Introduction
Functional endoscopic sinus surgery (FESS) is the standard surgical procedure for managing chronic rhinosinusitis with or without nasal polyposis. It aims to restore mucociliary function by re-establishing physiological sinus ventilation and drainage. This improves the quality of life of patients suffering from this common disease. However, like other surgical procedures, FESS too is associated with myriad complications. These complications can be due to the surgery or to the disease itself. In this context, it would be prudent to note that nasal anatomy is intrinsically related to the orbit and the skull. Hence, anatomical structures within the orbit and skull base, like the lacrimal apparatus, extraocular muscles, optic nerve and carotid artery, are prone to injury. The complications associated with FESS include haemorrhage, retrobulbar haemorrhage, infection, cerebrospinal fluid rhinorrhoea, and temporary or permanent blindness.Reference Lal, Stankiewicz, Flint, Haughey, Lund, Niparko, Robbins and Thomas1
Although extensive research has been conducted on most of these FESS-related complications, only few studies have specifically investigated nasolacrimal duct injury.Reference Ali, Murphy, Wormald and Psaltis2–Reference Bolger, Parsons, Mair and Kuhn7 Minor injuries usually heal without any stenosis or symptoms. Hence, most of these injuries remain unnoticed. A review of the limited literature on the subject revealed that 15 per cent of patients with FESS have lacrimal drainage system injury, of whom 0.3–1.7 per cent have symptomatic epiphora.Reference Bolger, Parsons, Mair and Kuhn7 These studies have evaluated this injury by fluorescein dye test, lacrimal irrigation test, Jones test, and dacryocystography or active transport dacryocystography.Reference Bolger, Parsons, Mair and Kuhn7 These methods are invasive and require an ophthalmologist.
A recent review of the literature cites the role of radiology in determining nasolacrimal duct injury in FESS.Reference Ali, Murphy, Wormald and Psaltis2 The nasolacrimal duct is clearly demarcated on computed tomography (CT) of the nose and paranasal sinuses (especially axial cuts), which is carried out routinely for FESS. Thus, radiology could be a very useful tool to evaluate nasolacrimal duct dehiscence and trauma related to FESS.
This paper presents our results on nasolacrimal duct injury in FESS, using the ‘swing door’ technique of uncinectomy, evaluated by radiology. To the best of our knowledge, this is the first prospective study to analyse nasolacrimal duct injury radiologically.
Materials and methods
This prospective observational study was carried out in the Department of Otorhinolaryngology – Head and Neck Surgery at Lady Hardinge Medical College, New Delhi, India, a tertiary care central government teaching hospital, from October 2016 to April 2018. The study was ethically cleared by the Medical Division of the University Board of Studies, University of Delhi, India. The study population comprised 50 adults of either sex, aged above 18 years.
The inclusion criteria were as follows. Chronic rhinosinusitis was defined as rhinosinusitis for a duration of more than 12 weeks despite medical management. Patients suffering from with chronic rhinosinusitis were given medical management with antibiotics, nasal decongestants and topical steroids for four weeks.Reference Lal, Stankiewicz, Flint, Haughey, Lund, Niparko, Robbins and Thomas1 Those patients for whom this treatment protocol failed were recruited into the study. The antibiotic was determined on the basis of culture and sensitivity. In the case of sterile culture or no pus, patients were treated with cefuroxime, a second-generation cephalosporin, (dose of 500 mg twice daily). Fluticasone nasal spray was used for topical steroid therapy. Patients with chronic rhinosinusitis with polyps were also included.
Patients were excluded from this study if they: were aged less than 18 years, had a previous history of FESS, had a sinonasal neoplasm, had an abnormal blood coagulation profile or were pregnant.
A detailed clinical investigation was carried out for all the patients and was duly recorded in a proforma. All patients underwent routine investigations (haemoglobin, bleeding time, clotting time, random blood sugar, urine examination, chest X-ray in a posterior-anterior view). Patients underwent other specific investigations if required for local or general anaesthesia.
A CT scan of the paranasal sinuses was performed in all cases, to delineate the extent of disease. Chronic rhinosinusitis was graded in accordance with the Lund–Mackay classification.
Radiology of nasolacrimal duct
All patients underwent multidetector CT scanning (using a Philips Brilliance 40-slice scanner). A volume scan without intravenous contrast was performed on all patients. In supine position, the axial plane was kept parallel to the inferior orbitomeatal plane, and scans were taken from the superior wall of the frontal sinus to the hard palate. The scans were obtained at 120 KVp and 80–100 mAs in a field of view of 180 mm. From these data, images were reconstructed in the axial, coronal and sagittal planes, with bone and soft tissue algorithms, with a slice thickness of 0.9 mm.
The CT scan images were evaluated to establish: nasolacrimal duct anatomy, including any dehiscence; and the extent of sinus disease in both soft tissue and bone window settings, in all planes. The nasolacrimal duct is seen as a circular opening at the anteromedial corner of the maxillary sinus. Its anterolateral walls are thick, whereas the medial wall is comparatively thinner. Following FESS, CT scan images were evaluated to determine any damage to the nasolacrimal duct, and compared with the pre-FESS CT scan.
Intervention
All patients underwent FESS using the ‘Messerklinger technique’ with ‘swing door’ uncinectomy. All the sinuses involved were judiciously addressed. After the surgical procedure had been completed and complete haemostasis was achieved, Merocel® nasal packs were placed. The packs were removed after 24 hours and the patient was discharged. Post-operatively, all the patients received a course of antibiotics (cefuroxime 500 mg twice daily) for a period of 7 days, along with analgesics (diclofenac plus paracetamol) for 3 days; thereafter, analgesics were given only on demand.
Follow up
The patients were regularly followed up and clinically evaluated, at the end of the first, second, fourth and sixth week after surgery. Repeat CT scanning of the nose and paranasal sinuses was performed at the end of four weeks. Radiological evaluation of nasolacrimal duct dehiscence or injury before and after FESS was recorded in a proforma, in consultation with the radiologist.
Results
Out of a total of 50 patients recruited in the study, 7 were lost to follow up. Hence, the statistical data and interpretation are presented for the remaining 43 patients, in accordance with the study protocol. Some interesting facts about our data are enumerated below.
The youngest case in our study was 18 years old and the oldest patient was 60 years old. Of the 43 patients, 30 (69.77 per cent) were male and 13 (30.23 per cent) were female (male-to-female ratio of 2.3:1); hence, there was a male preponderance. Most of the patients (n = 32; 74.42 per cent) had experienced symptoms for more than one year, and nasal obstruction was the commonest symptom. Out of the 43 patients, 13 (30.23 per cent) had nasal polyposis.
Nasolacrimal duct injury or dehiscence
In the present study, pre-operatively, only one case of nasolacrimal duct dehiscence was observed (Figure 1). Following FESS, one new case of post-operative nasolacrimal duct dehiscence was detected (Figure 2), probably due to the faulty surgical technique of uncinectomy. It healed in due course and thus required no further surgical intervention. Hence, we conclude that the prevalence of nasolacrimal duct dehiscence and the incidence of nasolacrimal duct injury in our series of patients undergoing FESS are both 1.16 per cent (1 out of 86 surgical procedures).
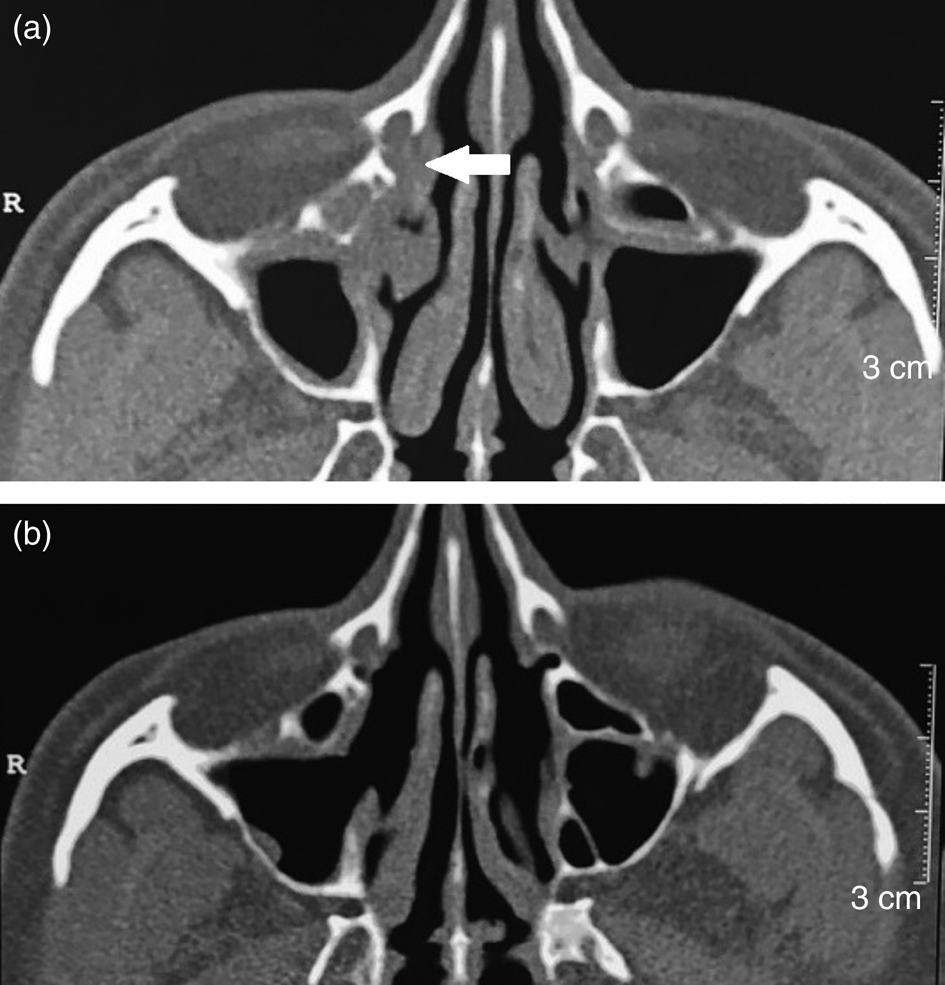
Fig. 1. Axial computed tomography images reconstructed in the bone window setting. (a) Pre-operative scan showing bony nasolacrimal duct dehiscence on the right side (white arrow) and an intact nasolacrimal duct on the left side. (b) Post-functional endoscopic sinus surgery scan shows similar findings of nasolacrimal ducts; however, the right uncinate process is not visualised and the ostia is widened. R = right
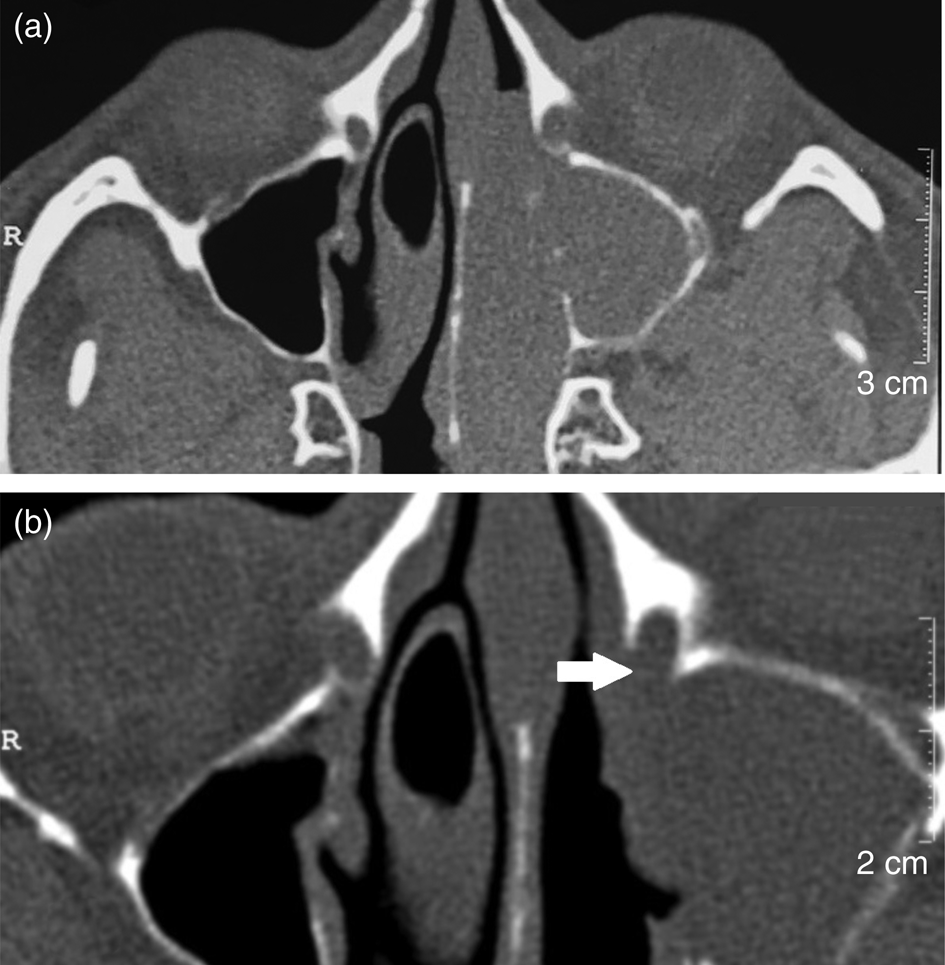
Fig. 2. Axial computed tomography images reconstructed in the bone window setting. (a) Pre-operative scan showing an intact bony nasolacrimal duct on the left side, but the bony wall of the right nasolacrimal duct is thin and surrounded by disease process. (b) Post-functional endoscopic sinus surgery image showing the absent posterior-medial wall of the left bony nasolacrimal duct (white arrow). R = right
Other complications
Other complications of FESS included one case of peri-orbital oedema, which required no intervention. No other complication of FESS was observed in this case series.
Discussion
The lacrimal apparatus is in close proximity to the uncinate process in the lateral wall of the nasal cavity. As uncinectomy is part of FESS, there is a chance that the nasolacrimal duct will become injured during FESS. The following anatomical points regarding the nasolacrimal duct deserve due consideration while performing uncinectomy in FESS.Reference Song, Jin, Kim, Huh, Kim and Kim8–Reference Zhang, Cheng, Xie, Wang, Zhang and Chen12
The lacrimal bone is situated immediately anterior to the mid-third of the uncinate process, which makes it vulnerable to injury during uncinectomy.Reference Chastain, Cooper and Sindwani13
The nasolacrimal sac is only 1–8 mm anterior to the root of the uncinate process and 0.5–1.8 mm from the natural ostium of the maxillary sinus. This makes it vulnerable to injury, not only during uncinectomy but also during the widening of the maxillary sinus ostium in FESS.Reference Cohen, Antunes and Morgenstern5
There is a dehiscence of lacrimal bone in 20 per cent of the normal population.Reference Unlu, Goktan, Aslan and Tarhan3 The lacrimal bone is very thin (0.1 mm): its thickness varies from between 100 μm and 300 μm, so it can be easily penetrated by surgical instruments.Reference Hartikainen, Aho, Seppa and Grenman14 The bony wall separating the mucous membrane of ethmoidal cells from the lacrimal bone is often missing.Reference Bolger, Parsons, Mair and Kuhn7
In the case of extensive pneumatisation, there may be pneumatisation of agger nasi cells (with anterior extension), the lacrimal bone and the frontal process of the maxilla. This leads to thinning of the bone over the lacrimal sac and duct, posing a risk of injury.Reference Bolger, Parsons, Mair and Kuhn7,Reference Whitnall15
It would also be pertinent to note that the bony nasolacrimal canal is not delineated during nasal endoscopy. The bony nasolacrimal canal is highly variable in size, with differences associated with age, sex and race. Moreover, the lacrimal bone may be subject to patchy erosion associated with ageing.Reference Shigeta, Takegoshi and Kikuchi16
All these factors make the nasolacrimal duct prone to injury during FESS. This also underlines the importance of the surgical technique that needs to be adopted during uncinectomy, so as to minimise the said injury.
We recorded a pre-operative dehiscence of 1.16 per cent in this study. This is markedly lower than the 20 per cent quoted by Unlu et al.Reference Unlu, Goktan, Aslan and Tarhan3 and 6.8 per cent reported by Ali et al.Reference Ali, Murphy, Wormald and Psaltis2 This reflects the prevalence of nasolacrimal duct dehiscence in the subcontinent and adds to the minimal data on this subject.
In the present study, only one case of nasolacrimal duct injury was recorded following FESS in 43 patients (86 surgical procedures). This makes the injury rate 1.16 per cent. The review of literature on this subject reveals an injury rate of up to 15 per cent for nasolacrimal duct injury in patients undergoing FESS.Reference Bolger, Parsons, Mair and Kuhn7 However, only 0.3–1.7 per cent of these cases were symptomatic.Reference Serdahl, Berris and Chole6,Reference Bolger, Parsons, Mair and Kuhn7,Reference Kennedy, Zinreich, Shaalan, Kuhn, Naclerio and Loch17,Reference Hunink, de Vries-Knoppert, Balm and Luth18 Our impressive results could be attributed to the surgical expertise of the principal investigator (GBS), an experienced rhinologist, and the cautious use of backbiting forceps while performing ‘swing door’ uncinectomy.
Interestingly, only a few studies have evaluated nasolacrimal duct injury in FESS. The salient features of these studies are given in Table 1. Kennedy et al. (1987) for the first time reported 2 symptomatic cases of nasolacrimal duct injury while performing endoscopic middle meatus antrostomy in 117 surgical procedures.Reference Kennedy, Zinreich, Shaalan, Kuhn, Naclerio and Loch17 Later, Serdahl et al. (1990) reported the treatment of eight cases of nasolacrimal duct injury by dacryocystorhinostomy.Reference Serdahl, Berris and Chole6 Serdahl, an ophthalmologist, analysed these cases by Jones I and Jones II tests. All these cases were referred to him, and thus the exact sample size is not available. Thereafter, Bolger et al. (1992) reported 7 cases of nasolacrimal duct injury in 46 FESS operations (sample size of 24 patients).Reference Bolger, Parsons, Mair and Kuhn7 This was a prospective study and used fluorescein dye to detect the injury. Later, Unlu et al. (2001), in a prospective study comprising 31 patients, reported 53.2 per cent dehiscence using active transport dacryocystography. None of their patients were symptomatic.Reference Unlu, Goktan, Aslan and Tarhan3 Nasolacrimal duct injury has also been reported by Saengpanich et al. (2001) in microscopic sinus surgery.Reference Saengpanich, Kerekhanjanarong, Chochaipanichnon and Supiyaphun19 In that study, only 1 out of 32 patients had nasolacrimal duct injury, and that too was asymptomatic. It is important to note that none of these studies used radiology for the evaluation of the nasolacrimal duct.
Table 1. Synopsis: studies on nasolacrimal duct injury following FESS

FESS = functional endoscopic sinus surgery; NLD = nasolacrimal duct; N/A = not applicable
Radiological evaluation of the nasolacrimal duct has been reported in the medical literature.Reference Takahashi, Kakizaki and Nakano20–Reference Aggarwal, Sharma, Das and Singh23 However, in an extensive internet search using PubMed and Medline services, we could find only one study on the radiological evaluation of nasolacrimal duct injury after FESS. In this retrospective study by Ali et al., comprising 63 patients, a pre-operative nasolacrimal duct dehiscence rate of 6.8 per cent and a post-operative dehiscence rate of 3.3 per cent (4 patients) were recorded for 118 surgical procedures.Reference Ali, Murphy, Wormald and Psaltis2 Out of these four patients, two had symptomatic epiphora, one of which required dacryocystorhinostomy. One of the important drawbacks of this study is the non-interpretation of nasolacrimal duct injury by the radiologists. In contrast, the present study is prospective in nature with the active involvement of a radiologist who is well conversant with the reporting of nasolacrimal duct dehiscence and lamina papyracea anatomy. This is in the best interests of patients and would also act as a safeguard against medicolegal litigation.
The technique of conventional cannulation dacryocystography is invasive, requiring local anaesthesia, cannulation, dilatation of the lacrimal punctum and injection of contrast material. There is also a risk of iatrogenic trauma or scarring of the lacrimal apparatus. The technique also requires co-operation from the patient.Reference Zinreich, Miller, Freeman, Glorioso and Rosenbaum24,Reference Weber, Rodriguez-DeVelasquez, Lucarelli and Cheng25 In contrast, radiological evaluation of the nasolacrimal duct is a simple and non-invasive method. Moreover, pre-operative dehiscence detected in this way guides the surgeon to carry out uncinectomy with caution, so as to prevent inadvertent injury to the nasolacrimal duct.
Modern radiological evaluation of the nasolacrimal duct apparatus involves the use of topical instillation of contrast material or saline with CT or magnetic resonance imaging (MRI).Reference Caldemeyer, Stockberger and Broderick26,Reference Rubin, Bilyk, Shore, Sutula and Cheng27 We believe that this technique is more beneficial in cases of epiphora, as it evaluates the physiology of the nasolacrimal duct apparatus. Since 1990, MRI has been used as an adjunctive diagnostic test for evaluating the nasolacrimal system. When combined with a contrast agent, it allows very fine resolution of soft tissue structures within and surrounding the nasolacrimal system.Reference Goldberg, Heinz and Chiu28 However, it is expensive, it has poor ability to image bony structures (not conducive to FESS), and there can be artefacts from the nearby ethmoidal cells. Magnetic resonance imaging is also susceptible to movement artefacts because of the relatively long acquisition times required.Reference Dutton, White, Cohen, Mercandetti and Brazzo29 Moreover, magnetic resonance dacryocystography visualises the smaller draining structures inconsistently.Reference Caldemeyer, Stockberger and Broderick26 Hence, it is not currently recommended for routine use.Reference Dutton, White, Cohen, Mercandetti and Brazzo29
Some may find the irradiation dose absorbed by the eye lens in spiral CT to be high (24.5 mGy, as compared with 1.2 mGy for digital subtraction dacryocystography), but it is still well within the prescribed radiological clinical limits (permissible dose: 0.5–2 Gy).Reference Zammit-Maempel, Chadwick and Willis30 Technically, the recommended radiation dose to the lens is 150 mSv annually. A CT of the paranasal sinuses generates only 5 mSv of radiation; thus, multiple scans pose no radiation hazard to the patients and can be conducted safely.Reference Rehani, Vano, Ciraj-Bjelac and Kleimen31
There are caveats to this study. The study cohort represents a population referred to a single tertiary care teaching hospital. Thus, the data recorded may not be representative of the general population. In addition, this study was not randomised and the results were not ascertained blindly. Observational studies such as these are also subject to potential biases (e.g. selection bias) and confounding. Further, the results might have been influenced by the expertise of the operating surgeon (GBS), a senior faculty member with considerable experience in FESS. An additional study limitation is the sole employment of ‘swing door’ uncinectomy. Last but not least, the study fails to compare the radiological technique versus conventional dacryocystography in the assessment of nasolacrimal duct injury.
• This prospective study highlights the importance of radiology in diagnosing nasolacrimal duct injury in functional endoscopic sinus surgery (FESS)
• This subject is seldom researched in medical literature
• Pre- and post-FESS computed tomography scans of 50 chronic rhinosinusitis patients were evaluated for nasolacrimal duct injury
• The minimal incidence of nasolacrimal duct injury using the ‘swing door’ uncinectomy technique in FESS was 1.16 per cent, with no symptomatic cases
• The regional prevalence of nasolacrimal duct dehiscence was 1.16 per cent
• Radiology is recommended as an excellent investigative tool to diagnose nasolacrimal duct injury following FESS
The true strength of this study lies in its prospective nature. This eliminates the shortcomings of a retrospective study: incomplete and inaccurate clinical data, and a poor follow-up record. This study amalgamates the realities of clinical practice and the rigours of scientific analysis, and thus further adds to the sparse medical literature on this subject. The true value of this study in the context of existing literature is the evaluation of nasolacrimal duct injury by non-invasive radiology in a prospective study design, hitherto unreported.
Conclusion
This academic study underlines the importance of radiology in the diagnosis of nasolacrimal duct injury. Hence, the technique described can be used to diagnose symptomatic cases of nasolacrimal duct injury following FESS. We recorded a regional prevalence of 1.16 per cent for nasolacrimal duct dehiscence. The study also highlights the low rate of nasolacrimal duct injury (1.16 per cent) in FESS using ‘swing door’ uncinectomy.
Competing interests
None declared





