I hear a lot of people saying they can’t wait for things to go back to normal … I hope to hell nothing goes back to the way it was before, we need better.
—Julie Garreau, Program Director, Cheyenne River Youth Project, Hoover Reference Airhihenbuwa2020The first large-scale COVID-19 outbreak in a Native American community originated from a large church gathering around March 7, 2020, in the small community of Chilchinbeto, Arizona, on the Navajo Nation (Allen Reference Allen2020).Footnote 1 The Navajo Nation responded to the COVID-19 outbreak by issuing a state of emergency and closing tribal offices and businesses in an effort to stop the spread of COVID-19 in their nation (Navajo-Hopi Observer News 2020). Through spring and summer, new cases of the coronavirus began to emerge in other Native nations across the United States. But the Navajo Nation remained the epicenter for COVID-19 in the United States and by May 2020 they had more per capita cases than the state of New York (Stoney Reference Airhihenbuwa2020). By August 2020, the CDC reported that Native Americans had 3.5 times more COVID-19 cases than White Americans and hospitalization rates that were five times that of White Americans (Centers for Disease Control and Prevention Reference Airhihenbuwa2020; Raifman and Raifman Reference Airhihenbuwa2020; Hatcher Reference Airhihenbuwa2020) with the majority of cases in the southwestern United States (Indian Health Service Reference Airhihenbuwa2020a).
The world’s largest outbreak of the SARS-CoV-2 virus, commonly referred to as coronavirus disease 2019 (COVID-19), has amplified longstanding racial and class inequalities that impact all aspects of American life. For Native American communities across the United States, long-standing health and economic inequalities have made them particularly vulnerable to COVID-19 infection and spread. The history of colonization and policy neglect by federal and state governments compound the effects of COVID-19 on Native peoples, making them particularly susceptible to the dark outcomes associated with the virus. This multi-generational political marginalization helps us understand why COVID-19 has been so devastating for Native American communities.
In this paper, we use data from a variety of sources, including innovative data on COVID-19 cases collected by Indian Country Today, to examine both Native American community-level and state-contextual factors associated with COVID-19 spread across Native nations. We find that state-level partisanship is associated with COVID-19 spread: Native nations in Republican states experience higher COVID-19 infection rates, as do states with higher ratios of Trump voters in their borders. We also find that measures of political and policy marginalization, including the absence of household plumbing and culturally relevant public health information, helped fuel the spread of COVID-19 in Native nations. The prevalence of non-Native American visitors onto tribal lands also contributed to COVID-19 spread. Our findings accord with existing scholarship on Native and health politics in the U.S. federalist system more broadly, and we advance empirics and theory in both fields.
Theories of Health Politics within Federalism and Native American Politics
We argue that the spread of COVID-19 in Native nations has been conditioned by longstanding political neglect and marginalization that has compounded over time. Native American health outcomes are shaped by multiple layers of inequality. In many ways, the devastating outcomes associated with COVID-19 are nothing new for tribes: non-Native governments have pursued policies that have imperiled Native health and well-being for centuries.
As we examine the politics behind COVID-19’s spread in Native nations, we reflect on insights from the literatures on health politics within U.S. federalism and from Native American politics. These literatures provide a foundation for our expectations and the motivation for our research design. The extant literature led us to expect that federal and state COVID-19 policies reflect party politics and not the needs of marginalized groups such as Native Americans. Existing research also led us to anticipate finding underinvestment in health infrastructure and culturally appropriate health information to serve Native nations would be contributing factors to COVID-19 cases for Native Americans. Finally, the Native American politics literature provides a basis to expect that the concerns of Native nations are largely ignored by both leaders and constituents outside of tribal lands. This we believe will be manifested by a correlation between the presence of non-Native visitors to tribal lands and COVID-19 outcomes. This may imply that non-Native Americans may act with little awareness or concern for how their behaviors may endanger Native lives.
Federalism, U.S. Health Care Policy, and Inequality
Health politics scholarship shows us that when responsibility for health policy is spread across the federal and state governments, healthcare inequalities are exacerbated. State health policies have gaps and inconsistencies that hit vulnerable populations hard (Campbell Reference Campbell2014). States with racially diverse populations unfortunately have a track record of underinvesting in healthcare overall and in communities of color in particular (Huberfeld, Gordon, and Jones Reference Airhihenbuwa2020). States have an important role in shaping health policy, and increasingly, party politics predict what those policies will be (Grumbach Reference Grumbach2018). Most recently, state politics has limited the reach of the Affordable Care Act (ACA) by limiting the application of tools available in the law, such as expansion of Medicaid (Béland, Rocco, and Waddan Reference Airhihenbuwa2020; Rocco, Keller, and Kelly Reference Airhihenbuwa2020). State-level ACA responses are racialized political choices that increase health disparities (Michener Reference Michener2020), a type of politics that flourishes at the confluence of racially disproportionate needs and decentralization (Michener Reference Michener2019). Disparate state-level health policies extend well beyond ACA implementation: in some states, a bundle of policies contribute to lower life expectancies (Montez et al. Reference Montez, Beckfield, Cooney, Grumbach, Hayward, Koytak, Woolf and Zajacova2020). Policies that undergird health inequality are not wholly unique to state-level health politics. In fact, Bailey et al. (Reference Airhihenbuwa2020) document that structural racism and underinvestment in federal health policy also drive health inequalities. Nor are these dynamics unique to health policy and outcomes. Miller (Reference Miller2015) notes that many of the features of decentralized health policy that exacerbate racial inequalities are also present in criminal justice policy.
These insights inform our work, and our analysis documents that comparable mechanisms have harmful effects on Native nations. There is surprisingly limited overlap between the literature on Native American politics and the research on contemporary health politics that is refracted through U.S. federalism. We hope to help bridge that gap in our work, which we believe can provide a path for scholars to work across these related but often isolated literatures.
Neglect and Marginalization as a Cause of COVID-19 Spread in Native Communities
There are 6.9 million American Indians and Alaska Natives in the United States and 574 federally-recognized Native nations (U.S. Census Bureau 2019). Native nations are sovereign governments that vary in size, geographic location, economies, and government structure. Likewise, all 574 Native nations vary by culture, language, and religion. Although tribal homelands once spanned across all fifty states, today Native nations have landholdings in thirty-four states, encompassing 56.2 million acres held in trust by the U.S. government and another 43 million acres in Alaska under the Alaska Native Land Claim Settlement Act.
Native nations are sovereign and therefore have distinct relationships with other governments. The federal government is legally defined as a trustee of Native nations and has a responsibility to provide social services, land, and to recognize the inherent sovereignty of Native nations (Cohen Reference Cohen and Cohen1960). Wilkins and Stark (Reference Wilkins and Stark2017) remind us that Native Americans are citizens of “extra constitutional nations.” Practice does not always match law, of course, and federal policies have slowly incorporated Native nations into the U.S. political process. This reality is key to our theory, as the slow and uneven incorporation of Native nations into the U.S. political process is a strong example of the marginalization that Native American communities continue to experience in the United States.
Nominally, state governments lack direct authority over Native nations. In practice, state policy impacts Native nations through direct and indirect mechanisms (Hiraldo Reference Airhihenbuwa2020; Kessler-Mata Reference Kessler-Mata2017; Steinman Reference Steinman2005; Witmer, Johnson, and Boehmke Reference Witmer, Johnson and Boehmke2014). Furthermore, states have worked consistently to suppress Native American voting rights, which has limited Native American political influence on both state and national policies (McCool, Olson, and Robinson Reference McCool, Olson and Robinson2007; Schroedel and Aslanian Reference Schroedel and Aslanian2015).
Several bipartisan federal commissions have documented the abrogation of Native American treaty rights and the overall marginalization of Native peoples and nations. In 2003, the U.S. Commission on Civil Rights examined congressional funding and federal agency support of Native American programs documented in A Quiet Crisis: Federal Funding and Unmet Needs in Indian Country. That report concluded the following:
A quiet crisis is occurring in Indian Country. Whether intentional or not, the government is failing to live up to its trust responsibility to Native peoples. The federal government undertook a legal and moral obligation to make up for what had been taken from Native Americans and to ensure their well-being … Efforts to bring Native Americans up to the standards of other Americans have failed in part because of a lack of sustained funding. The failure manifests itself in massive and escalating unmet needs in areas documented in this report and numerous others. The disparities in services show evidence of discrimination and denial of equal protection of the laws.
(U.S. Commission on Civil Rights 2003; 110)In 2018, the U.S. Commission on Civil Rights updated their assessment, finding—at best—only minor improvements. In some policy domains, they documented the backslide of federal support for programs that support Native wellbeing. Similar to the 2003 report, the U.S. Commission on Civil Rights concluded that the federal government has failed to live up to their trust responsibility to Native nations and their people. They noted the following:
Due at least in part to the failure of the federal government to adequately address the wellbeing of Native Americans over the last two centuries, Native Americans continue to rank near the bottom of all Americans in terms of health, education, and employment. Many Native Americans face unique challenges and harsh living conditions resulting from the United States having removed their tribes to locations without access to adequate resources and basic infrastructure upon which their tribal governments can foster thriving communities … The broken treaties have left many reservations without adequate access to clean water, plumbing, electricity, internet, cellular service, roads, public transportation, housing, hospitals, and schools.
(U.S. Commission on Civil Rights 2018; 1).In sum, these reports demonstrate that the vast inequalities present in Native American communities are known, not new and have been perpetuated by U.S. policy over time. Existing structural inequalities developed over centuries of political neglect and marginalization helped fuel the spread of COVID-19 in Native nations.
Centuries of Devastation: Health, Unemployment, Poverty, and Policy in Native Nations
In this section, we illustrate five layers of inequality. First, we document the historic and continuing federal policies that imperil Native health outcomes. Next, we document the effects of federal and state failures to address the lack of plumbing on tribal lands and the lack of culturally responsive health information on health outcomes for tribal communities. We then examine how non-Native Americans who travel onto tribal lands—in a context where federal policy impairs tribal governments’ ability to regulate these visitors when they are on tribal lands—contribute to the spread of illness. Finally, we demonstrate the powerful role of partisanship to health outcomes for tribes. In states where Republicans hold power—and where, often, responses to COVID-19 have ranged from casual to callous—there are tremendous risks to Native American health.
Health Politics and Native Americans
Native Americans are disproportionately affected by high rates of poverty, unemployment, and health disparities resulting from centuries of federal and state policies that have harmed Native peoples and neglected their wellbeing. Structural inequities like deficient infrastructure, food insecurity, a lack of internet access, trauma, and health interventions not adapted to local context have been well documented and continue to plague Native nations today (Fortuna et al. Reference Fortuna, Tolou-Shams, Robles-Ramamurthy and Porche2020; Graves et al. Reference Graves, Mackelprang, Amiri and Abshire2020; Hoover Reference Airhihenbuwa2020; Metzl, Maybank, and De Maio Reference Airhihenbuwa2020; Rodriguez-Lonebear et al. Reference Rodriguez-Lonebear, Barceló, Akee and Carroll2020).
Health epidemics are unfortunately not new for Native nations. In many ways, the coronavirus is a repeat of prior disease outbreaks on tribal lands caused by structural inequalities fueled by generations of colonization. In fact, several scholars have argued that colonization is the largest health epidemic that has led to the greatest loss of Indigenous life across the Americas (Estes Reference Airhihenbuwa2020; Fulton et al. Reference Fulton, Maestas, Maisel and Stone2006; Kubik, Bourassa, and Hampton Reference Kubik, Bourassa and Hampton2009; McKay, Vinyeta, and Norgaard Reference Airhihenbuwa2020; Saul, Thompson, and Hardy Reference Saul, Thompson and Hardy2021; Sherwood Reference Sherwood2013). For example, 90% of Indigenous life was lost across the Americas during the first century of European contact and death was incited by disease, starvation, and extreme poverty, all of which continue to ravage Native communities at disproportionate rates today (Jones Reference Jones2006; Newson Reference Newson1993; Snow and Lanphear Reference Snow and Lanphear1988; Stannard Reference Stannard1993).
Native American communities have also been disproportionately affected during other more traditionally defined health epidemics. During the influenza outbreak of 1918–1919, nearly 25% of Native Americans caught the flu (Kakol, Upson, and Sood Reference Airhihenbuwa2020) and were four times more likely to die from influenza than individuals living in urban areas (Centers for Disease Control and Prevention 2009). Similarly, in 1993, the first victims of the hantavirus outbreak in the southwestern United States were Navajo. Reflecting the racialization of health inequalities facing tribes, news agencies stoked fears of the unknown virus, commonly referring to it as the “Navajo flu” (Centers for Disease Control and Prevention 2020b; Pressley Reference Pressley1993). During the 2009 H1N1 outbreak, American Indian and Alaska Natives’ death rates were four times greater than all other racial and ethnic groups combined in states with high Native populations (Centers for Disease Control and Prevention 2009; Galarce, Minsky, and Viswanath Reference Galarce, Minsky and Viswanath2011; Kakol, Upson, and Sood Reference Airhihenbuwa2020). Research has documented that poverty and poor living conditions in Native communities helped fuel the spread of H1N1. Beyond health pandemics and epidemics, poverty has been consistently associated with negative health disparities in Native communities and overall increased incidences of pneumonia and annual flu (Jones Reference Jones2006; Sarche and Spicer Reference Sarche and Spicer2008). Housing conditions also have a well-documented impact on Native American health vulnerabilities. In fact, nearly 13% of Native American households in Native nations lack safe water and many others lack solid waste disposal and sewers (Indian Health Service Reference Airhihenbuwa2020b).
Access to quality healthcare has long been a challenge for Native American communities and also contributes to negative health outcomes. The right to quality healthcare is a treaty right for Native nations, codified in the Snyder Act of 1921 and Indian Health Care Improvement Act of 1976 (Indian Health Service 2013; U.S. Commission on Civil Rights 2003). Originally, healthcare for Native peoples was administered through the Department of War until this responsibility was transferred to the Department of the Interior in 1849. In 1955, the Department of the Interior transferred the oversight of Native American healthcare to the Public Health Service (today housed under Health and Human Services) and created the Indian Health Service (IHS) department (Bergman et al. Reference Bergman, Grossman, Erdrich, Todd and Forquera1999).
Underfunding of the IHS and the lack of large-scale political will to provide quality healthcare to Native Americans have been a consistent feature of federal policy (Bergman et al. Reference Bergman, Grossman, Erdrich, Todd and Forquera1999; Warne and Frizzell Reference Warne and Frizzell2014). IHS annual per capita healthcare spending for Native Americans has generally lagged far behind per capita spending for Medicare, the Bureau of Prisons, and the Veterans’ Administration (Smedley, Stith, and Nelson Reference Smedley, Stith and Nelson2003). The IHS is only funded at roughly 60% of total need (Trahant Reference Trahant2018). In 2019, for example, per capita spending for American Indian healthcare was $3,943 (HHS Division News 2020) compared to U.S. average per capita spending of over $11,500 (Martin et al. Reference Martin, Hartman, Lassman and Catlin2021). This lack of investment directly impacts the infrastructure available to address health pandemics like COVID-19.
Consequently, the care provided by the IHS has been neglectful, harmful, and inadequate (Dillingham Reference Dillingham1977; Lawrence Reference Lawrence2000; Roubideaux Reference Roubideaux2002). Today, one of the consequences of these structural features of federal Indian policy neglect is that 25% of American Indians and Alaska Natives die before the age of 45, compared to 8% of the rest of the U.S. population (Indian Health Service 2014).
In the face of structural inequalities related to healthcare and persistent poverty, Native nations are actively working to combat these conditions through self-governance. Since the passage of the Indian Self-Determination and Education Assistance Act of 1975, Native nations have been working to exercise self-governance powers over the systems that structure the well-being of their people, including healthcare, economic development, and more (Deloria and Lytle Reference Deloria and Lytle1984; Evans Reference Evans2011).
In practice, however, the federal government has failed to live up to treaty obligations for Native nations. The history of neglect and marginalization of Native nations by the federal government has been more compounded and pronounced during the COVID-19 pandemic. The federal response on tribal lands has lacked clear direction and leadership. Aid packages were trapped in bureaucratic limbo because federal agencies failed to coordinate (Cancryn Reference Cancryn2020). Scholars have detailed the “arbitrary and capricious allocation” of federal relief funds to tribal governments (Akee et al. Reference Akee, Henson, Jorgensen and Kalt2020; 2) that left Native nations “in fear of mass death” (Rodriguez-Lonebear et al. Reference Rodriguez-Lonebear, Barceló, Akee and Carroll2020; 3). Moreover, there has been great variation in how states have collaborated with Native nations to initiate response strategies. Combined, all these factors significantly impact the effects on the spread of COVID-19 in Native communities.
The Role of State Partisanship and Political Ideology
We also expect to find a relationship between statewide political partisanship and COVID-19 rates for Native communities. Although political scientists are still grappling to understand drivers of COVID-19 rates across the United States, the field has already established clear partisan effects on several important aspects of preventative measures to address the spread of the virus (Green et al. Reference Green, Edgerton, Naftel, Shoub and Cranmer2020; Grossman et al. Reference Grossman, Kim, Rexer and Thirumurthy2020; Kushner Gadarian, Goodman, and Pepinsky Reference Airhihenbuwa2020; Merkley et al. Reference Merkley, Bridgman, Loewen, Owen, Ruths and Zhilin2020). Survey data has also documented that conservative Americans are less likely to believe that the virus is real, more likely to believe that the pandemic is blown out of proportion, and as a result, not take preventative measures to slow its spread (Bump Reference Airhihenbuwa2020; Gallup, Inc 2020; Mitchell and Oliphant Reference Airhihenbuwa2020; Perez Reference Airhihenbuwa2020; Peters and Grynbaum Reference Airhihenbuwa2020; Pew Research Center 2020a, 2020b; Santucci Reference Santucci2020). For example, scholars have also found that self-identified Republicans are less likely to wear a mask in public to address infection rates of COVID-19, as are Americans who live in Republican-led states (Sanchez, Dominguez, and Vargus Reference Sanchez, Roybal and Joshi2020). These differences in preventative behavior are key, given that almost all public health experts have strongly encouraged the wearing of masks to reduce the spread of the virus.
There are also clear policy differences based on partisanship at the state and local level. For example, state partisan divides exist in public face mask mandates (Adolph et al. Reference Adolph, Amano, Bang-Jensen, Fullman, Magistro, Reinke and Wilkerson2020). As of early August Reference Airhihenbuwa2020, thirty-two U.S. states have required face coverings statewide: twenty-four are led by Democratic governors who have issued a mask mandate and only eight states run by Republicans have implemented a mask mandate, which equates to roughly one-third of all Republican-led states (Kim, Andrew, and Frpop Reference Airhihenbuwa2020). Furthermore, Democratic states were quicker to implement mask wearing policies, with half of the Democratic-led states having mandates in place by March Reference Airhihenbuwa2020. Conversely, 75% of the eight Republican-led states waited until July to put their mandate in place.
These state-level partisan differences are consistent with and potentially in response to messages from the Republican and Democratic presidential candidates in the Reference Airhihenbuwa2020 election. On one hand, Biden-Harris, the eventual presidential ticket winners, suggested that a national mask mandate should be considered. Conversely, then-Vice President Pence drew sharp criticism for deciding to not wear a mask during a trip to the Mayo Clinic in Rochester, Minnesota, and Trump had refused to wear a mask in public himself on many occasions. The differences in messaging could possibly lead to significant partisan differences in mask wearing across the public, as well as different policies at the state level based on the party of the governor.
Given the association between partisanship and the behaviors and policy approaches to limit the spread of COVID-19, we anticipate that infection rates among Native Americans will be higher in states with a Republican governor and with higher electoral support for President Trump in 2016.
Layers of Inequality
Household Access to Running Water
Adequate access to household water remains a significant challenge for many Native American nations. Much of this crisis is due to a lack of basic infrastructure to deliver both running water and safe and clean groundwater. Additionally, water sources in many Native nations are contaminated with arsenic and uranium from mining by private firms that the federal government authorized but then monitored poorly. This has resulted in fifty-eight out of every 1,000 Native American households lacking plumbing, compared with only three out of every 1,000 white households (Roller et al. Reference Roller2019). On the Navajo Nation, an estimated 30% of the population does not have access to running water. Similarly, in Oglala Lakota County, South Dakota—home of the Oglala Lakota Indian reservation—14% of households do not have access to full plumbing (Baek Reference Baek2020).
Even in communities with running water, infrastructure to deliver clean and healthy water remains a significant challenge. For example, in June Reference Airhihenbuwa2020, during the COVID-19 pandemic, the Confederated Tribes of Warm Springs in Warm Springs, Oregon, issued a boil water notice because of water mainline cracks that posed significant health risks to residents (Kohn Reference Airhihenbuwa2020).
Running water in Native nations is in many ways a matter of state, federal, and tribal system alignment. It reflects state governments’ desire to coordinate with tribes, since the federal government has funded state water systems far more than tribal water systems (Rodriguez-Lonebear et al. Reference Rodriguez-Lonebear, Barceló, Akee and Carroll2020, Haider and Teodoro Reference Airhihenbuwa2020). Access to water in Native American communities has increased over time, but federal support for safe water systems in Native communities has been slow and stalled by lack of funding. On the Navajo Nation alone, it is expected to cost $200 million to provide the most basic water and sanitation access.
Overall, access to water has become critical to advancing public health recommendations to stop the spread of COVID-19 through handwashing and other good sanitation practices. Research has documented that disparities in access to safe drinking water are associated with larger health disparities and are responsible for community spread during past pandemics (Balazs and Ray Reference Balazs and Ray2014; Eggers et al. Reference Eggers2018; Pollock et al. Reference Pollock, Sagan, Oakley, Fontaine and Poffenroth2012). Rodriguez-Lonebear et al. (Reference Rodriguez-Lonebear, Barceló, Akee and Carroll2020) found a correlation between COVID-19 spread and lack of water access in Native American communities and this mirrors findings in developing countries (Corburn et al. Reference Corburn2020; Okoi and Bwawa Reference Airhihenbuwa2020; Senghore et al. Reference Senghore2020). Given the connection between water and public health, we expect that an increase in reservation households that have access to running water will be associated with lower rates of COVID-19 in Native nations.
The Role of Language and Information in COVID-19 Outcomes
Native American health is also compromised by the shortage of health information available in Native languages. Government health agencies and news media disseminate valuable, lifesaving information about the severity of COVID-19’s health threats, as well as best approaches to reduce the spread of the virus and manage infections. When access to information is limited due to language barriers or digital divide, underrepresented communities are disproportionately harmed. Recommendations regarding behavior changes, such as the wearing of masks and social distancing, have varied across all levels of government and over time. For vulnerable communities in particular, this uneven access to information creates obstacles that could further impact infection rates.
Research finds that communication inequalities during public health crises heighten vulnerability for the public, particularly for those with higher communication barriers, lower knowledge, and lower socio-economic levels (Airhihenbuwa Reference Airhihenbuwa2020; Cassady et al. Reference Cassady, Castaneda, Ruelas, Vostrejs, Andrews and Osorio2012; Lin et al. Reference Lin, Savoia, Agboola and Viswanath2014; Viswanath and Ackerson Reference Viswanath and Ackerson2011). Moreover, research has found that individuals may be less trusting of public health information, and consequently, less willing to change their behavior when public health information is not available in their primary language (Clayman et al. Reference Clayman, Manganello, Viswanath, Hesse and Arora2010).
A large segment of the U.S. population who speak a language other than English at home includes Native people who speak over 169 Indigenous languages. Roughly 16% of Native people report speaking only a Native language and the vast majority are elders 65 years and older (Siebens and Julian Reference Siebens and Julian2011). The most common Native American languages spoken are Navajo (with over 169,000 Navajo speakers), followed by Yupik and Dakota (with each having roughly 19,000 speakers). Rodriguez-Lonebear et al.’s (Reference Rodriguez-Lonebear, Barceló, Akee and Carroll2020) analysis of COVID-19 infection rates across tribal communities early in the pandemic found that COVID-19 rates were lower in communities with larger numbers of English-only households. These authors concluded that “access to relevant information that is communicated in the language spoken by many reservation residents may play a key role in the spread of COVID-19 in some tribal communities.” We build on this finding by testing the relationship between percentage of non-English language use and Native American COVID-19 outcomes. We know there was a lag in the availability of timely and culturally-relevant public health information in Native languages for Native communities (Cheetham Reference Airhihenbuwa2020; Hatcher Reference Airhihenbuwa2020). We anticipate finding that tribal communities with a higher percentage of non-English speakers may have higher infection rates due largely to limited information being available to those communities in their Native languages.
Visitors to Native Communities and Exposure to COVID-19
One of the challenges Native American communities have faced while trying to protect their residents from COVID-19 has been the high rate of non-tribal members visiting tribal lands during the pandemic (Leonard Reference Airhihenbuwa2020). As Florey (Reference Airhihenbuwa2020) documents, COVID-19 has exposed the consequences of longstanding federal limits on tribal governments’ ability to regulate non-tribal members when they endanger health and safety on tribal lands. In normal times, Native nations have welcomed non-residents to their homelands to support economic development through casinos, for vacation, and for other purposes that support Native American economic development (Piner and Paradis Reference Piner and Paradis2004).
The context of the COVID-19 pandemic, however, led to a significant departure in policy, as many governments closed parks and limited outdoor recreation. Similarly, Native nations acted to close reservation borders or restrict access to their communities. Despite these precautions and closures, many non-Native residents continued to travel to Native communities (Hatcher Reference Airhihenbuwa2020; KRQE Media 2020; Silversmith Reference Airhihenbuwa2020). In many ways, the decision to venture into tribal lands during a pandemic reflects a lack of respect for tribal sovereignty, and exposes highly vulnerable communities to the highly contagious virus (Grimwood et al. Reference Grimwood, Muldoon and Stevens2019).
For example, the Yerington Paiute Tribe of Nevada had its bi-weekly delivery of bottled water stolen by a non-Native resident. Tribes in Nevada had their signs restricting visitation to tribal members shot with guns, and non-members violated their guidelines by forcing their way on to tribal grounds to camp (Spillmand and Kane Reference Airhihenbuwa2020). These conditions motivated many tribes across the state of Nevada to continue efforts to close their borders and limit the ability of residents to leave their community.
This context suggests that the presence of visitors to Native American communities could be associated with COVID-19 outcomes. This is a factor that likely varies significantly across tribal communities, with some tribes having greater proximity to urban counties or with high recreational demand or other appeals for non-Native visitors. Additionally, jurisdictional challenges make it more difficult for some Native nations to limit access compared to other Native nations.
Research Design and Data Discussion
To test our hypotheses related to community and state levels factors that fuel the spread of COVID-19 across Native nations, we compiled a new and original dataset from a variety of sources. These sources include Indian Country Today’s COVID-19 Native community case data, American Community Survey five-year estimates (2014–2018), Native community hospital data from the Indian Health Service health facility directory, National Indian Gaming Association, and state level public health and partisan data, including the governor’s party identification and levels of support for Donald Trump from 2016.
Our dependent variable is the sum of total positive COVID-19 cases in Native nations as gathered and confirmed by Indian Country Today. We use positive COVID-19 case counts through June 11, 2020. We use this as a cut-point because we are interested in examining the political dynamics of the pandemic during the early response phase and this cut point aligns with the full distribution of Coronavirus Aid, Relief, and Economic Security (CARES) Act funding for federally recognized tribes.
We believe this is a plausible cut-point for identifying the early phase of the COVID-19 pandemic on tribal lands. By June 11, the outbreak had been spreading in Native nations for three months. During that time, tribes were struggling to secure federal assistance for their COVID-19 responses. In May, the Department of Treasury (DoT) distributed only half of the CARES funding that Congress had allocated to tribes and distributed the balance on June 12. At this point, tribes were able to shift away from efforts to compel the federal government to fulfill its tribal commitments towards spending more time and money on tribal policymaking.
We test both community- and state-level factors that explain COVID-19 cases across 333 Native communities in the lower forty-eight United States. We include in our dataset all tribal governments with reservations or Tribal Statistical Areas designated in the Census Bureau’s American Community Survey (ACS). Our sample only includes tribes with residential housing on tribal lands. For some tribes with a very small land base, tribal lands are used for administrative offices and public facilities, and tribal members live off of tribal lands. We do exclude Indigenous communities in Alaska and Hawaii because data for these communities was not included in early iterations of the Indian Country Today dataset (Rodriguez-Lonebear et al. Reference Rodriguez-Lonebear, Barceló, Akee and Carroll2020).
We use a negative binomial regression which is ideal given that we are working with count data.Footnote 2 Our measure is a tribe-state dyad to account for tribes that cross state boundaries. This is an important nuance to our design, as several tribes including the Navajo Nation have lands that span multiple states. If a tribe in our dataset crosses state boundaries, it is coded as part of two dyads. In the average observation, sixty-one tribal members had contracted COVID-19. A complete description of this data and our measures follows.
COVID-19 Case Counts in Native America: Data Erasure and Indigenous Data Sovereignty
As we argue earlier, federal policy has impacted Native wellbeing in real and measurable ways and this was exacerbated during the COVID-19 pandemic. But federal interactions with Native nations also affects the availability (or rather absence) of data on Native American communities. There is growing critical scholarship on Indigenous erasure—where Indigenous Peoples are systematically overlooked, intentionally excluded, and “Othered” as a footnote, or treated as an “Asterisk Nation*” (Hudson et al. Reference Hudson2020; National Congress of American Indians 2012). The lack of intentionality to collect Indigenous data has led to huge disparities in the availability of timely and accurate data on Indigenous peoples and communities, especially compared to other ethnic/racial groups. This lack of data is pervasive, and the data available for research has unfortunately often been weaponized (Walter and Andersen Reference Walter and Andersen2013), necessitating the need for Indigenous Peoples to govern their own data (Kukutai, Carroll, and Walter Reference Airhihenbuwa2020; Rainie et al. Reference Rainie, Schultz, Briggs, Riggs and Palmanteer-Holder2017; Taylor and Kukutai Reference Kukutai and Taylor2016).
This context for understanding Indigenous data (or absence of) is important because in the face of such exclusion, Native nations have had to respond to data needs with innovative solutions. This includes during the COVID-19 health pandemic. During the early days of the pandemic, data on all racial and ethnic groups was a challenge, including for Native American communities. Without data, tribes were struggling to respond locally as well as to advocate for federal and state action.
To address this gap, Indian Country Today, housed at Arizona State University, developed a website and Google form to gather crowdsourced tribal data of COVID-19 cases and deaths in Indian Country (Indian Country Today 2020). According to the Indian Country Today website, data is “confirmed by tribes, tribal health clinics, urban Indian programs, the Indian Health Service, state public health agencies or the Centers for Disease Control and Prevention.” Not all data was crowd sourced, as data was also gathered from the public release of information by Native nations and also supplemented and verified by news reports. This data serves as an innovative and comprehensive grassroots effort to combat the absence of standardized Native American COVID-19 case data. Indian Country Today is one of the oldest, best-known Indigenous media outlets in the United States and beyond. Indian Country Today has taken the lead in collecting other data to combat the absence of data on Native Americans in the United States. For example, in 2018, they successfully collected data on Native American candidates for federal and state office (Evans et al. Reference Evans, Foxworth, Huyser, Macias-Mejia and Sanchez2019). Rodriguez-Lonebear et al. (Reference Rodriguez-Lonebear, Barceló, Akee and Carroll2020) have already published peer-reviewed research that uses the Indian Country Today dataset to highlight socioeconomic correlates of COVID-19 rates in Native Nations.
The efforts of Indian Country Today to collect and verify COVID-19 case outcomes in Native nations is an exercise of Indigenous Data Sovereignty. Indigenous Data Sovereignty serves Native nations and their inherent right to govern the use of their own data (Kukutai and Taylor Reference Kukutai and Taylor2016; Snipp Reference Snipp, Kikutai and Taylor2016; Rodriguez-Lonebear Reference Rodriguez-Lonebear, Kukutai and Taylor2016) and serve as a tool for tribal nations to advance Indigenous rights and interests as well as to hold the federal government accountable to its treaty obligations (Carroll et al. Reference Carroll, Rodriguez-Lonebear, Akee, Lucchesi and Richards2020). The Indian Country Today dataset represents the only comprehensive publicly available data for Native nations. We acknowledge that our dataset may be limited but is ultimately better than no data, which would result in continued Indigenous exclusion and erasure. Data collected by Indian Country Today were collected in line with best practices, including protection of identifying features of individuals who submitted data. Overall, the data collected by Indian Country Today were done to address Indigenous erasure and provide valuable data to Native communities to understand and combat this public health crisis especially in the face of neglect by state and federal governments. Given the overall approach and existing peer-reviewed publications utilizing this data (Rodriguez-Lonebear et al. Reference Rodriguez-Lonebear, Barceló, Akee and Carroll2020), we believe it is the best data available to understand COVID-19 infection rates across Native communities. We also assert that the results remain designed to benefit Indigenous Peoples collectively and to reduce harm (RDA COVID-19 Working Group Reference Airhihenbuwa2020).
All data for hard-to-reach populations comes with limitations, and our dataset is no exception.
We have done our best to account for these limitations through different modeling strategies discussed later.
Community Level Factors
To test the effects of COVID-19 spread across Native communities, we use a number of community level explanatory factors.
Water and language
Rodriguez-Lonebear et al. (Reference Rodriguez-Lonebear, Barceló, Akee and Carroll2020) noted that COVID-19 cases were more likely in areas with a higher proportion of homes lacking indoor plumbing, and COVID-19 cases were less likely in communities where greater rates of English-only language are present. The association between these two factors and COVID-19 outcomes motivates inclusion of these measures in our model. We use the percentage of Native American households in Native nations with complete plumbing and the percentage of households that speak only English. For the average observation in our dataset, 95% of households have plumbing. For the average observation, 77% of households speak only English at home. This data comes from the American Community Survey five-year estimates (2014–2018).
Non-Native American visitors
We expect that visitors from nearby populations will increase tribes’ COVID-19 rates. As one indicator of non-tribal members visiting tribal lands, we include the size of tribal casinos. We think casino size is a good measure as it gives a sound proxy for one reason that individuals visit tribal lands and we know that the presence of Native casinos is usually combined with other draws for non-Native tourists. Casino revenues are proprietary information and not available publicly, but other indicators on the of scale of casino operations are accessible. Evans et al. (Reference Evans, Dolšak, Plog and Prakash2020) compiled the square footage of all tribally-owned casinos, available from the National Indian Gaming Association at http://indiangaming.com/home/ and we include their compilation in this paper with their permission. For the average observation, tribal casinos covered 66,891 square feet.
State Contextual Factors
Partisanship. Former President Trump consistently downplayed the dangers of COVID-19, disparaged public health policies that can reduce the spread of the disease, encouraged his supporters to defy health and safety regulations, and pressured Republican governors to avoid utilizing their powers to protect public health. We expect that these behaviors endanger Native Americans. We employ two interchangeable measures to capture the influence of Trump’s message in a state. First, we consider the extent of support for Trump in the state, which we measure by percent of votes for Trump in 2016. For the average observation in our sample, 45% of state voters cast ballots for Trump in 2016. Trump directed his message not just to individuals who supported him, but to Republican governors as well. As a second measure, we identify whether a state’s governor is a Republican. Governors have a great deal of discretion over powers they can use—or not use—to contain a pandemic. Across our dataset 29% of observations are in states with a Republican governor.
State COVID-19 rates. We expect that nearby or adjacent COVID-19 rates will affect the tribes’ COVID-19 rates. Accordingly, we include the number of cases per 100,000 by June 11 in each state (Centers for Disease Control and Prevention 2020a). For the average observation, state cases were 469 per 100,000 residents.
Other Controls
Demographic controls
Native nations are not a monolith; their social and economic circumstances vary greatly. We include a variety of indicators of social and economic conditions on tribal land, drawn from the ACS. Specifically, we control for Native American population, age, and incomes by reservation. We expect that higher-income households will have lower rates of COVID-19. For the average observation, the median household income on tribal lands was $42,237. We expect more COVID-19 cases when populations are larger. For the average observation, 12,999 people live within the tribe’s lands.
We control for age, with awareness that the health and social conditions associated with age may be different on tribal lands than in the U.S. population overall. While elders are more vulnerable to COVID-19, they also are less likely to be in the workplace, schools, or other places where large groups gathered. Furthermore, risk factors for serious COVID-19 cases are higher among young- and middle-aged Native Americans than for the rest of the U.S. population. The protective effects typically associated with youth may be less relevant for Native health. For the average observation, the median age on tribal lands was thirty-six years.
For the average observation, 55% of people living within the tribe’s lands are American Indian or Alaska Native. Many tribal lands are “checkerboarded,” meaning there are private parcels of land owned by non-Native Americans within the outer boundaries of a reservation. In large part, tribal governments do not have authority over these parcels. Checkerboarding is a product of federal assimilation policy: “a mighty pulverizing engine to break up the tribal mass,” to use Theodore Roosevelt’s words. Today, checkerboarding results in an array of jurisdictional complexities (Wilkins and Stark Reference Wilkins and Stark2017). Given that checkerboarded lands are harder to govern overall, we expect poorer health outcomes where more non-Native Americans live on tribal lands.
Measurement controls
We include four measures to account for possible underreporting of COVID-19 cases on some tribal lands. We consider whether the tribe operates any health facilities or whether Indian Health Service (IHS) operates any health facilities on the tribe’s lands. In either circumstance, we expect that health care services are more easily accessible. As a result, we expect testing and thus the identification of COVID-19 cases will be higher. Such a facility was present for 77% of observations (Indian Health Service n.d.).
We expect that Native American COVID-19 cases might be under-detected because of racial misclassification. In some states, health agencies and health providers have a history of misclassifying Native American patients as Hispanic White, Non-Hispanic white, or Black. To account for the fact that some states are more likely to miscode Native American cases, we include the IHS’s state-level adjustment factors reported in “Adjusting for Miscoding of Indian Race on State Death Certificates” (Indian Health Service 1996). For a nationwide measure of racial misclassification in health data, the most reliable information comes from death certificates, and we expect that the forces driving this misclassification are also present in the treatment of patients who survive. For the average observation, IHS advises an adjustment rate of 1.24. This means that for every one hundred Native American deaths recorded in the state, an additional twenty-four Native American deaths are miscoded as another race. In some states, the adjustment rate is 2.5.
We consider whether some tribes are more or less likely to register COVID-19 cases on Indian Country Today’s COVID-19 database. One indicator is whether the tribe is part of a health policy network more closely attached to Indian Country Today. Perhaps tribes that are in close proximity to Indian Country Today are more likely to know about this crowd-sourced dataset and spread word in their professional networks. Indian Country Today is headquartered in Phoenix, so we control for whether a tribe is a member of the Phoenix Indian Health Board. The Phoenix Indian Health Board is a key organization connecting tribal health professionals in the Southwest; 12% of observations are from members of the Phoenix Indian Health Board.
Another indicator is whether a tribal government is recognized by a state government but not the federal government. State-recognized tribes have less access to national networks of tribal health professionals that are facilitated by federal agencies. Because state-recognized tribes are less networked, perhaps they are less aware of the crowd-sourced dataset. ACS notes whether a tribe is state or federally recognized; 10% of observations are of state-recognized tribes.
Results
We find striking effects from state and national politics on COVID-19’s spread, with statistically significant effects for both party of governor and Trump vote share at the state level. Due to high correlation between party of governor and electorate support for President Trump, we estimate and present two separate models that are identical other than the presence of these correlated measures. As shown in table 1, tribes have more COVID-19 cases in states with a Republican governor (Model 2) and where a greater share of people voted for Trump in 2016 (Model 1). In short, the effects of a governor’s party and Trump support on COVID-19 cases are interchangeable. Trump’s reaction to COVID-19 was unresponsive and slow, often prioritizing politics over public health. This encouraged Trump supporters to buck health safety measures and pressured governors to do the same. In states where Republican leaders promote recklessness, we find that Native Americans are more likely to fall ill.
Table 1 Model predicting # of COVID-19 cases of tribal members across Native nations by June 11, 2020
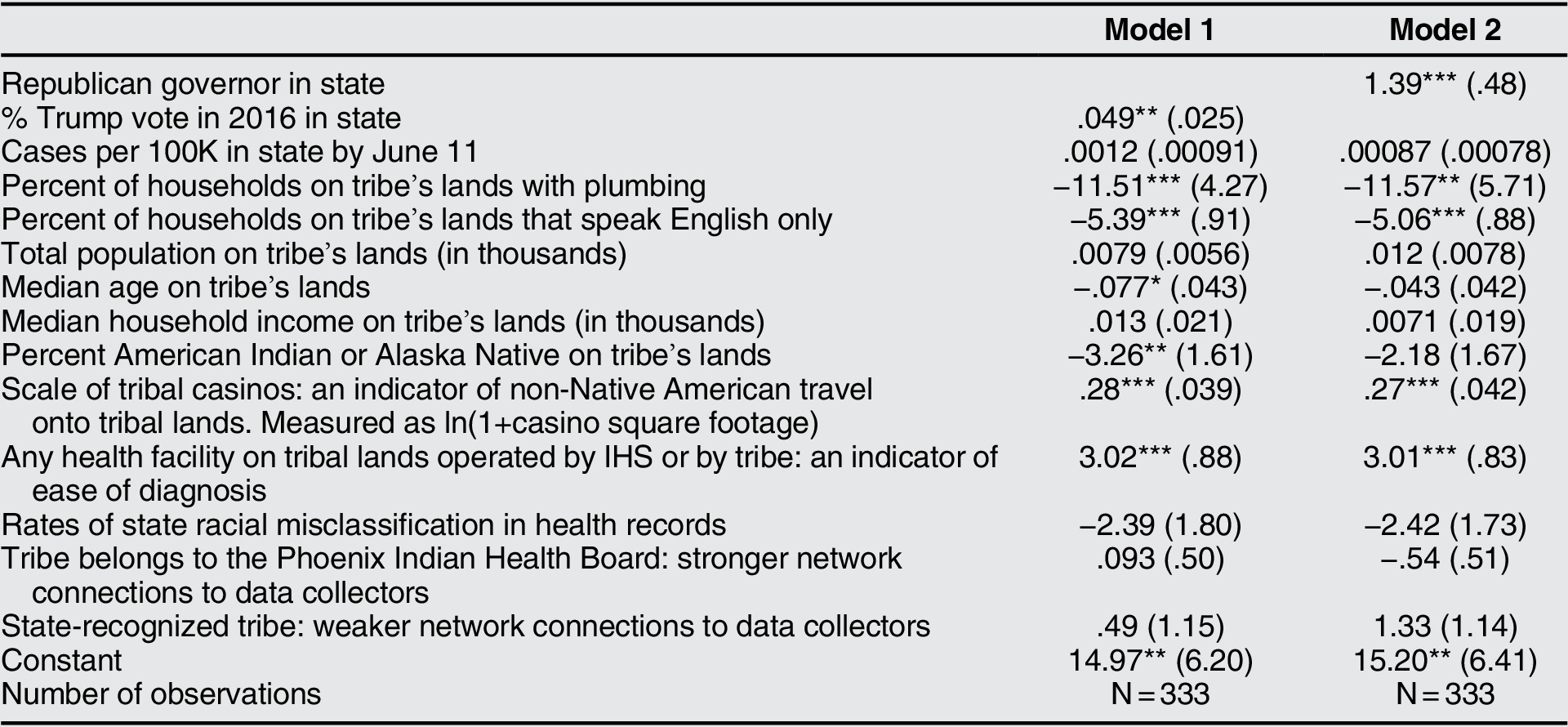
Notes: Negative binomial regression. Robust standard errors in parentheses. *p < 0.10, **p < 0.05, ***p < 0.01.
We find that the long-term political marginalization of Native Americans affects COVID-19’s spread as well. Where there is less plumbing availability, there are more COVID-19 cases. For decades, the federal government and state governments have known about utility shortfalls on Native lands and opted to not act. This is a strong barometer of political marginalization. Furthermore, where rates of fluency in English are lower, there are more COVID-19 cases for tribes. When federal agencies and states lack the ability or desire to provide health information in Native languages, it also reflects an overall culture of political marginalization for Native American communities.
In situations that bring more non-Native Americans onto tribal lands, we find there are more COVID-19 cases among tribal members. Specifically, larger tribal casinos lead to statistically significant increases in tribal COVID-19 cases. Casino size is of course only one indicator of non-Native Americans travel onto tribal lands. We expect other mechanisms and industries that increase travel would matter, too, but do not have the capacity to collect more direct measures of this phenomenon.
We find that tribes have more COVID-19 cases when more non-Native Americans live amongst tribal members, and the effect is statistically significant in one model. Non-Native neighbors may facilitate disease interface between tribal members and outside populations. Additionally, where populations are older, there are fewer COVID-19 cases among tribal members, and the effect is statistically significant in Model 1. As we note in a prior section, we suspect that overall social and health experiences associated with age on tribal lands may differ from the rest of the country.
Among our other control variables, we find positive and statistically significant effects from health facilities on tribal lands. This result conforms with our expectations: easier access to health care facilities results in more diagnoses of COVID-19 cases in Native communities.
Substantive Effects
In figure 1, we translate regression coefficients into predicted number of COVID cases. We find striking effects, especially considering that we measure cases up through June 11, Reference Airhihenbuwa2020, and that the median tribal population is 843 members. For dichotomous variables, we examine whether or not a condition existed. For continuous variables, we operationalize “very high” levels as the ninetieth percentile of the distribution, “very low” levels as the tenth percentile of the distribution, and hold most continuous control variables at their mean. Because of long tails in their distributions, we hold at their median the casino square footage, population on tribal lands, and percent of population on tribal lands that is Native American.
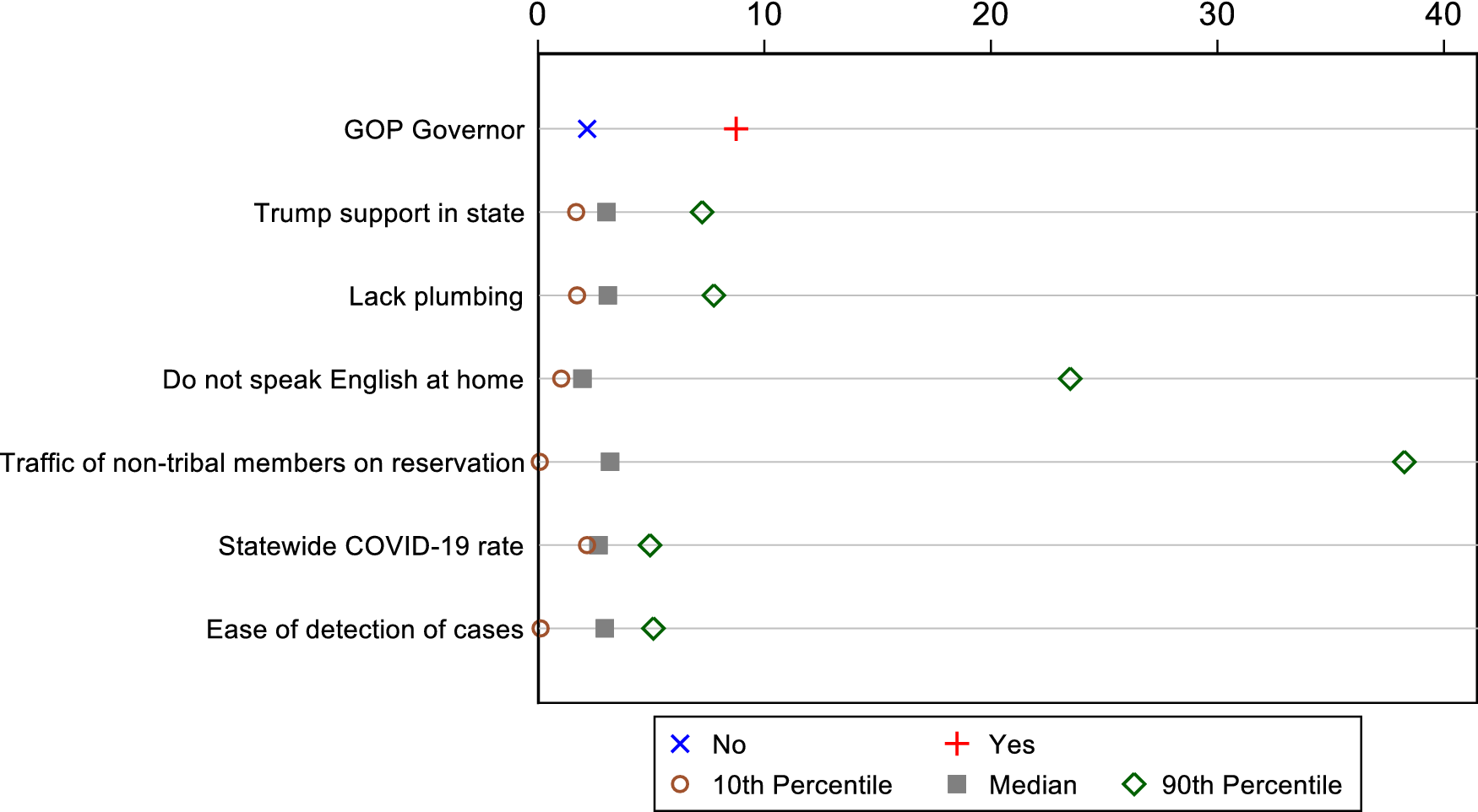
Figure 1 Predicted number of COVID cases for the tribe
First, we find that state politics matter. The model predicts 2.2 cases for a tribe in a state with a Democratic governor. Cases roughly quadruple—to 8.3—under a Republican governor. Our results are parallel for statewide Trump support in 2016. When statewide Trump support was very low, the predicted number of cases is 1.7. We find that when Trump support is very high, cases roughly quadruple, to 7.3 cases.
The absence of plumbing has comparable effects. When the frequency of households that lack plumbing is very low, we expect 1.7 cases. When the frequency of households that lack plumbing is very high, we predict 7.8 cases.
We think our findings present a clarion call for language-appropriate, culturally competent public health outreach. When it is less common for tribal members to speak English, cases skyrocket. When the frequency of speaking other languages is very low, we expect 1 case. When the frequency of speaking languages other than English is very high, the effects are devastating: we predict 23.5 cases.
The presence of non-Native Americans on tribal lands has dramatic effects. We expect 0.1 cases when that presence is very low—specifically, when tribes are very low both in their casino size and the share of population on tribal lands that is not Native American. We expect 38.3 cases where the presence of non-Native Americans is very high.
Interestingly, statewide COVID rates have limited direct effects on cases on tribal lands. Very low statewide rates are associated with 2.2 cases; when statewide rates are very high, we expect 5.0 cases.
Finally, we note troubling effects of the ease of detecting COVID-19 cases. Simply put, where detection is much harder, tribes were likely to be experiencing an outbreak and not know it. When capacity for detection is very low, a tribe may believe it has 0.1 cases. But in reality, cases may be more extensive: when capacity to detect is very high, we expect tribes to observe 5.1 cases. We measure this capacity both by the presence a health facility on tribal lands and by our indicator of state accuracy in identifying Native American patients. In brief, shortcomings of public health systems may have masked outbreaks entirely.
Discussion
When the coronavirus pandemic hit the United States, many Native nations took swift action—in some cases, even before states. Many Native American leaders may have been unsure about how the global pandemic would unfold, but they understood the vulnerability of Native communities. Yet in many cases, Native nations were left to fend for themselves by both states and the federal government. Conflict between state governments, non-tribal citizens, and tribal governments posed a significant threat to the health of Native American communities.
Our study brings multiple literatures into the conversation. Existing work on Native American politics and the politics of health within U.S. federalism point clearly in one direction: we should expect under-provision of vital health resources to Native nations. Our findings demonstrate that this holds true in the case of COVID-19 and illustrate how inequality is further exacerbated in uncertain times. We also build on extant research that highlights the significant health effects of the lack of infrastructure, in particular access to water and plumbing.
Our findings illustrate the multifaceted nature of the federal and state governments’ historic and continuing neglect of Native American wellbeing. The federal government made a commitment to protect Native health but has failed to meet it. Federal and state governments have created conditions that make Native peoples highly vulnerable to COVID-19. These governments could provide basic health infrastructure and language-appropriate health resources. Republican leaders could adopt policies that protect Native health, with the knowledge that states’ non-tribal residents may act as disease vectors into Native communities. Some state governments have done some of these things, but too many have not.
Policy Recommendations
The following policy changes could help address the harms that we document.
Unrestricted funds : The current distribution of funds to Native nations are often restricted to specific programs, narrow categories, and specific timeframes for spending. Native nations need unrestricted funds to manage distribution and spending according to their community and populations needs. For example, time restrictions on federal CARES funding for Native nations may make the spending of federal dollars difficult because of their remote locations, lack of current administrative capabilities, and general shortages of supplies throughout the country.
Provide Broadband Services: An estimated 35% of individuals living on tribal lands are without broadband services. The lack of services further exacerbates the education and health gap, prohibits access to telehealth, and obstructs the acquisition of basic information on the COVID-19 pandemic (Sanchez, Roybal, and Joshi Reference Airhihenbuwa2020).
Prioritize Life Saving Equipment and PPE for Tribal Nations: Limited funding for Indian Health Services (IHS) by the U.S. government has endangered Native peoples. During early days of the pandemic, IHS reported having a limited number of ICU beds and reported having only eighty-one ventilators across the country (Cancryn Reference Airhihenbuwa2020). Tribes were also disadvantaged in trying to purchase PPE and some PPE sent to Native communities were not medical grade or were sent wrong equipment (Collman Reference Airhihenbuwa2020; Willis Reference Airhihenbuwa2020). The federal government must prioritize lifesaving equipment for Native nations and consider funding a separate stockpile for Native nations.
Investment in Infrastructure : The lack of healthy water, plumbing, electricity, broadband, and other kinds of infrastructure remain a perennial challenge that effects the health of Native people. Many tribal lands also lack safe roads and public transportation making access to resources, care, and emergency services near impossible. The federal government must prioritize investment in meaningful infrastructure for Native nations.
Investment in Education: Native American students experiences some of the nation’s highest disparities in educational attainment. Education is a significant predictor of one’s health status (Ross and Wu Reference Ross and Wu1995). The pandemic has significantly exacerbated the existing achievement gap for Native students Increased funding and support for educational services will be critical for long-term recovery.
State Support for Tribal Closures to the Public: While some states supported tribal land closures, other states governments did the opposite. Closures of tribal lands to non-tribal members were key to the reduction and control of COVID-19 cases. This recommendation also highlights that the broader public must also respect tribal sovereignty all the time, but especially when public crisis places Native people in greater harm.
Support for Long-term Economic Recovery and Development: Tribal government and business closures resulting from COVID-19 have had a devastating economic impact on Native nations (Akee et al. Reference Akee, Henson, Jorgensen and Kalt2020). Moreover, Native families, most who were financially vulnerable before the pandemic, have experienced even greater loss of employment, income, and savings (National Public Radio 2020). There needs to be long-term investment in Native nation economic development, diversification, and job creation. Significant losses in gaming revenue for some Native nations may also necessitate the renegotiation of gaming revenue sharing agreements with states. In sum, Native nations will need long-term economic relief, and this will require collaborative approaches with both federal and state governments.
Federal Legislation Affirming Tribal Governments’ Powers to Regulate Non-Members on Tribal Lands: When non-members endanger public health and safety on tribal lands, tribal governments can do very little to stop them. Federal legislation could undo case law’s limits. Tribes need the authority to require everyone to comply with tribal health and safety standards while on tribal lands (Florey Reference Airhihenbuwa2020).
Acknowledgements
The authors thank attendees of the Politics of Race, Immigration, and Ethnicity Consortium (PRIEC) virtual gathering held in May Reference Airhihenbuwa2020 for their helpful feedback. The research reported in this article was supported by the National Institute of Minority Health and Health Disparities of the National Institutes of Health under award number U54 MD004811. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.




