Atrial septal defects (ASDs) are common and can present at any age, and females constitute 65 to 75% of patients with secundum ASDs.Reference Webb and Gatzoulis1 Pulmonary valve stenosis is less commonly associated with ASD. Percutaneous device closure is currently the treatment of choice for congenital heart defects, which are amenable for closure, and the femoral vein is the conventional approach for such interventions. Interrupted inferior vena cava (IVC) is a congenital anomaly/variant which is associated with other defects. This precludes our choice of vascular access and necessitates other approaches like the jugular vein from which conventional device deployment strategies cannot be employed, and dextrocardia further complicates the procedure. We report a case in which we employed an unconventional method of device deployment successfully in this complex anomaly.
Case report
A 20-year-old female patient presented to us with a history of shortness of breath of 1-month duration. She had a loud ejection systolic murmur in the right second intercostal space. On echocardiography, she had situs inversus with dextrocardia and ostium secundum ASD of size 32 mm with adequate rims and severe valvular pulmonary stenosis (Fig 1a). Transesophageal echo was not helpful due to poor window because of dextrocardia. Cardiac magnetic resonance was done to rule out additional defects as well as to size the defect accurately. Inferior venocavogram done in anteroposterior and lateral views demonstrated an interrupted infra-hepatic segment of the IVC with azygos continuation (Fig 1b).

Figure 1. (a) Transthoracic echocardiography with color Doppler in the parasternal short-axis view illustrating the atrial septal defect with left to right shunt (the probe has been inverted to get the normal anatomical orientation). (b) Angiogram of the inferior vena cava in the lateral view showing the inferior vena cava continuing as azygus vein and joining the superior vena cava.
Through the left internal jugular vein access, the ASD was crossed with a 0.035-inch hydrophilic guidewire after multiple attempts and manipulation with an Amplatz left catheter after failing with Judkin’s right and multipurpose catheters. The guidewire did not support the sheath into the pulmonary vein, so the device was tried deploying from the left atrium. The device could not be aligned with multiple strategies and was repeatedly prolapsing into the right atrium. Then, a Lunderquist wire was placed in the left ventricle apex over which a 14 Fr sheath was positioned (Fig 2a). Even from the left ventricle, the device could not be aligned by deploying it immediately after pulling it into the left atrium. Finally, under transthoracic echo guidance, a Ceraflex septal occluder (Lifetech, Shenzen, China) of size 36 mm was partially deployed in left ventricle inflow across the mitral valve leaflets avoiding entanglement in the chordae (Fig 2b, supplementary video 1). The device was slowly pulled from across the mitral valve, and the left atrial disc was fully deployed and later, the right atrial disc was deployed (Fig 3a, supplementary video 2), achieving a stable position. After this, the pulmonary valve was crossed using hydrophilic straight tipped wire (Terumo glide wire), which was exchanged with an Amplatzer extra stiff wire over which the pulmonary valvuloplasty was done with an Atlas balloon of size 24 × 40 mm (Fig 3b). The pre-dilation peak gradient across the pulmonary valve was 60 mmHg, which decreased to 15 mmHg after dilation. The patient is asymptomatic, and 1-year echocardiographic follow-up showed no residual shunt across the interatrial septum and a residual peak gradient of 18 mmHg across the pulmonary valve (Fig 4).

Figure 2. (a) Lunderquist wire along with the sheath being placed in the left ventricular apex from the left internal jugular vein in anteroposterior view on fluoroscopy. (b) Transthoracic echo showing the device being deployed in the left ventricular inflow across the mitral valve leaflets to align the device. (The echo view has been inverted at the time of acquisition for better understanding.)

Figure 3. (a) Fluoroscopy in the left anterior oblique view showing the device fully deployed with a good waist of the device. (b) Fluoroscopy in the lateral view depicting the balloon pulmonary valvuloplasty.
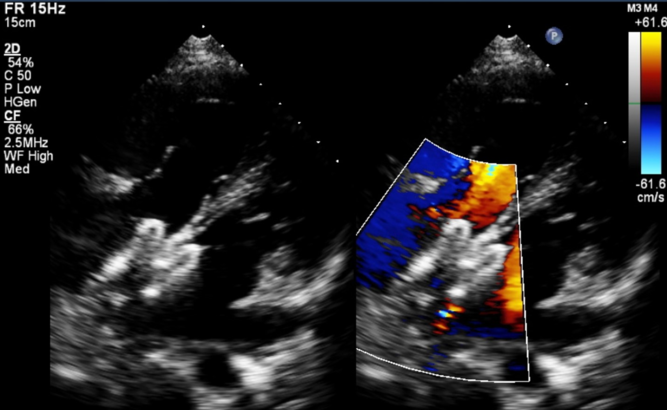
Figure 4. Transthoracic echo with colour Doppler study showing the atrial septal occluder in position without any residual shunt (echo images acquired with the probe inverted).
Discussion
Compared to surgical closure, transcatheter ASD closure is associated with fewer complications and faster hemodynamic improvement.Reference Eerola, Pihkala, Boldt, Mattila, Poutanen and Jokinen2 In the presence of an obstruction or interruption of the IVC, alternate vascular access is needed for the intervention. Transhepatic access has been used as an alternative venous access for the percutaneous ASD closure, but an increased risk of complications is possible.Reference Hussain, Strumpf, Ghandforoush, Jamal and Diethrich3 We chose the jugular vein on the left side as the patient had left superior vena cava. From this approach, we could not achieve stable wire and sheath position from the pulmonary veins because of the anatomy and stiffness of the wire, and the procedure became challenging due to dextrocardia. A single case has been reported so far in which device closure of the ASD was done in the presence of interrupted IVC and dextrocardia.Reference Oliveira, Moura, Almeida, Ribeiro and Nascimento4
Multiple challenges were observed in this procedure. First, crossing the ASD due to abnormal orientation of the atrial septum, which needed an Amplatz curve catheter. Second, the extra stiff wire could not be placed in the pulmonary vein due to the tortuosity resulting in the inability to utilise pulmonary vein device deployment. Third, the device could not be aligned to the septum from the left atrium. The upper side of the left atrial disc would prolapse into the right atrium immediately after deployment leading to malalignment. The device could only be aligned and deployed after releasing the left atrial disc in the left ventricle inflow across the mitral valve leaflets. A similar approach has been taken before, but the device was opened only after pulling it back into the left atrium by Ozdemir E et al.Reference Ozdemir, Emren, Eren, Nazli and Tokac5; but in our patient, we had to do it in the left ventricle inflow across the mitral valve to align it to the septum. Caution was taken to open it just across the leaflets and not entangle in the chordae. Other methods that could have been tried are the balloon-assisted technique and modification of the tip of the delivery sheath. A balloon positioned in the upper part of the defect may prevent the device from prolapsing, but it needs another jugular vein puncture in our patient. If the tip of the sheath is bevelled, it can retain the device in the left atrium, but it needs modification by the physician. Due to the lack of a proper transesophageal echo window, the procedure was done under transthoracic echo guidance. Lastly, the co-existing pulmonary stenosis needed the passage of a wire/balloon-tip catheter across the right ventricular outflow tract, which was difficult due to the extremely tortuous course. The pulmonary valve was doming with favourable anatomy, which had a high chance of success. ASD was a complex lesion, so device closure was attempted before the valvuloplasty.
Conclusion
Alternative access sites for percutaneous ASD closure such as the left internal jugular vein can be safely used. The non-conventional approach needs modification of the routine deployment techniques.
Acknowledgements
None.
Supplementary material
To view supplementary material for this article, please visit https://doi.org/10.1017/S104795112000178X
Financial support
This research received no specific grant from any funding agency, commercial or not-for-profit sectors.
Conflicts of interest
None.






