers, and by means of appropriate tutoring and individual development of resilient personality, they can tap a high quality of life.
Commentary
The data of this paper were recently presented as a poster at the 53rd Annual Meeting of the Association for European Pediatric and Congenital Cardiology in May 2019, which was awarded as a finalist of the poster price competition.









