Introduction
Juvenile recurrent parotitis is defined as a non-obstructive, non-suppurative inflammatory disease characterised by unilateral or bilateral parotid gland swelling recurring at least twice before puberty.Reference Nahlieli, Shacham, Shlesinger and Eliav1 Its incidence is unknown, but it is the second most common childhood disease of the salivary glands after mumps.
The clinical symptoms include intermittent, usually unilateral swelling of the parotid gland, which occurs suddenly (over minutes or hours) and may persist for days or weeks, and which is usually associated with pain and redness of the overlying skin and more general symptoms such as fever and malaise.Reference Leerdam, Martin and Isaacs2 The first episode typically occurs between the ages of 3 and 6 years (range, 6 months to 16 years),Reference Galili and Marmary3, Reference Ericson, Zetterlund and Ohman4 more often in males.Reference Geterud, Lindvall and Nylèn5, Reference Mandel and Bijoor6 The frequency of recurrence varies but may be as high as 30 episodes in one year, although the average is one-and-a-half episodes a year.
The aetiopathology of juvenile parotitis remains obscure, although it has been suggested that many factors may increase susceptibility, including dental malocclusion,Reference Bernkopf, Colleselli, Broia and de Benedictis7 congenital duct malformation,Reference Nahlieli, Shacham, Shlesinger and Eliav1, Reference Ericson, Zetterlund and Ohman4, Reference Sitheeque, Sivachandran, Varathan, Ariyawardana and Ranasinghe8 genetic factorsReference Kolho, Saarinen, Paju, Stenman, Stenman and Pitkaranta9–Reference Morales-Bozo, Urzua-Orellana, Landaeta, Montalbán, Torres and Pinochet11 and immunological anomaliesReference Shkalim, Monselise, Mosseri, Finkelstein and Garty12–Reference Havaldar16 (cases have been reported in patients with human immunodeficiency virus (HIV) infection, phagocyte dysfunction and humoral immunodeficiency). Another hypothesis considers juvenile recurrent parotitis to be a mucosa-associated lymphoid tissue disorder, and this is suggested by histological specimens showing hyperplastic cells surrounding the ducts in a manner similar to chronic inflammatory disorders. This can lead to parenchymal modifications of the glands and, according to Ussmuller and Donath,Reference Ussmuller and Donath17 even their complete lymphatic transformation, with the appearance of multiple myo-epithelial lesions that are interpreted as precursors of benign lympho-epithelial lesions.
The rarity of juvenile recurrent parotitis and the difficulty in defining its exact aetiopathology has led to a lack of universal guidelines for its diagnosis and management. Patients are therefore likely to be misdiagnosed, and may undergo inadequate and invasive diagnostic and therapeutic procedures.
The aim of this study was to review the literature in order to identify the role of modern diagnostic techniques in the management of juvenile recurrent parotitis, and to discuss the contribution of sialoendoscopy to its diagnosis and treatment on the basis of our own experience.
Review
Diagnosis
The diagnosis of juvenile recurrent parotitis is based on the clinical finding of recurrent parotid swelling and the radiological demonstration of sialectasia in children under 16 years of age. A blood test should be carried out to detect any viral or bacterial infections and to exclude mumps or other possible associations such as HIV, Sjögren's syndrome or general immunodeficiency.Reference Leerdam, Martin and Isaacs2 Traditional diagnostic methods include sialography and ultrasonography (US); computed tomography has also been described but represents a second choice.Reference Mandel and Bijoor6
Sialography shows the duct architecture of the salivary glands up to the fourth order of branching,Reference Kalinowsky, Heverhagen, Rehberg, Klose and Wagner18 and involves duct incannulation and the administration of a radiopaque iodate contrast medium.Reference Miziara and Campelo19, Reference Norman and McGurk20 In the presence of juvenile recurrent parotitis, the sialogram shows punctate shadows, strictures and kinks.Reference Miziara and Campelo19 Although sialography is considered an appropriate diagnostic method because of its high resolution and possible curative effect, its use is limited by the need for ionising radiation, allergy to the contrast medium, acute glandular infection and distal duct stenosis. Recent studies have shown that US is equally sensitive in detecting the pathological features of juvenile recurrent parotitis,Reference Leerdam, Martin and Isaacs2 as the multiple hypoechoic areas seen in US images seem to correspond to the punctate shadows seen in sialograms.Reference Galili and Marmary3, Reference Ussmuller and Donath17, Reference Miziara and Campelo19, Reference Nozaki, Harasawa, Hara, Kohno and Shigeta21 It can also be considered more tolerable, especially for young patients, but this is clearly operator-dependent. The use of colour Doppler allows rapid evaluation of the vascular parenchymal system of the gland, and provides information about vascular anatomy and flow velocity;Reference Martinoli, Derchi, Solbiati, Rizzatto, Silvestri and Giannoni22 patients usually show widespread glandular hyper-vascularisation during acute episodes, and hypo-vascularisation during quiescent phases.
Magnetic resonance imaging (MRI) has also been used. Two MRI patterns have been identified as typical of juvenile recurrent parotitis:Reference Huisman, Holzmann and Nadal23 (1) T1-weighted hypointense and T2-weighted hyperintense signals, with contrast enhancement, in the acute inflammatory stage; and (2) T1-weighted and T2-weighted isointense signal, without contrast enhancement, in comparison with the other major salivary glands, in the chronic inflammatory stage. Other commonly observed findings (especially in the chronic phase) are multiple cysts inside the parenchyma and the expansion of the Stensen ducts. The disadvantages of MRI are its high costs, limited availability, and the need for sedation in younger patients.
Magnetic resonance sialography has been recently introduced as a non-invasive radiological procedure. It is based on the principle of magnetic resonance hydrography, in which fluids are hyperintense on heavily T2-weighted images (i.e. using the constructive interference in steady state (‘CISS’) and half-Fourier single-shot turbo spin-echo (‘HASTE’) sequences).Reference Gadodia, Seith, Sharma and Thakar24, Reference Tonami, Ogawa, Matoba, Kuginuki, Yokota and Higashi25 Using this approach, magnetic resonance sialography can visualise the anatomy of the ducts up to the second or third order branching, and can reveal highly intense focal lesions corresponding to sialectasis. The constructive interference in steady state sequence shows the intraglandular ducts and sialectasis better than the half-Fourier single-shot turbo spin-echo sequence.Reference Gadodia, Seith, Sharma and Thakar24 The advantages of magnetic resonance sialography over standard sialography are: the use of saliva as a natural contrast medium; the lack of requirement to incannulate the duct or to use ionising radiation; and the facility to examine all four major salivary glands using multiple projection images in any plane, allowing optimal assessment of the ductal system.Reference Lomas, Carroll, Johnson, Antoun and Freer26 Moreover, continuous magnetic resonance sialography, performed after the administration of lemon juice, allows dynamic evaluation of parotid gland activity.Reference Morimoto, Ono, Tanaka, Kito, Inoue and Shinohara27
Finally, magnetic resonance virtual endoscopy and three-dimensional magnetic resonance sialography have been promoted on the basis of their imaging of vascular structures together with the gastrointestinal, biliary and urinary tracts.Reference Morimoto, Tanaka, Tominaga, Yoshioka, Kito and Ohba28 The resulting images have been compared with real endoscopic views. As these modalities provide useful morphological and pathological information, they could play a role in adapting sialoendoscopy to the individual patient's anatomy.Reference Su, Liao, Kang and Zou29
Sialoendoscopy is a new advance in optical medical systems which allows direct exploration of the intra- and extra-glandular system,Reference Nahlieli, Nakar, Nazarian and Turner30 and which can identify the morphological and inflammatory alterations responsible for the clinical symptoms of juvenile recurrent parotitis. Sialoendoscopy enables the establishment of an appropriate diagnosis, because it can identify the typical mucous plugs, stenosis and avascularisation of the ducts that are hidden by blood vessels under normal conditions.Reference Ericson and Sjoback13, Reference Quenin, Plouin-Gaudon, Marchal, Froehlich, Disant and Faure31–Reference Martins-Carvalho, Plouin-Gaudon, Quenin, Lesniak, Froehlich and Marchal33 The mini-endoscopes used in the salivary gland duct system can be divided into flexible, rigid, semi-rigid and, recently, flexible semi-rigid types. This last type seems to combine the advantages of the flexible and rigid mini-endoscopes, and is considered currently to be the best instrument available on the basis of its clear view, small diameter and stiffness.Reference Nahlieli, Nakar, Nazarian and Turner30 Sialoendoscopy was initially used to confirm the diagnosis of obstructions and strictures, and to remove sialoliths by means of different techniques and instruments;Reference Morimoto, Ono, Tanaka, Kito, Inoue and Shinohara27 more recently, it has been used in the diagnosis and treatment of juvenile recurrent parotitis.Reference Nahlieli, Shacham, Shlesinger and Eliav1, Reference Quenin, Plouin-Gaudon, Marchal, Froehlich, Disant and Faure31–Reference Faure, Querin, Dulguerov, Froehlich, Disant and Marchal35
Treatment
Historically, the treatment of juvenile recurrent parotitis has changed from invasive to more conservative surgery and ‘watch and wait’ approaches. Many of the options proposed in the past have now been almost totally abandoned: tympanic nerve section, duct ligation, the injection of sclerosing substances, partial or total parotidectomy, and low-dose radiotherapy.Reference Nahlieli, Shacham, Shlesinger and Eliav1, Reference Leerdam, Martin and Isaacs2, Reference Laskawi, Schaffranietz, Arglebe and Ellies36, Reference Mulcahy and Isaacs37 Previously, total parotidectomy with conservation of the facial nerve was the most widely used treatment option, and had a high success rate (80–100 per cent); however, it exposed patients to the risk of well-known complications such as facial paresis, Frey syndrome, ear lobe numbness, traumatic neuroma of the great auricular nerve, and an unsatisfactory aesthetic result.Reference Norman and McGurk20 More recently, a revised approach more attuned to confirmation of the benign nature of the pathology, and to the disappearance or attenuation of symptoms after puberty, has enabled avoidance of parotidectomy in all but a few cases.
Some authors recommend the continuous administration of low or standard doses of antibiotics early in an acute attack;Reference Galili and Marmary3, Reference Chitre and Premchandra38 however, there is no evidence that antibiotics affect the duration of episodes.Reference Galili and Marmary3, Reference Ericson, Zetterlund and Ohman4, Reference Cohen, Nussinovitch and Kauschansky39 Some patients do show a mucopus discharge from the parotid duct, but there is little evidence of bacterial involvement, and some studies suggest that salivary secretions contain normal mouth flora.Reference Ericson, Zetterlund and Ohman4, Reference Hara, Nagata, Mizuno, Ura, Matsuo and Ueda40 Anti-inflammatory therapy is used to treat the symptoms, and chewing gum or sialogogues, fluid intake, and hot compresses or massages in the parotid region have been proposed for the prevention of recurrence.Reference Chitre and Premchandra38
It is well known that sialography has curative effects in patients with juvenile recurrent parotitis.Reference Galili and Marmary3 Katz et al. Reference Katz, Hartl and Guerre41 have recently described their experience of using iodinated oil sialography to manage a large series of patients. The procedure was safe and painless, but 98 per cent of the treated patients experienced a recurrence after a mean symptom-free time of one year.
The introduction of salivary gland endoscopy has opened up new horizons, not only in diagnosis but also in the treatment and post-operative management of juvenile recurrent parotitis.
A study of 26 children by Nahlieli et al. Reference Nahlieli, Shacham, Shlesinger and Eliav1 identified the main features of mucous plugs, stenosis and duct avascularity, treated by washing the duct system, removing plaques from sialectatic ducts, and dilating strictures with high-pressure saline and, when necessary, a dilatation balloon; treatment was concluded with an intraduct steroid injection. After a follow-up period of 36 months, only 2 patients required repetition of the endoscopic procedure, because of recurrence of symptoms in the contralateral gland. The only transient side effect was gland swelling due to the irrigation.
Quenin et al. Reference Quenin, Plouin-Gaudon, Marchal, Froehlich, Disant and Faure31 have confirmed the usefulness of sialoendoscopy as a diagnostic and interventional procedure in juvenile recurrent parotitis, by observing clinical resolution in 90 per cent of 10 cases (7 bilateral) after a follow-up period of 11 months. However, two cases experienced swelling of the pharyngeal portion of the parotid gland, with partial upper airway obstruction. Finally, a high success rate was obtained in a large series of 70 children who were followed up for 6–36 months; only 5 patients experienced symptom recurrence.Reference Shacham, Droma, London, Bar and Nahlieli32
Personal experience
Between January 2005 and July 2010, 14 children (8 boys and 6 girls; mean age 7.9 years; age range 4–12 years) with symptomatic unilateral (8 cases) or bilateral (6 cases) juvenile recurrent parotitis were treated at the otolaryngological clinic of the Fondazione Policlinico, University of Milan.
The diagnosis was based on clinical symptoms and supported by US and colour Doppler US findings (using a Hitachi H21 system (Hitachi, Tokyo, Japan); US frequency 7.5 MHz).
Five patients also underwent dynamic magnetic resonance sialography using a Gyroscan Intera system (Philips, Eindhoven, The Netherlands) with axial T2-weighted turbo spin-echo cross-sectional sequences and T2-weighted spin-echo sequences with three-dimensional and maximum intensity projection (‘MIP’) reconstruction. All patients underwent a blood examination comprising blood cell counts, total and partial immunoglobulin (Ig) analysis (i.e. IgA, IgM, IgG and IgE), erythrocyte sedimentation rate, polymerase chain reaction testing and autoantibody testing (for anti-Ro/SSA, anti-La/SSB and anti-nuclear autoantibodies and rheumatic factor).
The indication for sialoendoscopy was at least 2 swelling episodes during a 12-month period.
Written, informed consent was obtained for each procedure. The study was approved by the institutional review board of the Fondazione IRCCS Ca' Granda Ospedale Maggiore Policlinico.
Sialoendoscopy was performed under general anaesthesia using a flexible, semi-rigid, nitinol sialoendoscope (0.8 mm with ‘all-in-one’ telepack camera system; Karl Storz, Tuttlingen, Germany). Lavage and dilatation with saline under pressure (about 60 ml) enabled passage of the sialoendoscopic unit through the duct system to at least the second order branching. Before removing the sialoendoscope, an intraductal injection of hydrocortisone 100 mg and Rifocin 250 mg/3 ml (Sanofi, Paris, France) was usually administered. The patients usually received systemic antibiotic prophylaxis during the endoscopic procedure. They underwent follow-up evaluation a month later and then every year (mean follow up, 30 months; range, 12–55 months).
Twenty sialoendoscopic procedures were performed in total (eight unilateral and six bilateral). The patients' main demographic, clinical and therapeutic data are shown in Table I. The mean duration of the procedure was 20 minutes for each gland. Failure to enter the duct system was not encountered in any patient. In all cases, the diagnostic endoscope was able to pass into the second order branching, and into the third order branching in eight glands (40 per cent).
Table I Sialoendoscopies: demographic, clinical and therapeutic data

* In the previous year. Paradise score: 0 = tonsils fit within tonsillar fossa; 1 = tonsils <25 per cent of space between pillars; 2 = tonsils <50 per cent of space between pillars; 3 = tonsils <75 per cent of space between pillars; 4 = tonsils >75 per cent of space between pillars. Pt no = patient number; yr = years; FU = follow up; mths = months; 2° proc = secondary procedure; prev Sx = previous surgery; SE = sialoendoscopy; rec = recurrence; M = male; F = female; ADT = adenotonsillectomy; AD = adenoidectomy
During endoscopy, the ductal layer appeared white, without the normal blood vessel coverage usually present (Figure 1). All the patients showed main duct strictures and dilation, but all of the strictures were less than 50 per cent of the duct lumen. Mucous plugs were found in 12 glands (60 per cent), most being related to strictures. Stensen duct kinks were observed during six procedures. There were no post-procedure complications except for swelling of the gland due to irrigation, which variably and spontaneously resolved within a few hours.

Fig. 1 Sialoendoscopic view of a parotid gland duct in a child with juvenile recurrent parotitis, showing the white appearance of the ductal layer, without the blood vessel coverage usually present.
A successful result (i.e. a reduction in the number of acute episodes of parotitis) was obtained in all patients (see Table I). During the mean 30-month follow-up period, 5 patients experienced a recurrence of symptoms (36 per cent), with a mean symptom-free period of 20 months. A second sialoendoscopy was performed in three recurrent cases; these patients experienced at least two episodes of swelling in the one year.
The blood tests showed serum IgA deficiency in three children without a history of immune problems.
The patients' past medical histories revealed previous adenotonsillectomy (six children) or adenoidectomy (three children); the remaining five patients showed adenotonsillar hypertrophy (at least Paradise grade 3).
Clinical examination revealed pathological cervical lymph nodes in all patients. No other specific disease was reported.
Ultrasound examination showed: typically low, heterogeneous echogenicity; multiple small, hypoechogenic areas indicating duct dilation; and hyperplasic cells around the ducts of all involved glands (Figure 2).
Fig. 2 Ultrasonograph showing the parotid gland in a child with juvenile recurrent parotitis, showing the typically low, heterogeneous echogenicity, with multiple small, hypoechogenic areas.
Colour Doppler US identified hypovascularisation during the quiescent phase of juvenile recurrent parotitis, and hypervascularisation during the acute phase.
Dynamic magnetic resonance sialography was well tolerated by the five children who underwent it, and was of diagnostic quality. It allowed the visualisation of intraglandular branches at least to the second order of branching. In all five patients, we found a high intensity, focal lesion signal suggesting sialectasis involving all of the parotid gland (particularly the symptomatic glands) (Figure 3). In addition, four children showed isointense general parotid gland signals on T2-weighted imaging, suggesting no active inflammation (when compared with the submandibular and sublingual glands); however, the fifth child showed a hyperintense general parotid signal on T2-weighted imaging, suggesting acute parotid inflammation. All of the patients had enlargement of the symptomatic parotid glands, and of intraparotid and cervical lymph nodes.
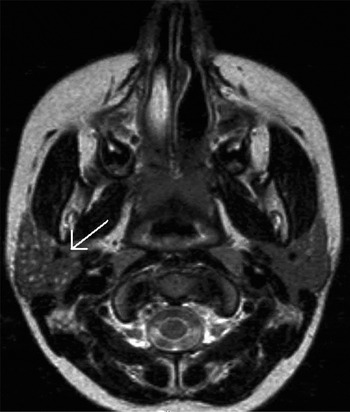
Fig. 3 Axial, dynamic magnetic resonance sialograph of the right parotid gland in a child with juvenile recurrent parotitis, showing high intensity, intraglandular, focal lesion signals (arrow) suggesting sialectasis.
Discussion
The management of juvenile recurrent parotitis is still controversial despite the development of modern diagnostic tools and the use of salivary gland endoscopy. The diagnosis has traditionally been made on the basis of recurrent parotid swelling together with radiological demonstration of sialectasis by means of sialography. Modern radiological approaches include the use of US, colour Doppler US and magnetic resonance sialography, which are all valid, non-invasive alternatives to sialography for the morphological study of the parotid duct system and the glandular parenchyma. Sialoendoscopy is a minimally invasive procedure that provides direct information about the morphology of the salivary duct system and all possible causes of salivary obstruction.
In our study of 14 children, diagnostic US evaluation allowed us to identify all of the previously described, typical pathological features of juvenile recurrent parotitis,Reference Leerdam, Martin and Isaacs2, Reference Galili and Marmary3, Reference Ussmuller and Donath17, Reference Nozaki, Harasawa, Hara, Kohno and Shigeta21 and colour Doppler US provided further information about flow speed that made it possible to differentiate the acute and chronic phases of the disease. When used, magnetic resonance sialography revealed the anatomy of the ducts up to the second or third order branching; high intensity, focal lesion signals corresponded to sialectasis. Finally, diagnostic sialoendoscopy showed the typical white appearance of the ductal layer, without the normal, healthy blood vessel coverage, and also the presence of mucous plugs and duct anomalies (e.g. strictures and kinks) as previously reported by other authors.Reference Nahlieli, Shacham, Shlesinger and Eliav1, Reference Quenin, Plouin-Gaudon, Marchal, Froehlich, Disant and Faure31–Reference Faure, Froehlich and Marchal34
Various invasive and non-invasive therapeutic procedures have been proposed for the management of juvenile recurrent parotitis. Of these, operative sialoendoscopy seems to be the preferred technique because it is safe and minimally invasive. Its therapeutic uses include dilatation of the restricted duct system, possible resolution of duct anomalies, and injection of saline, steroids and antibiotics into the duct. It has been demonstrated that the mere intraductal instillation of saline can be effective in managing chronic sialadenitis.Reference Antoniades, Harrison, Epivatianos and Papanayotou42 In our series, we observed a reduction in the number of acute parotitis episodes in all patients over a mean follow-up period of 30 months. Our results are in line with those of previous studies demonstrating the effectiveness of this therapeutic method.Reference Nahlieli, Shacham, Shlesinger and Eliav1, Reference Quenin, Plouin-Gaudon, Marchal, Froehlich, Disant and Faure31–Reference Faure, Froehlich and Marchal34
With regard to aetiopathogenesis, the therapeutic role of duct dilatation and the efficacy of intraductal steroid injection during operative sialoendoscopy seem to support the hypothesis of an immunological disorder. The activation of multiple lymphocyte infiltrates, observed in previous studies, may favour the theory of an inflammatory reaction near the ducts, as indicated by the histological detection of hyperplastic cells around the duct.Reference Ussmuller and Donath17 Ussmuller and DonathReference Ussmuller and Donath17 observed the progressive replacement of the parenchyma by lymphatic tissue in salivary glands that had been removed because of juvenile recurrent parotitis, and concluded that this could be related to a mucosa-associated lymphoid tissue disorder. Interestingly, the colour Doppler US scans of all our patients showed reactive intraparenchymal lymph nodes. Moreover, many of these patients showed high-grade adenotonsillar hypertrophy (Paradise grade 3–4), and the patients who had previously undergone adenotonsillar surgery suffered a greater number of parotitis episodes. It is tempting to speculate that the removal of such lymphatic tissue may favour an increase in lymphocytic follicular hyperplasia in the salivary gland. It is hypothesised that such hyperplasia, and the resulting deficient immune response, occur as part of a local mucosa-associated lymphoid tissue disorder. The disappearance or attenuation of the symptoms of juvenile recurrent parotitis, commonly seen after puberty, could therefore be an expression of the maturation of the local mucosa-associated lymphoid tissue system. It is also interesting that three of our patients had a serum IgA deficit; this is in keeping with Fazekas and colleagues' findingReference Fazekas, Wiesbauer, Schroth, Potschger, Gadner and Heitger14 that 23 per cent of their patients were IgA-deficient, compared with only 0.21 per cent of their healthy subjects. This further supports the hypothesis of an inadequate local immune response.
Conclusion
The use of modern, minimally invasive diagnostic tools such as colour Doppler US, magnetic resonance sialography and sialoendoscopy represents a new frontier in the management of juvenile recurrent parotitis. Sialoendoscopy can also have an important therapeutic effect by reducing the number of recurrent acute parotitis episodes, thus giving patients a better quality of life until puberty.






