Introduction
Suicide is a major public health concern worldwide and the second most common cause of death amongst young adults in the European Union (WHO, 2001). Suicide attempt is the strongest known risk factor for suicide (Leon et al. Reference Leon, Friedman, Sweeney, Brown and Mann1990; Yoshimasu et al. Reference Yoshimasu, Kiyohara and Miyashita2008).
For effective prevention, knowledge of key risk factors for suicide attempt and completed suicide is essential. The epidemiology is complex and a range of factors, including childhood risk factors (Sourander et al. Reference Sourander, Klomek, Niemela, Haavisto, Gyllenberg, Helenius, Sillanmaki, Ristkari, Kumpulainen, Tamminen, Moilanen, Piha, Almqvist and Gould2009; Bruffaerts et al. Reference Bruffaerts, Demyttenaere, Borges, Haro, Chiu, Hwang, Karam, Kessler, Sampson, Alonso, Andrade, Angermeyer, Benjet, Bromet, de Girolamo, de Graaf, Florescu, Gureje, Horiguchi, Hu, Kovess, Levinson, Posada-Villa, Sagar, Scott, Tsang, Vassilev, Williams and Nock2010; Niederkrotenthaler et al. Reference Niederkrotenthaler, Floderus, Alexanderson, Rasmussen and Mittendorfer-Rutz2012), familial clustering (Tidemalm et al. Reference Tidemalm, Runeson, Waern, Frisell, Carlström, Lichtenstein and Langström2011), low intelligence quotient (Batty et al. Reference Batty, Whitley, Deary, Gale, Tynelius and Rasmussen2010a ; Sörberg et al. Reference Sörberg, Allebeck, Melin, Gunnell and Hemmingsson2013), low body mass index (BMI) (Batty et al. Reference Batty, Whitley, Kivimaki, Tynelius and Rasmussen2010b ; Kinoshita et al. Reference Kinoshita, Kinoshita, Shimodera, Nishida, Inoue, Watanabe, Oshima, Akechi, Sasaki, Inoue, Furukawa and Okazaki2012), short stature (Jiang et al. Reference Jiang, Rasmussen and Wasserman1999; Whitley et al. Reference Whitley, Rasmussen, Tynelius and Batty2010), low socio-economic status (Andres et al. Reference Andres, Collings and Qin2010), history of psychiatric disorders (Qin, Reference Qin2011) and somatic illness (Gradus et al. Reference Gradus, Qin, Lincoln, Miller, Lawler, Sorensen and Lash2010; Saitta et al. Reference Saitta, Keehan, Yousif, Way, Grekin and Brancaccio2011; Kendal & Kendal, Reference Kendal and Kendal2012), are associated with increased risk.
There are a few cross-sectional studies that indicate physical activity in adolescence as a protective factor against suicidal ideation (Brown & Blanton, Reference Brown and Blanton2002; Babiss & Gangwisch, Reference Babiss and Gangwisch2009), but the relationship with more serious forms of suicidal behaviour (suicide attempt or suicide death) remains unclear. Previous studies have relied on questionnaires or self-rating scales for the measurement of physical activity. Prospective studies are lacking. Cognitive performance (Gunnell et al. Reference Gunnell, Magnusson and Rasmussen2005), BMI (Magnusson et al. Reference Magnusson, Rasmussen, Lawlor, Tynelius and Gunnell2006) and height (Whitley et al. Reference Whitley, Rasmussen, Tynelius and Batty2010) at conscription have all been shown to be associated with future risk of suicide and both cognitive performance and BMI are also associated with cardiovascular fitness (Åberg et al. Reference Åberg, Pedersen, Torén, Svartengren, Bäckstrand, Johnsson, Cooper-Kuhn, Åberg, Nilsson and Kuhn2009; Pahkala et al. Reference Pahkala, Hernelahti, Heinonen, Raittinen, Hakanen, Lagstrom, Viikari, Ronnemaa, Raitakari and Simell2013). Further, we recently showed that lower cardiovascular fitness at conscription was associated with increased risk of serious depression in adulthood (Åberg et al. Reference Åberg, Waern, Nyberg, Pedersen, Bergh, Åberg, Nilsson, Kuhn and Torén2012).
We performed a prospective cohort study of all Swedish men born in 1950–1987 who at conscription at age 18 years had no history of mental illness. The first aim was to determine whether cardiovascular fitness at conscription was associated with future risk of suicide attempt or suicide death during a follow-up time of 5–42 years. The second aim was to examine how cognitive performance, BMI, height and depression would make an impact on the hypothesized relationship between fitness and suicide attempt or suicide death. A third aim was to study the relationship between cardiovascular fitness and cognitive performance and future risk of suicidal behaviour.
Method
Participants
A cohort of 18-year-old Swedish males who enlisted for military service between 1968 and 2005 (i.e. born between 1950 and 1987; n = 1 353 723) was compiled from the Swedish Military Service Conscription Register. During that time Swedish law required all 18-year-old Swedish men to enlist. Exemptions were granted only for incarcerated males, severe chronic medical or mental conditions, or functional disabilities documented by a medical certificate (approximately 2–3% of the 18-year-old male population each year). When enlisting, males underwent extensive and highly standardized physical and psychological examinations prior to assignment in the Swedish Armed Forces. Conscripts with any history of mental illness or ongoing psychiatric disorders at the time of the examination (n = 69 609) were excluded from the current study. All Swedes have a unique personal identification number making linkage to other registers possible. The Ethics Committee of the University of Gothenburg and Confidentiality Clearance at Statistics Sweden approved the study.
Swedish military service conscription register data
Cardiovascular fitness test
Cardiovascular fitness was assessed using the cycle ergonometric test. The procedure, including elements of validity and reliability, has been described in detail previously (Nordesjö & Schéle, Reference Nordesjö and Schéle1974). Briefly, after a normal resting electrocardiogram, 5 min of submaximal exercise was performed at work rates of 75–175 W, depending on body weight. The work rate was continuously increased by 25 W/min until volitional exhaustion. The subject was instructed to maintain pedal cadence between 60 and 70 revolutions per min. Heart rate was continuously measured. The final work rate (Wmax) was recorded and divided by body weight. This measure was employed because it yielded a better correlation with maximum oxygen consumption (
![]() ${\rm V_{{O_2}max}}$
) (correlation coefficient about 0.9) than predicted
${\rm V_{{O_2}max}}$
) (correlation coefficient about 0.9) than predicted
![]() ${\rm V_{{O_2}max}}$
(correlation coefficient about 0.6–0.7). The resulting values (Wmax/kg) were transformed into stanine (STAndard NINE) scores that served as a measure of cardiovascular fitness.
${\rm V_{{O_2}max}}$
(correlation coefficient about 0.6–0.7). The resulting values (Wmax/kg) were transformed into stanine (STAndard NINE) scores that served as a measure of cardiovascular fitness.
Cognitive tests
The cognitive performance tests are described in detail elsewhere (Carlstedt, Reference Carlstedt2000) and data have been employed in other studies (Gunnell et al. Reference Gunnell, Magnusson and Rasmussen2005; Åberg et al. Reference Åberg, Pedersen, Torén, Svartengren, Bäckstrand, Johnsson, Cooper-Kuhn, Åberg, Nilsson and Kuhn2009; Sörberg et al. Reference Sörberg, Allebeck, Melin, Gunnell and Hemmingsson2013). Four cognitive tests were used during the period of assessment covered by the current study: logical performance test, verbal test of synonym and opposites, test of visuospatial/geometric perception, and technical/mechanical skills including mathematical/physics problems. Results from all four tests were combined yielding a combined intelligence score, which was regarded as a measure of general cognitive performance. Procedures for carrying out the cognitive tests changed in 1980 (Carlstedt, Reference Carlstedt2000) but others who have used these conscription data (Gunnell et al. Reference Gunnell, Magnusson and Rasmussen2005) as well as our own group (Åberg et al. Reference Åberg, Pedersen, Torén, Svartengren, Bäckstrand, Johnsson, Cooper-Kuhn, Åberg, Nilsson and Kuhn2009) have shown that the procedural alteration did not affect the associations examined. Test results were standardized against data from previous years to give scores from 1 (low) to 9 (high) with a Gaussian/normal distribution for each of the five scores: combined intelligence, logical, verbal, visuospatial, and technical/physics scores. The standardization to a nine-point ‘stanine’ scale provided long-term stability of the datasets. Before 1996 raw data were not electronically recorded and only stanine scores could be accessed for statistical analysis.
Diagnoses recorded at conscription
Conscripts were assessed by psychologists and physicians during the conscription examination. Those (n = 69 609) who met criteria for previous or ongoing psychiatric disorders [International Classification of Diseases (ICD)-8 and -9 codes 290–319; ICD-10 codes F00–F99; all mental and behavioural disorders] were excluded from the current analyses.
Outcomes
Suicide attempt
Attempted suicide diagnoses were obtained from the Swedish National Hospital Discharge Register, which is maintained at the National Board of Health and Welfare. The Swedish National Hospital Discharge Register covers virtually all in-patient care for psychiatric disorders since 1964. Discharge diagnoses are coded by the physician in accordance with the ICD versions 8, 9 or 10 (ICD-8, ICD-9 and ICD-10). We identified diagnostic codes for first episode of hospitalization for attempted suicide from 1968 to 31 December 2010. The specific ICD-8, ICD-9 and ICD-10 codes that were used in the analyses are shown in Table 1.
Table 1. Numbers of male conscripts with hospital record of suicide attempt or suicide death without previous attempt during up to 42 years of follow-up by method-specific ICD codes a

ICD, International Classification of Diseases.
a For persons with repeat behaviours, only first episodes are shown.
Suicide death
Suicide deaths were identified by linkage with the Cause of Death Register, which is maintained at the National Board of Health and Welfare. The Swedish Cause of Death Register, which covers virtually all deaths since 1961, is annually updated based on death certificate diagnoses. See Table 1 for specific ICD-8, ICD-9 and ICD-10 codes.
Covariates from other data sources
LISA
Education and occupation information was obtained from the longitudinal integration database for health insurance and labour market studies (Swedish acronym LISA). The LISA database (http://www.scb.se/Pages/List____257743.aspx) at Statistics Sweden was initiated in 1990 and includes all registered residents aged 16 years and older. The database, which is annually updated, integrates data from the labour market, as well as educational and social sectors. Information on parental education was obtained from LISA (80% coverage) and was rated in seven levels: pre-high school education less than 9 years, pre-high school education 9 years, high school education, college education (less than 2 years), college education (2 or more years), postgraduate education and postgraduate research training.
Multi-Generation Register
Links to the Multi-Generation Register (http://www.scb.se/Pages/List____257501.aspx; website in Swedish) at Statistics Sweden enabled the identification of full brothers.
Statistical analysis
All statistical calculations were performed with SAS version 8.1 (SAS Institute Inc., USA). The follow-up period began at the date of conscription (baseline) and subjects were censored at the time of (1) first suicide attempt or (2) suicide (in cases without prior attempt) or (3) death from other causes or (4) at the end of follow-up, i.e. on 31 December 2010 (minimum 5 years and maximum 42 years of follow-up). We used Cox proportional hazards models to assess the influence of cardiovascular performance at age 18 years and potential confounders on the occurrence of first onset of suicide attempt or suicide death during the observation period. Cardiovascular fitness scores were transformed to stanines that were categorized as ‘low’ (stanine score 1–3), ‘medium’ (stanine score 4–6) and ‘high’ (stanine score 7–9); the ‘high’ group was the reference category. Since cardiovascular fitness was not normally distributed (see online Supplementary Table S1), separate analyses were also performed with ‘low’ cardiovascular fitness as stanine score 1–4, ‘medium’ as stanine score 5–7 and ‘high’ as stanine score 8–9.
Age was used as the time axis in the Cox model, thus controlling for age. To assess effects of secular variation in rates of suicide attempt or suicide death and differences in conscription procedures over time, we adjusted for calendar years by stratifying the Cox model by conscription decade (1960s, 1970s, etc.).
To reduce the risk for possible reverse causation, i.e. suicidal thoughts affecting performance on the physical tests, we restricted the analysis to men with no mental illness at the conscription examination and no previous episodes of in-patient psychiatric care in accordance with the National Hospital Register. To further reduce baseline misclassification, we performed separate analyses excluding incident cases of suicide attempt or suicide death during the year following the conscription examination.
Because differences among regions and test centres could introduce bias, geographical region and conscription test centres were considered as possible confounders and were adjusted for.
Adjustment for the continuous variables BMI and height were performed. Education levels for each parent were included as confounders (Nock et al. Reference Nock, Greif Green, Hwang, McLaughlin, Sampson, Zaslavsky and Kessler2013). Also adjustment for cognitive performance at conscription was performed.
To further assess potential effects of familial factors, subanalyses were performed within full brother pairs of conscripts. We used the Cox's proportional hazards model adjusting for the above-listed confounders including also suicide attempt or suicide death in one or more male siblings as an additional explanatory variable. This inclusion was independent of temporal relation to the brother's suicidal behaviour within the observation period.
The fact that the study spans a long time could have made an impact on our results due to latency of effect. To study how follow-up time affected the associations, separate analyses were performed with the follow-up times: 1–10, 11–20, 21–30 and 31–42 years.
Separate Cox models were performed to assess the influence of cardiovascular performance and potential confounders on the occurrence of suicide death during the observation period.
In a final set of analyses focusing on the suicidal behaviour outcome, we looked specifically at interactions involving both cardiovascular and cognitive performance data, first by stratifying by level of cognitive performance and second by combining low, medium and high performance in nine separate groups; the high cardiovascular/high cognitive performance group was the reference category.
Due to the large number of observations, the p values were very small [in all analyses when the 95% confidence interval (CI) was separated from 1 the p values were <0.0001]. Therefore p values are not reported and the risk for type I errors is considered very low.
Results
Our analyses are based on the 1 136 527 mentally healthy conscripts with no prior history of attempted suicide and with complete information from military conscription. At least one suicide attempt was registered for 12 563 individuals during the observation period (Table 1). Suicide was the cause of death for a total of 5857 of the men in the cohort; 4814 of these had no previous registration of attempted suicide. In all, there were 17 377 cases with first onset of suicide attempt or suicide death during the observation period, corresponding to 1.53% of the total sample. The mean time from assessment of cardiovascular fitness at age 18 years to the first admission for attempted suicide was 14.1 years. For those with no previous attempt, the mean time from the evaluation and death by suicide was 15.5 years. Numbers with first onset of suicide attempt or suicide death are shown by level of follow-up time in online Supplementary Fig. S1.
Cardiovascular fitness at age 18 years and future suicide attempt or suicide
Numbers and proportions with suicide attempt or suicide death during the observation period are shown by level of cardiovascular fitness at age 18 years in online Supplementary Table S1. Poor performance on the cardiovascular fitness test was associated with an increased risk for suicide attempt/death (Table 2). We found an inverse relationship with the highest hazard ratios (HRs) for suicidal behaviour in the low cardiovascular fitness group (stanine score 1–3). The strength of the associations changed little in models that controlled for calendar year, BMI, conscription test centre, parental education and height. However, the HR in the low cardiovascular fitness group was attenuated by 29% [the relative change between HRs 2.23 and 1.87 calculated as (HRunadj – HRadj)/(HRunadj – 1.0)] when controlling for cognitive performance at conscription. Data were reanalysed using a different categorization of cardiovascular fitness (see Statistical analysis) and this procedure yielded similar HRs (results not shown). Therefore, stanine score 1–3 was used as ‘low’, stanine score 4–6 as ‘medium’ and stanine score 7–9 as ‘high’ cardiovascular fitness in all following analyses.
Table 2. Risk for suicide attempt/death in relation to cardiovascular fitness in a national cohort of 18-year-old male conscripts (n = 1 136 527)

Data are given as hazard ratio (95% confidence interval).
a With age-adjusted and fully adjusted models.
b Suicide attempt/death.
c Adjusted for calendar year, body mass index.
d Reference category: high.
e Adjusted for calendar year, body mass index, conscription test centre, parental education.
f Adjusted for calendar year, body mass index, conscription test centre, parental education, intelligence quotient.
g Adjusted for calendar year, body mass index, conscription test centre, parental education, intelligence quotient, height.
h Subanalyses after exclusion of conscripts (n = 3348) with in-patient depression preceding or coinciding with the suicidal behaviour and with a latency time for suicide attempt/death within 1 year after conscription examination.
i Subanalyses for conscripts (n = 336 055) with one or more full-brothers. Suicide attempt/death in one or more brother included in the model as an additional explanatory variable.
j Adjusted for calendar year, body mass index, conscription test centre.
k Adjusted for calendar year, body mass index, conscription test centre, intelligence quotient.
l Adjusted for calendar year, body mass index, conscription test centre, intelligence quotient, height.
m One or more brothers with suicidal behaviour.
Separate analyses excluding individuals with in-patient treatment for depression preceding or coinciding with the first onset of suicide attempt or suicide death and excluding incident cases of suicide attempt or suicide death during the year following the conscription examination (i.e. a latency time of 1 year) yielded similar results.
In the total cohort there were 336 055 subjects with one or more full-brothers. While having one or more brothers with suicide attempt or suicide death was associated with a threefold increased risk of future suicidal behaviour, both low and medium cardiovascular fitness remained significant predictors in the model.
Three ICD versions were utilized during the long observation period. As this might affect results, we carried out separate analyses for each ICD system. These analyses showed similar associations between cardiovascular fitness and future suicidal behaviour but with twofold higher HRs within the ICD-10 compared with ICD-8/9. In order to see if there were changes in the effect size with greater follow-up time, subgroups were created for 10-year periods with respect to conscription year and length of follow-up. Higher HRs were observed closer to baseline within the same ICD version (Table 3).
Table 3. Risk for suicide attempt/death in relation to cardiovascular fitness at age 18 years by 10-year follow-up periods in male conscripts (n = 1 136 527)

Data are given as hazard ratio (95% confidence interval). Adjusted for calendar year, body mass index, conscription test centre.
ICD, International Classification of Diseases.
a Reference category: high.
There may be systematic differences between individuals who attempted suicide and those who committed suicide. Therefore, we performed separate analyses including only suicide death with or without previous suicide attempt as outcome (n = 5857). In fully adjusted models poor performance on the cardiovascular fitness test was not associated with an increased risk for suicide death (HR 0.96, 95% CI 0.80–1.15). Separate analyses excluding individuals with in-patient treatment for depression preceding or coinciding with suicide death and excluding incident cases of suicide death during the year following the conscription examination (i.e. a latency time of 1 year) yielded similar results.
Relationships between physical and cognitive performance at age 18 years and future suicidal behaviour
In the final set of analyses, we wanted to study interactions between cardiovascular fitness and cognitive performance and future risk of suicidal behaviour. Supplemental data regarding the relationship between cognitive performance and suicide attempt or suicide death are presented in online Supplementary Tables S1 and S2.
Table 4 shows that low and medium (compared with high) cardiovascular fitness was associated with an increased risk of future suicidal behaviour when stratified for ‘low’, ‘medium’ and ‘high’ cognitive performance. It demonstrates the lack of an interaction between cardiovascular fitness and cognitive performance. This indicates that cardiovascular fitness is an important predictor for later suicidal behaviour independent of cognitive performance.
Table 4. Risk for suicide attempt/death in relation to cardiovascular fitness by cognitive performance (intelligence quotient) at age 18 years in male conscripts (n = 1 136 527)

Data are given as hazard ratio (95% confidence interval).
a Suicide attempt/death.
b Adjusted for calendar year, body mass index.
c Adjusted for calendar year, body mass index, conscription test centre, parental education.
d Adjusted for calendar year, body mass index, conscription test centre, parental education, height.
e Reference category: high.
Subsequently nine separate groups were created by combining ‘low’, ‘medium’ and ‘high’ performance; the ‘high’ cardiovascular/‘high’ cognitive performance group was the reference category (online Supplementary Table S3 and Fig. 1). Poor performance (category ‘low’) on both the cognitive and cardiovascular fitness tests was associated with a fivefold increased risk of attempted suicide/death by suicide. Having high cardiovascular fitness but low cognitive performance reduced the risk to threefold. Although cognitive performance seems to have a larger effect on later suicidal risk than cardiovascular fitness per se, a high cardiovascular fitness (compared with low) reduced future risk of suicidal behaviour in all cognitive performance levels.
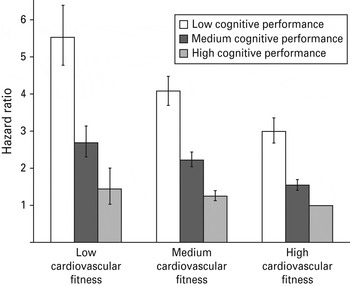
Fig. 1. Risk for suicidal behaviour for 18-year-old male conscripts (n = 1 136 527) with different levels of cognitive performance, shown by level of cardiovascular fitness. All values are from fully adjusted models in online Supplementary Table S3 (Depression excluded and 1 year latency time section). Data are hazard ratios, with 95% confidence intervals represented by vertical bars.
Discussion
In this national cohort study, we demonstrate that low cardiovascular fitness in early adulthood is associated with a twofold increased risk of suicidal behaviour during up to 42 years of follow-up. Relationships followed a dose–response pattern. Associations were only slightly attenuated after controlling for a number of possible covariates including serious depression. The associations between cardiovascular fitness and later suicidal risk were attenuated by 29% after controlling for cognitive performance. The combination of low cardiovascular fitness and low cognitive performance resulted in a fivefold increase in later risk of suicide attempt or suicide death.
The present study is a prospective study with a national population-based cohort of over a million individuals, objective measures of both cardiovascular fitness and cognitive performance, and a long follow-up time. The Swedish National Hospital Discharge Register enables us to cover virtually all in-patient care for suicide attempts during 42 years. Similarly, the Swedish Cause of Death Register covers all confirmed suicides during these years.
As the use of three separate ICD systems might affect results, we carried out separate analyses for each ICD version (8/9/10). Indeed, the associations between cardiovascular fitness and suicidal behaviour differed depending on which ICD version was used. Specifically, higher HRs were observed within the ICD-10. We have previously reported the same phenomenon for other associations (Åberg et al. Reference Åberg, Waern, Nyberg, Pedersen, Bergh, Åberg, Nilsson, Kuhn and Torén2012). While this may be an artifact it could also reflect a true secular variation that might be related to differences in diagnosis rate or treatment regimens over time. Also, while ICD-8 and ICD-9 are considered to be very similar, the ICD-10 is somewhat different. Clinical diagnoses are more clear and specific in this later version. More specific diagnoses would be expected to yield higher HRs.
An additional strength of this study is the reliance on psychologists and physicians for baseline assessment of mental health history, allowing us to exclude individuals with pre-existing psychiatric disorders, thereby reducing the risk of reverse causation. Also by including parental educational level as a confounder and by performing subanalyses within full-brother pairs, many early childhood risk factors could be accounted for, including genetics and parental treatment and upbringing.
However, there are also drawbacks of the current design. Data on cardiovascular fitness were available at baseline only. The incidence of attempted suicide is underestimated, as some do not seek hospital care in connection with a suicide attempt. Similarly, some actual suicides may have been categorized as deaths of uncertain cause.
Although we could adjust for parental education and suicidal behaviour in brothers we were not able to adjust for specific early developmental influences such as childhood psychiatric problems which did not require in-patient care or parental death that may have affected the associations (Sourander et al. Reference Sourander, Klomek, Niemela, Haavisto, Gyllenberg, Helenius, Sillanmaki, Ristkari, Kumpulainen, Tamminen, Moilanen, Piha, Almqvist and Gould2009; Kuramoto et al. Reference Kuramoto, Runeson, Stuart, Lichtenstein and Wilcox2013). Further, although the conscripts underwent extensive examinations by psychologists, subsyndromal states that might have affected the future risk of suicidal behaviour may have been missed, and some may have opted not to tell about previous episodes of suicidal behaviour. Suicide attempts are common in youth, with accumulated prevalence figures as high as 1% in Swedish and 2% in American male teens up to the age of 18 years (Zetterqvist et al. Reference Zetterqvist, Lundh and Svedin2012; Nock et al. Reference Nock, Greif Green, Hwang, McLaughlin, Sampson, Zaslavsky and Kessler2013). Conscripts who neglected to report previous suicide attempts or episodes of mental ill-health would be inappropriately included in our study if they had no previous record of psychiatric hospitalization. Results from our study cannot be directly extrapolated to women or to other settings, as patterns of suicidal behaviour differ between men and women and among different cultures (Nock et al. Reference Nock, Borges, Bromet, Cha, Kessler and Lee2008, Reference Nock, Greif Green, Hwang, McLaughlin, Sampson, Zaslavsky and Kessler2013).
There are possible confounders that may increase risk for both poor fitness and suicide attempt or suicide death. A couple of cross-sectional epidemiological studies have documented an association between self-reported sedentary life-style in adolescence and suicidal behaviour (Brown & Blanton, Reference Brown and Blanton2002; Babiss & Gangwisch, Reference Babiss and Gangwisch2009). They conclude that self-esteem and social support are important mediators of the relationships between sports participation and suicidal ideation. We were not able to control for self-esteem, personality and socio-environmental circumstances at the time of conscription/later in the life course that may have affected the associations.
Biological risk factors associated with major depression contribute to the aetiology of suicidal behaviour (Coryell, Reference Coryell2006). Several cross-sectional and a few prospective epidemiological studies have documented an association between self-reported sedentary life-style and depression (Farmer et al. Reference Farmer, Locke, Moscicki, Dannenberg, Larson and Radloff1988; Buckworth & Dishman, Reference Buckworth and Dishman2002; Strawbridge et al. Reference Strawbridge, Deleger, Roberts and Kaplan2002; Harvey et al. Reference Harvey, Hotopf, Overland and Mykletun2010). Therefore, a possible explanation for the association between cardiovascular fitness in young adulthood and suicidal behaviour later in life could be mediated via a protective effect of physical fitness on depression. Depression is indeed an important risk factor for suicidal behaviour; however, it is somewhat less salient at younger ages (Hunt et al. Reference Hunt, Kapur, Robinson, Shaw, Flynn, Bailey, Meehan, Bickley, Parsons, Burns, Amos and Appleby2006). This paper focuses on first episode of suicidal behaviour, which in many cases occurred at a relatively young age, a time of life when depression might play a less prominent role in suicide-related outcomes. The association with cardiovascular fitness remained after exclusion of individuals with in-patient depression preceding or coinciding with the first episode of suicidal behaviour. Further, the association between cardiovascular fitness and suicidal behaviour appeared to be connected to suicide attempt in our study; associations with suicide death were not significant. If depression had been the main mediator of the association we would have expected to find larger HRs for death by suicide than for the combined suicide attempt/suicide death outcome as those who die by suicide would be more likely to be depressed than those with non-fatal attempts. Taken together, our findings suggest that the reduced risk for future suicidal behaviour observed in those with better cardiovascular performance at the age of 18 years might in part be attributed to a mechanism other than a protective effect of physical fitness on depression. There are data at the molecular biological level indicating that the increased susceptibility of certain individuals towards suicidal behaviour stems from disruptions in the hypothalamic–pituitary–adrenal axis (Wasserman et al. Reference Wasserman, Wasserman and Sokolowski2010) and expression of brain-derived neurotrophic factor (BDNF) (Dwivedi, Reference Dwivedi2009), which may be independent of depression. Interestingly, these disruptions are positively affected by physical exercise (Zheng et al. Reference Zheng, Liu, Li, Yang, Chen, Wang, Jiang, Wang, Wang, Cornelisson and Halberg2006; Griffin et al. Reference Griffin, Mullally, Foley, Warmington, O'Mara and Kelly2011) and one may speculate that physical exercise in young adulthood could contribute to an increased brain reserve capacity (Nithianantharajah & Hannan, Reference Nithianantharajah and Hannan2009) which might reduce the risk of suicidal behaviour in times of distress. One mechanism underlying these effects of exercise on brain function could be the robust increase in the generation of new neurons in the adult hippocampus (van Praag et al. Reference van Praag, Kempermann and Gage1999; Brown et al. Reference Brown, Cooper-Kuhn, Kempermann, van Praag, Winkler, Gage and Kuhn2003). There is emerging evidence of the possible involvement of hippocampal neurogenesis in mediating the beneficial effects of physical exercise on counteracting stress (Yau et al. Reference Yau, Lau and So2011).
Both physical fitness and cognitive performance in late adolescence seem to be important predictors for later suicidal behaviour. We found that cardiovascular fitness was associated with future suicidal risk independently of cognitive performance. At the individual level it may be difficult to change cognitive performance; however, cardiovascular performance is possible to improve. A greater understanding of the mechanisms underlying these associations including complex bidirectional models may provide opportunities and strategies for prevention (de Jonge & Roest, Reference de Jonge and Roest2012). While our results cannot be extrapolated to adolescents with previous episodes of mental illness and suicide attempts, future studies could test the usefulness of exercise programmes for these individuals. Evaluating new strategies could prove to be clinically important, considering the difficulty of reducing suicidal behaviours among young people (Gibbons et al. Reference Gibbons, Brown, Hur, Davis and Mann2012).
Supplementary material
For supplementary material accompanying this paper, please visit http://dx.doi.org/10.1017/S0033291713001207.
Acknowledgements
This study was supported by grants from the Märtha Lundqvists Stiftelse, the Swedish Research Council for Worklife and Social Science (FAS), the Swedish Research Council and the Swedish government under the LUA/ALF agreement for biomedical research. The authors thank Dr Tommy Johnson for statistical help and advice.
Declaration of Interest
None.







