Pulmonary hypertension (PH) is one of the most serious complications of CHD.Reference Saleh, Shabana, El Amrousy and Zoair1 Increased left to right shunt in CHD is the principle cause of PH-related CHD. The proliferation of fibroblasts and smooth muscle cells besides the extracellular matrix deposition is the basis of pulmonary vascular remodelling that is the key factor in the pathogenesis of PH.Reference Rabinovitch2,Reference Voelkel, Gomez-Arroyo, Abbate, Bogaard and Nicolls3 Over the past years, several blood biomarkers such as B-type natriuretic peptide, N-terminal pro-B-type natriuretic peptide, endothelin-1, growth differentiation factor-15, and miRNAs have been used to access diagnosis and prognosis in patients with PH, but none of them were validated to be an ideal marker.Reference Giannakoulas, Mouratoglou, Gatzoulis and Karvounis4–Reference Abd-Rabo, El-Amrousy, El-Serogy and Zoair6
Connective tissue growth factor is another promising biomarker in PH. Connective tissue growth factor is a member of CCN (Cyr61, CTGF, and Nov) family. Connective tissue growth factor acts as a downstream mediator of transforming growth factor-β1 that is involved in the regulation of pulmonary arterial smooth muscle cell proliferation, extracellular matrix deposition, and consequently leads to pulmonary vascular remodelling.Reference Chen and Lau7,Reference Li, Hu and Jia8 Moreover, connective tissue growth factor has the effects of promoting cell mitosis, adhesion, migration, induction of extracellular matrix synthesis, and fibrosis. So, it has been used as a marker in fibroproliferative diseases, heart failure, and idiopathic pulmonary fibrosis.Reference Tahira, Fukuda and Endo9–Reference Behnes, Brueckmann and Lang11 However, the diagnostic and predictive value of plasma connective tissue growth factor in children with PH-related CHD has not been recorded.
The aim of this study was to evaluate the diagnostic and predictive value of plasma connective tissue growth factor in children with PH-related CHD and to correlate its levels with various clinical, echocardiographic, and haemodynamic parameters.
Patients and methods
This is a prospective case-controlled study that was conducted on 80 children with CHD who were recruited from those admitted at Pediatric Cardiology Unit at Tanta University hospitals during the period from January 2018 to March 2019. Forty healthy children of matched age and sex were included as a control group. The study was approved by local ethical committee of our faculty of medicine. Children were included in the study after signing a written consent by their parents.
Inclusion criteria: children aged less than 18 years with CHD with or without PH.
Exclusion criteria: neonates with PH; children with renal, hepatic, or pulmonary disease; children with genetic syndromes.
Children with CHD were divided into 2 groups:
Group I: included 40 children with CHD and PH.
Group II: included 40 children with CHD and no PH.
PH was diagnosed if mean pulmonary artery pressure was ≥25 mmHg, and pulmonary vascular resistance was ≥3 Wood unit.
The following investigations were performed to all included children:
1. Complete history taking and thorough clinical and cardiac examination.
2. Diagnostic catheterisation: Cardiac catheterisation was performed under general anaesthesia for CHD patients only to evaluate mean pulmonary artery pressure and pulmonary vascular resistance. Pulmonary blood flow, systemic blood flow, and the ratio between pulmonary blood flow and systemic blood flow were also measured using Fick method. Pulmonary vascular resistance, pulmonary blood flow, and systemic blood flow were indexed for body surface area.
3. Echocardiographic examination: using Vivid 7 and Vivid 9 ultrasound machine (GE Medical System, Horten, Norway) with 7 and 4s MHz multi-frequency transducers. M mode, Doppler, and two-dimensional modes were used for the assessment of the following:
Type of CHD
Right ventricular diameter: is estimated at the end diastole of the right ventricle in the apical four-chamber view at the mid-cavity just above the moderator band.
Right ventricular systolic function: right ventricular fractional area change was measured by two-dimensional echocardiography from the apical four-chamber view. Both right ventricular end-diastolic area and right ventricular end-systolic area were obtained. Then right ventricular fractional area change can be calculated by the equation:
Right ventricular fractional area change = right ventricular end-diastolic area – right ventricular end-systolic area / right ventricular end-diastolic area × 100.Reference DiLorenzo, Bhatt and Mercer-Rosa12
Right ventricular diastolic function: was measured through pulsed trans-tricuspid Doppler in the form of tricuspid E/A ratio where E wave represented RV relaxation and A wave represented right atrial contraction.
4. Plasma levels of connective tissue growth factor: was measured using double-antibody enzyme-linked immunosorbent assay kit supplied by SunRed catalogue No. 201-12-0147, Shanghai, China. The blood samples were collected in tubes containing EDTA after overnight fasting at 9 am then centrifuged for 15 minutes. The plasma sample was stored at −20°C till the time of analysis. The inter- and intra-assay coefficients of variation were estimated by repeated tests.
All patients with CHD were followed up for 6 months for adverse outcomes such as death or readmission. Poor prognosis is defined as the occurrence of death or readmission of the patients during the period of follow-up. PH was graded as mild, moderate, and severe according to the mean pulmonary artery pressure obtained during cardiac catheterisation. Mild PH was defined as mean pulmonary artery pressure between 26 and 40 mmHg, moderate PH if mean pulmonary artery pressure ranged between 41 and 55 mmHg, and severe PH if mean pulmonary artery pressure was more than 55 mmHg.Reference Galiè, Hoeper and Humbert13
The primary outcome was to evaluate the diagnostic value of plasma connective tissue growth factor in children with PH-related CHD. The secondary outcomes were to evaluate the predictive value of plasma connective tissue growth factor in children with PH-related CHD and to correlate plasma connective tissue growth factor levels with different clinical, echocardiographic, and haemodynamic parameters.
Statistical analysis
The sample size was calculated using a value of 0.841 for the area under the curve of the plasma connective tissue growth factor for diagnosing PH in children with CHD based on a previous study.Reference Li, Tang, Jia, Zhao, Liu and Liu14 On the basis of this calculation, we found that 36 children in each group would be needed to achieve a power of 90% with a = 0.05. Continuous variables were expressed by mean and standard deviation. Categorical variables were expressed in the form of number and percentage. Comparing the mean of the three groups was performed by using one-way analysis of variance. Comparing the means between the two groups of CHD was performed using Studentʼs t-test. Post hoc analysis was performed using Tukey test to evaluate significance between the groups. Correlation between plasma connective tissue growth factor levels and different variables was performed using Spearman correlation coefficient. Receiver operating characteristic curve was drawn to evaluate the diagnostic and predictive value of connective tissue growth factor in children with PH-related CHD at different cut-off values. The inter- and intra-assay coefficients of variation for plasma connective tissue growth factor were estimated by dividing the standard deviation by the mean and multiply it with 100. Statistical analysis of the data was performed using SPSS V. 21 (SPSS Inc. Chicago, Illinois, United States of America). P value was considered significant if less than 0.05.
Results
The study included 40 children with PH-related CHD with a mean age of 16.7 ± 5.2 months, 40 children with CHD and no PH with a mean age of 17.2 ± 4.9 months, and 40 healthy children as a control group with a mean age of 17 ± 4.8 months. There was no significant difference between the three groups as regards age, sex, or height. The weight of children with CHD was significantly lower than that of the control group. Heart rate was significantly higher in children with CHD compared to the control group. Respiratory rate, right ventricular diameter, plasma connective tissue growth factor, and mean pulmonary artery pressure were significantly higher in children with PH-related CHD compared to those with CHD only and to the control group. Nevertheless, oxygen saturation, right ventricular fractional area change, and right ventricular E/A ratio were significantly lower in children with PH-related CHD compared to those with CHD only and to the control group (Table 1).
Table 1. Demographic, clinical, laboratory, haemodynamic, and echocardiographic parameters in the studied groups

p: p value for comparison between the three studied groups
p1: p value for comparison between PH-CHD and CHD groups
p2: p value for comparison between PH-CHD and control groups
p3: p value for comparison between CHD and control groups
VSD = ventricular septal defect; ASD = atrial septal defect; PDA = patent ductus arteriosus; TGA = transposition of great arteries; AVC = atrioventricular canal; HR = heart rate; b/m = beat per minute; RR = respiratory rate; CTGF = connective tissue growth factor; PVR = pulmonary vascular resistance; WU = wood unit; Qp = pulmonary blood flow; Qs = systemic blood flow; mPAP = mean pulmonary artery pressure; RVD = right ventricular diameter; RV FAC = right ventricular fractional area change; RV = right ventricle; E/A ratio = ratio of the early (E) to late (A) ventricular filling velocities
* means significant
Six children had mild PH with mean plasma connective tissue growth factor levels of 841.3 ± 99.8, 18 children had moderate PH with mean plasma connective tissue growth factor levels of 1174.4 ± 510.6, and 16 children had severe PH with mean plasma connective tissue growth factor levels of 3252.1 ± 1274.1. There was a significant difference between the three grades as regards plasma connective tissue growth factor levels with the lowest levels in children with mild PH and the highest levels in children with severe PH (p = 0.001; Table 2).
Table 2. Plasma CTGF levels in different grades of PH in PH-CHD group

p: p value for association between different grades of PH
p1: p value for comparison between mild and moderate PH
p2: p value for comparison between mild and severe PH
p3: p value for comparison between moderate and severe PH
CTGF = connective tissue growth factor; PH = pulmonary hypertension
* means significant
There was a significant positive correlation between plasma connective tissue growth factor levels and mean pulmonary artery pressure, pulmonary vascular resistance, and right ventricular diameter. However, there was a significant negative correlation between plasma connective tissue growth factor levels and both oxygen saturation and right ventricular diastolic function (p < 0.05). There was no significant correlation between plasma connective tissue growth factor levels and age, sex, height, weight, heart rate, respiratory rate, or right ventricular fractional area change (p ≥ 0.05; Table 3).
Table 3. Correlation between plasma CTGF levels and different parameters in PH-CHD group
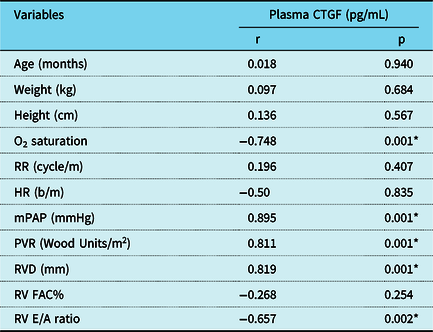
CTGF = connective tissue growth factor; kg = kilogram; HR = heart rate; b/m = beat per minute; RR = respiratory rate; mPAP = mean pulmonary artery pressure; PVR = pulmonary vascular resistance; RVD = right ventricular diameter; RV FAC = right ventricular fractional area change; RV = right ventricle; E/A ratio = ratio of the early (E) to late (A) ventricular filling velocities
* means significant
Ten patients with PH-related CHD had a poor prognosis on follow-up; 3 died while 7 were readmitted due to complications of excessive shunting such as severe heart failure. The mean plasma level of connective tissue growth factor in PH-related CHD patients with poor prognosis (3675.5 ± 1276.6) was significantly higher than those with good prognosis (1382.33 ± 840.91) with p < 0.001 (Fig. 1).

Figure 1. Plasma connective tissue growth factor levels in patients with good and poor prognosis in pulmonary hypertension-related CHD group.
At a cut-off value of ≥650 pg/mL, the sensitivity of plasma connective tissue growth factor as a diagnostic biomarker in PH-related CHD patients was 95%, the specificity was 90%, positive predictive value was 91%, negative predictive value was 94 %, and the accuracy was 92.5% (Fig. 2). While, at a cut-off value of ≥1900 pg/mL, the predictive value of plasma connective tissue growth factor for adverse outcome in PH-related CHD patients had a sensitivity 88%, specificity 83%, positive predictive value 78%, negative predictive value 91%, and accuracy of 85% (Fig. 3). The inter- and intra-assay coefficients of variation for plasma connective tissue growth factor were 6 and 2%, respectively.

Figure 2. Receiver operating characteristics curve for connective tissue growth factor to diagnose pulmonary hypertension in CHD patients.

Figure 3. Receiver operating characteristics curve for connective tissue growth factor to predict poor prognosis in pulmonary hypertension-related CHD patients.
Discussion
Currently, non-invasive quick reliable biomarkers to monitor disease severity and diagnosis are urgently needed in children with PH-related CHD. To the best of our knowledge, our study is the first study that evaluated the diagnostic and predictive values of plasma connective tissue growth factor levels in children with PH-related CHD.
Our results showed that the plasma levels of connective tissue growth factor were significantly elevated in patient with PH-related CHD compared to those with CHD only and to the control group. This was in agreement with the results of Li et al.Reference Li, Tang, Jia, Zhao, Liu and Liu14 Connective tissue growth factor secretion increased in several conditions such as increased mechanical stretch, pressure overload, and oxidative stress,Reference Blom, Goldschmeding and Leask15 which are all present in case of PH-related CHD. Moreover, Zhu et alReference Zhu, He, Xu, Zhang and Hu16 reported that immunohistochemical stains of lungs from rat PH model showed abundant connective tissue growth factor expression in pulmonary arterial smooth muscle cells and concluded that vascular remodelling closely associates with the proliferation of pulmonary arterial smooth muscle cells in PH and increased plasma levels of connective tissue growth factor seemed to reflect remodelling process.
Our study showed that plasma connective tissue growth factor can be used to diagnose PH in CHD children with a high sensitivity reaching 95% and a high specificity of 90% at a cut-off level ≥650 pg/mL. Similarly, Li et alReference Li, Tang, Jia, Zhao, Liu and Liu14 reported that the combination of connective tissue growth factor and brain natriuretic peptide increased the specificity for diagnosis of PH in children with CHD compared with brain natriuretic peptide alone (93 versus 76%). Moreover, our study revealed that plasma connective tissue growth factor levels were correlated with grading and severity of PH in children with PH-related CHD suggesting its potential possible role in the pathogenesis of PH-related CHD and its possible implication for predicting the severity of PH in these children.
The novel finding in our study was that the plasma connective tissue growth factor levels were significantly elevated in PH-related CHD patients with poor prognosis compared to those with good prognosis. Our study reported that plasma connective tissue growth factor can be used as a promising predictive biomarker for predicting adverse outcomes in children with PH-related CHD with a sensitivity of 88% and a specificity of 83% at a cut-off value of ≥1900 pg/mL.
In the present study, there was a significant positive correlation between plasma levels of connective tissue growth factor and both mean pulmonary artery pressure and pulmonary vascular resistance suggesting a pathological role linked to the increased pulmonary pressure. This was in agreement with the results of Liu et al.Reference Liu, Wang and Zhou17 Furthermore, there was a significant positive correlation between plasma connective tissue growth factor levels and right ventricular diameter which reflected the severity of PH. Increased afterload caused by increased pulmonary pressure in PH leads to right ventricular stretch and dilatation which correlated with the degree of pulmonary pressure.Reference Noordegraaf and Galie18
Interestingly, there was a significant negative correlation between plasma levels of connective tissue growth factor and the oxygen saturations in children with PH-related CHD. This was in agreement with the results of Li et alReference Li, Tang, Jia, Zhao, Liu and Liu14 who reported that children with cyanotic CHD and PH had significantly higher levels of plasma connective tissue growth factor compared to those with acyanotic CHD and PH. This can be explained by the fact that hypoxia increased the secretion of connective tissue growth factor.Reference Huang, Zou and Yu19
Our study also showed that there was significant negative correlation between plasma connective tissue growth factor levels and right ventricular diastolic function. Right ventricular diastolic dysfunction reflected severity of PH as persistent haemodynamic overload by PH induces right ventricular hypertrophy and results in accumulation of extracellular matrix, which impairs right ventricular diastolic compliance and function,Reference Ryan, Huston and Kutty20 and it is known that connective tissue growth factor enhances deposition of extracellular matrix in such conditions.
Our study reported that connective tissue growth factor is a promising biomarker that has good diagnostic and predictive values in children with PH-related CHD. However, more studies with larger sample size and longer follow-up are needed to confirm these results.
Limitation of the study is small number of the included children. Serial measurements of connective tissue growth factor levels before and after treatment in children with PH-related CHD to assess its value in predicting response to treatment were not performed. All of our patients had reversible PH, so we could not comment on the ability of connective tissue growth factor (CTGF) to predict reversibility of PH.
Conclusion
Plasma connective tissue growth factor is a promising biomarker with good diagnostic and predictive values in children with PH-related CHD.
Financial Support
This research received no specific grant from any funding agency, commercial, or not-for-profit sectors.
Conflicts of Interest
None.
Ethical Standards
The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national guidelines on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008, and has been approved by the institutional committees of Faculty of Medicine, Tanta University.








