Introduction
Postpartum depression (PPD) is one of the most common disorders following childbirth (Rasmussen, Strøm, Wohlfahrt, Videbech, & Melbye, Reference Rasmussen, Strøm, Wohlfahrt, Videbech and Melbye2017) with a global prevalence of 17% and an incidence of 12% (Hahn-Holbrook, Cornwell-Hinrichs, & Anaya, Reference Hahn-Holbrook, Cornwell-Hinrichs and Anaya2018; Shorey et al., Reference Shorey, Chee, Ng, Chan, Tam and Chong2018). PPD can occur in the first hours after giving birth through the end of the first postpartum year (American College of Obstetricians and Gynecologists Committee on Health Care for Undeserved Women, 2018; Gaynes et al., Reference Gaynes, Gavin, Meltzer-Brody, Lohr, Swinson, Gartlehner and Miller2005; O'Hara & McCabe, Reference O'Hara and McCabe2013; Yim, Tanner Stapleton, Guardino, Hahn-Holbrook, & Dunkel Schetter, Reference Yim, Tanner Stapleton, Guardino, Hahn-Holbrook and Dunkel Schetter2015). When left untreated, PPD seriously impacts the health of the mother and her baby (Slomian, Honvo, Reginster, & Bruyère, Reference Slomian, Honvo, Reginster and Bruyère2019; Stein et al., Reference Stein, Pearson, Goodman, Rapa, Rahman, McCallum and Pariante2014) with the worst consequences being suicide ideation, attempted suicide or suicide (Esscher et al., Reference Esscher, Essén, Innala, Papadopoulos, Skalkidou, Sundström-Poromaa and Högberg2016; Orsolini et al., Reference Orsolini, Valchera, Vecchiotti, Tomasetti, Iasevoli, Fornaro and Bellantuono2016) as well as infanticidal thoughts (Barr & Beck, Reference Barr and Beck2008). An early method to reduce the burden of PPD and its consequences is through prevention (Arango et al., Reference Arango, Díaz-Caneja, McGorry, Rapoport, Sommer, Vorstman and Carpenter2018), that is, before the woman develops the disorder.
Approaches to prevent depression can be divided into three types according to the target population (Mrazek & Haggerty, Reference Mrazek and Haggerty1994). Universal prevention is directed at the full population, selective prevention is focused on people who have been exposed to risk factors related to the onset of the disorder, and indicated prevention is targeted at people with prodromal symptoms not yet meeting the diagnostic criteria of a depressive disorder (World Health Organization, 2004). According to O'Connor, Senger, Henninger, Coppola, and Gaynes (Reference O'Connor, Senger, Henninger, Coppola and Gaynes2019), most interventions focused on preventing PPD have been based on a psychological approach.
To the best of our knowledge, seven systematics reviews and meta-analysis (SRs/MAs) on the effectiveness of interventions for the prevention of PPD including psychological strategies have been published to date (Cluxton-Keller & Bruce, Reference Cluxton-Keller and Bruce2018; Dennis & Dowswell, Reference Dennis and Dowswell2013; Lin, Xue, Yang, Li, & Cao, Reference Lin, Xue, Yang, Li and Cao2018; Morrell et al., Reference Morrell, Sutcliffe, Booth, Stevens, Scope, Stevenson and Stewart-Brown2016; O'Connor et al., Reference O'Connor, Senger, Henninger, Coppola and Gaynes2019; Sockol, Neill Epperson, & Barber, Reference Sockol, Neill Epperson and Barber2013; Yasuma et al., Reference Yasuma, Narita, Sasaki, Obikane, Sekiya, Inagawa and Nishi2020). The general conclusion of all of them is that the interventions studied are effective in preventing PPD. However, there are some differences between these SRs/MAs and the present study. The main difference is that the above SRs/MAs do not exclude women with a diagnosis of depression at the beginning of the intervention (that is, at study baseline), although two of them excluded trials where more than 20% (Dennis & Dowswell, Reference Dennis and Dowswell2013) or 50% (O'Connor et al., Reference O'Connor, Senger, Henninger, Coppola and Gaynes2019) of the participants were depressed at baseline. Consequently, the results preclude making a clear distinction to be made between prevention effectiveness and treatment effectiveness. Second, two of the SR/MAs focused on specific types of interventions, such as family therapeutic interventions (Cluxton-Keller & Bruce, Reference Cluxton-Keller and Bruce2018) or self-help psychological interventions (Lin et al., Reference Lin, Xue, Yang, Li and Cao2018). Third, the other SR/MAs focused only on prenatal trials for universal prevention (Yasuma et al., Reference Yasuma, Narita, Sasaki, Obikane, Sekiya, Inagawa and Nishi2020). Finally, one of the SRs/MAs only included studies conducted in countries ranked as having ‘very high’ human development according to the World Health Organization (O'Connor et al., Reference O'Connor, Senger, Henninger, Coppola and Gaynes2019). Additionally, new randomized controlled trials (RCTs) on interventions for the prevention of PPD have recently been published.
The aim of this study was to conduct an SR/MA of RCTs assessing the effectiveness of psychological interventions in preventing PPD in non-depressed women.
Method
The study followed the PRISMA guidelines for reporting SRs and MAs (Moher, Liberati, Tetzlaff, & Altman, Reference Moher, Liberati, Tetzlaff and Altman2009). The protocol of the study was registered with the International Prospective Register of Systematic Reviews (PROSPERO) [registration number: CRD 42018109981] and published elsewhere (Martín-Gómez et al., Reference Martín-Gómez, Moreno-Peral, Bellón, Conejo Cerón, Campos-Paino, Gómez-Gómez and Motrico2020).
Search strategy
Relevant electronic databases were searched including MEDLINE (through Ovid and PubMed), PsycINFO, Web of Science, Scopus, CINAHL, Cochrane Central Register of Controlled Trials (CENTRAL), OpenGrey (System for Information on Grey Literature in Europe), Australian New Zealand Clinical Trial Registry (ANZCTR) and clinicaltrial.gov from inception to 17 August 2020. The search was performed following the PICO model and using medical headings and keywords associated with RCTs, prevention and PPD. Searches were piloted first in PubMed and then adapted to be run across the rest of the databases. online Supplementary eAppendix 1 shows the search strategy used for each database. PROSPERO was searched for similar ongoing or recently completed SRs. Meta-Analytic Database, an academic website comprising electronic databases, was also explored. In addition, SRs and MAs in the field of prevention and PPD were hand-searched, and their reference lists were reviewed, as were the references from the RCTs included in this SR/MA. Authors from studies included in this SR/MA as well as experts in the field were contacted to identify additional relevant studies missing from our search.
Eligibility criteria
Eligible participants were pregnant women or women who had given birth in the past 12 months who were non-depressed at baseline. Since some interventions may begin before delivery, pregnant women were included when the study reported a measure of PPD after delivery. In order to distinguish PPD prevention from treatment interventions, depression had to be ruled out through diagnosis by a mental health specialist or through validated scales with standard cut-off points or standardized interviews. Studies that included depressed and non-depressed women at baseline were also included when they reported separate results for non-depressed participants or if the authors replied to our request for separate results for non-depressed participants. Eligible interventions were psychological interventions, including those with psychoeducational and psychosocial approaches. Psychological interventions were considered to be those that aim to change the thoughts and behaviors of an individual (e.g. cognitive-behavioral therapy, interpersonal therapy and psychological debriefing) (Dennis and Dowswell, Reference Dennis and Dowswell2013). The psychoeducational approach is focused on informing women about PPD without engaging them in an active intervention (e.g. information sessions and the distribution of fact sheets) (Sockol et al., Reference Sockol, Neill Epperson and Barber2013). When interventions aim to promote changes through certain links with the social environment (e.g. home visits, telephone support, group interventions and interventions in which the woman's partner has been included in the session) are considered a psychosocial approach (Dennis and Dowswell, Reference Dennis and Dowswell2013; Sockol Reference Sockol2015). Despite this differentiation, these types of interventions often overlap in actual practice. Interventions implemented before and/or after delivery were included. The comparators allowed were usual care, attention control, waiting list or no intervention. Outcomes (primary or secondary) included the incidence of new cases of PPD and/or the reductions in postpartum depressive symptoms during the first year after childbirth, measured by validated scales or standardized interviews. The RCT was the only design included because it provides more evidence on causality than other types of studies (Piantadosi, Reference Piantadosi2017). Restrictions regarding language or setting were not imposed. When necessary, additional information was sought from the corresponding author to resolve any questions about eligibility.
Study selection
After duplicate records were eliminated, two researchers (CM-G and HC-P) completed the entire study selection process separately. The titles and abstracts of all studies were reviewed. Studies that did not meet the inclusion criteria were excluded. The full texts of the remaining studies were reviewed. Disagreements were resolved through a third independent researcher (EM). The inter-agreement of the initial total full-text selection between reviewers was excellent (Fleiss, Levin, & Paik, Reference Fleiss, Levin and Paik2013) [Cohen's K = 0.82; 95% confidence interval (CI) 0.77–0.88].
Data extraction
Two researchers (CM-G and HC-P) independently extracted all the relevant characteristics of the included studies. Discrepancies were resolved by consensus between both reviewers. Information related to author, year, country, target population characteristics, type of prevention, session details for the intervention group, sample size (control/intervention) and type of control group was extracted. Furthermore, the exclusion criteria regarding depression at baseline, PPD outcomes and validated instruments used (cut-off if a scale was used), and follow-up evaluations over time provided by the RCTs were collected.
Risk of bias
To assess the quality of the studies included, the Cochrane Collaboration risk-of bias-tool version 1(Higgins & Green, Reference Higgins and Green2011) was used. This tool allows the risk of bias to be measured by six items: (1) random sequence generation, (2) allocation concealment, (3) blinding of the participants and personnel, (4) blinding of the outcome assessments, (5) incomplete reporting of the outcome data, and (6) selective reporting of the data.
Each study was evaluated quantitatively and qualitatively. Quantitatively, in items 1–6, zero points were assigned for low risk of bias, one point for unclear risk of bias and two points for high risk of bias. The risk of bias score ranges between 0 and 12 points, considering RCTs to have a low risk when scoring ⩽ 3 points, moderate risk when scoring 4–5 points and high risk when scoring ⩾6. Following previous studies (Gómez-Gómez et al., Reference Gómez-Gómez, Bellón, Resurrección, Cuijpers, Moreno-Peral, Rigabert and Motrico2020; Rigabert et al., Reference Rigabert, Motrico, Moreno-Peral, Resurrección, Conejo-Cerón, Cuijpers and Bellón2020), items 1,2, 4, 5 and 6 were evaluated qualitatively. Item 3 was excluded given that the nature of the interventions included in this study precluded blinding of the outcome assessments. Accordingly, each item mentioned was evaluated by assigning the label low, unclear or high risk of bias. Each study was subsequently coded taking into account the following: when all the items scored as low risk of bias, the study was coded with an overall low risk of bias. When the items were assessed with low and unclear risk of bias, or only unclear, the study was coded with moderate risk of bias. In studies in which at least one of the items was assessed as being at high risk of bias, the study was coded with a high risk of bias. The quality ratings were checked by two researchers (CM-G and PM-P) and disagreements were resolved by a consultation with a third independent researcher (SC-C). The initial level of agreement between researchers was excellent (Fleiss et al., Reference Fleiss, Levin and Paik2013) (Cohen's K = 0.90; 95% CI 0.72–0.97).
Assessment of publication bias
Publication bias was estimated by analyzing the funnel plot and through Duval and Tweedie's trim-and-fill procedure (Duval & Tweedie, Reference Duval and Tweedie2000). Begg and Mazumdar's rank correlation (Begg & Mazumdar, Reference Begg and Mazumdar1994) and Egger's test (Egger, Davey Smith, Schneider, & Minder, Reference Egger, Davey Smith, Schneider and Minder1997) were also performed.
Data analysis
Quantitative data from each study were extracted independently by two researchers (CM-G and SC-C). Statistical analyses were carried out using the Comprehensive Meta-Analysis (CMA) software package, V.3 (Borenstein, Hedges, Higgins, & Rothstein, Reference Borenstein, Hedges, Higgins and Rothstein2013) and STATA-Release V.14.2 (Press, Reference Press2019). We used the standardized mean difference (SMD) between the intervention and the control group as a measure of effect. Negative SMDs indicated a better outcome in the intervention group. The effect size was interpreted following Cohen's proposal: 0.20 corresponds to a small effect size, 0.50 corresponds to medium effect size and 0.80 corresponds to a large effect size (Cohen, Reference Cohen1989). A random-effects model was selected for pooling effect size because studies included in the SR/MA were carried out with heterogeneous populations (Higgins & Green, Reference Higgins and Green2011). As the Edinburgh Postnatal Depression Scale (EPDS) was the most used scale to assess depressive symptoms across the included RCTs and it is a specific scale to assess PPD symptoms, it was selected when the RCTs also reported data from another scale. When studies only reported incidence (Phipps, Raker, Ware, & Zlotnick, Reference Phipps, Raker, Ware and Zlotnick2013; Zlotnick, Johnson, Miller, Pearlstein, & Howard, Reference Zlotnick, Johnson, Miller, Pearlstein and Howard2001), CMA was used to obtain the equivalent SMD (inputting the events and the sample size of each group -intervention and control- in the software spreadsheet; the software automatically calculates the corresponding SMD). The first post-intervention measure assessed after delivery and reported in the study was the measure used for the effect size analyses. In one RCT (Phipps et al., Reference Phipps, Raker, Ware and Zlotnick2013) where only incidence was evaluated, the measure used was the first measure with cases of depression in the intervention group or the control group.
The heterogeneity of the effect sizes was estimated through visual inspection of the forest plots and Cochran's Q statistic with its p value. Heterogeneity was also tested with the I 2 statistic, which can quantify heterogeneity ranging from 0% (no heterogeneity) to 100% (the differences between the effect sizes can be fully explained by chance). The interpretations of the percentages are as follows: 0–40% indicates potentially unimportant heterogeneity, 30–60% indicates moderate heterogeneity, 50–90% indicates substantial heterogeneity and 75–100% indicates considerable heterogeneity (Higgins & Green, Reference Higgins and Green2011).
Sensitivity analyses were performed using a fixed-effects model and Hedges' g; with the profile likelihood method (an alternative to the DerSimonian-Laird method, which is more conservative and convenient when the number of studies is small), excluding the RCT that caused the greatest increase in heterogeneity, with the mean follow-up (for each RCT, we calculated the SMD by combining the SMD at different postpartum and post-test follow-up times into a single estimate as the mean) and with the most recent postpartum evaluation. Sensitivity analyses were also conducted excluding RCTs with a high risk of bias based on quantitative and qualitative assessments and using RCTs coded as low risk of bias from the quantitative as well as from the qualitative assessments.
Subgroup analyses were performed using a mixed-effects model according to the following predefined variables: previous deliveries (primiparous only v. primiparous and multiparous), type of prevention (selective/indicated v. universal preventive interventions), age (adolescents v. adolescents and adults), ethnicity (intervention targets women of a specific ethnic group v. does not target), intervention timing (prepartum interventions only v. interventions carried out during prepartum and postpartum period; v. postpartum intervention only; v. intervention carried out during prepartum or postpartum period) and previous history of depression (women with or without a previous history of depression v. women without a previous history of depression). Due to large differences between RCTs included in this SR/MA, post hoc subgroup analyses were also performed (Higgins et al., Reference Higgins, Thomas, Chandler, Cumpston, Li, Page and Welch2020) according to the intervention orientation (cognitive-behavioral therapy or interpersonal therapy or other), risk of bias coded from the quantitative criteria (low v. moderate v. high) and qualitative criteria (low and moderate v. high; low v. moderate and high) and sample size.
Meta-regressions were conducted to explain the between-trial heterogeneity. A priori, to adjust for risk of bias it was forced into the multivariate meta-regression models. The sample size was not included in the meta-regression model, as expected (Martín-Gómez et al., Reference Martín-Gómez, Moreno-Peral, Bellón, Conejo Cerón, Campos-Paino, Gómez-Gómez and Motrico2020), because publication bias was not detected. To explain the maximum degree of heterogeneity we obtained the most parsimonious meta-regression model (including the least number of variables) with the best goodness of fit, using a post hoc analysis strategy. Before including the data in a meta-regression analysis, the normality of the distribution was confirmed by skewness and kurtosis normality tests for quantitative variables (D'Agostino, Belanger, & D'Agostino, Reference D'Agostino, Belanger and D'Agostino1990) and transformations were conducted, when appropriate, to approximate normality. Among the covariates considered for the subgroup analysis, those with a significance level of p < 0.15 in bivariate meta-regression and those that were not removed from the model due to collinearity were also included in the meta-regression models. CIs and standard errors were calculated using the Knapp and Hartung method (Knapp & Hartung, Reference Knapp and Hartung2003). p values were also computed using the Higgins and Thompson (Higgins & Thompson, Reference Higgins and Thompson2004) permutation test. A plot of the standardized shrunken residuals was used to test the goodness of fit in the meta-regression models. Likewise, taking into account the variable included in the final meta-regression model (previous deliveries), an ad hoc MA of random effects stratified according to this variable was performed.
Quality of evidence
The GRADE (Grade of Recommendation, Assessment, Development and Evaluation) system (Balshem et al., Reference Balshem, Helfand, Schünemann, Oxman, Kunz, Brozek and Guyatt2011) was used to determine the overall quality of evidence. Assessment of the quality of the evidence considers five aspects: risk of bias, publication bias, imprecision (random error), inconsistency and indirectness (Guyatt, Oxman, Schünemann, Tugwell, & Knottnerus, Reference Guyatt, Oxman, Schünemann, Tugwell and Knottnerus2011).
Results
Study selection
A total of 7187 records were identified (3903 after removal of duplicates). Of these, 312 were examined in full text. As a result, 17 RCTs reported in 18 articles met the inclusion criteria for this SR/MA. online Supplementary eAppendix 2 provides the references for all included studies. For MA calculations, we used 15 RCTs reported in 16 articles because two (Crockett, Zlotnick, Davis, Payne, & Washington, Reference Crockett, Zlotnick, Davis, Payne and Washington2008; Hagan, Evans, & Pope, Reference Hagan, Evans and Pope2004) of the 17 RCTs included in the SR did not report the necessary data even after contacting the authors (see Fig. 1).

Fig. 1. PRISMA Flow diagram.
Study characteristics
The characteristics of the 17 RCTs included are described in Table 1. The RCTs included were published between 2001 and 2019. A total of 4958 participants were enrolled. The sample size ranged from 35 to 2241 (median = 106). 12 RCTs were carried out in the United States and the remaining five were conducted in the United Kingdom, Portugal, Norway, Australia and China.
Table 1. Characteristics of included studies
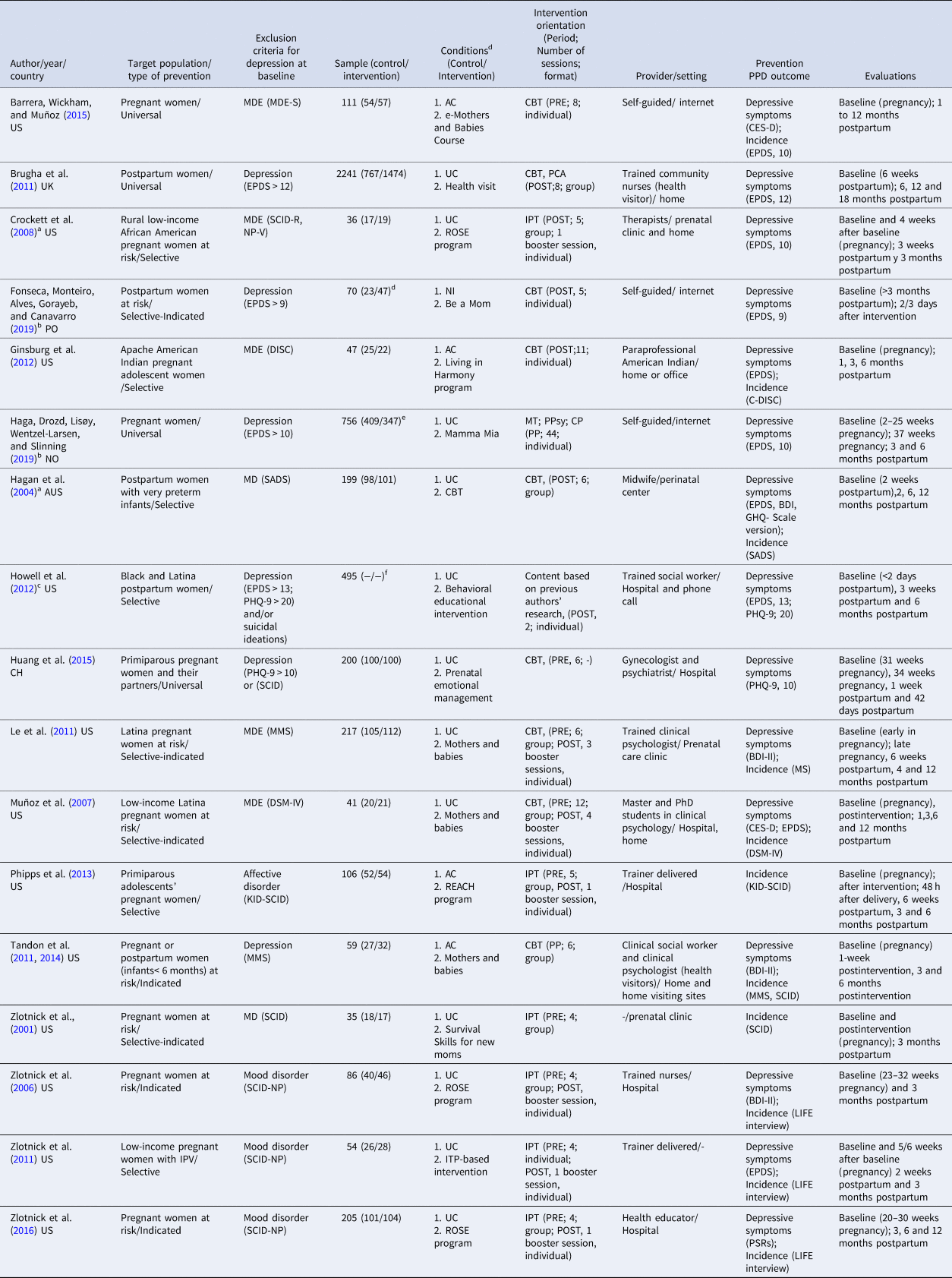
US, United states; UK, United Kingdom; PO, Portugal; NO, Norway; AUS, Australia; CH, China; IPV, Intimate partner violence; MDE, Major depressive episode; MDE-S, Major Depressive Episode Screener; SCID-R, NP-V, Structured Clinical Interview for DSM Revised Non-Patient Version; EPDS, Edinburgh Postnatal Depression Scale; DISC, Diagnostic Interview Schedule for Children-Computer version; MD, major depression; SADS, Schedule for Affective Disorders and Schizophrenia; PHQ-9, Patient Health Questionnaire; SCID, Structured Clinical Interview for DSM Disorders; MS, Mood Screener; DSM-IV = Diagnostic and Statistical manual of Mental Disorders criteria; MMS, Maternal Mood Screener; KID-SCID, Structured Clinical Interview for DSM Disorders-Childhood version; SCID-NP, Structured Clinical Interview for DSM Disorders -Non-Patient edition; AC, Active control; UC, usual care; NI, no intervention; CBT, cognitive behavioral therapy; ITP, interpersonal therapy; PCA, person-centered approach; MC, metacognitive therapy; PPsy, positive psychology; CP, couple therapy; PRE, prepartum intervention; POST, postpartum intervention; PP, prepartum and postpartum intervention; CES-D, Center for Epidemiological Studies-Depression Scale; BDI-II, Beck Depression Inventory-II; GHQ, General Health Questionnaire; LIFE interview, Longitudinal Interval Follow-up Evaluation; PSRs, Psychiatric Status Ratings.
a This study is included in the systematic review only, not in the meta-analysis.
b Depressed women were not excluded at study baseline, but, upon request, the authors submitted results for non-depressed participants at baseline.
c Depressed women were not excluded at study baseline but the results are reported separately for non-depressed women.
d Only subclinical sample included. Total sample of 194 (96/98).
e Only subclinical sample included. Total sample of 962 (431/531).
f Only subclinical sample included. Total sample of 540 (270/270).
Regarding the target population, 12 RCTs focused on pregnant women, four on postpartum women and one on both. Two of them were aimed only at primiparous women. The majority of the RCTs focused on adult women and two were conducted with adolescents. Five RCTs focused on ethnic minorities, such as African American women, Apache Indians and Latinas in the United States. One of the studies focused on women who suffered intimate partner violence and another was conducted with women and their partners.
Regarding the type of prevention, four RCTs conducted universal prevention, six selective prevention, three indicated prevention and four included both selective and indicated prevention (for inclusion, women had to have a social risk factor for PPD and/or the previous history of depression and/or subthreshold symptoms of PPD). Nine RCTs used a standardized interview and five RCTs used a scale with a validated cut-off point to exclude depression at baseline. One study reported separately the results of women without depression at baseline, and in two articles, upon request, the corresponding authors sent us the data on women without depression at baseline. In the last three articles, their evaluations at baseline were also performed using a validated scale with a standard cut-off point.
Concerning the period in which the intervention was carried out, in nine RCTs the interventions were performed during pregnancy and, of these, six had postpartum reminder sessions. Six RCTs were conducted in the postpartum period and, of these, one carried out reminder sessions in the later postpartum period. Two RCTs included interventions carried out during pregnancy and in the postpartum period but one was because the intervention included pregnant and postpartum women together; therefore, not all of the women participated in the intervention during pregnancy and after delivery. Interventions were based on cognitive behavioral therapy in nine RCTs, and one also combined this with a person-centered approach. Interpersonal therapy was used in seven RCTs, and in one this was combined with metacognitive therapy and positive psychology. Interventions were delivered in an individual format in six RCTs, in a group format in five RCTs and combining both in five further RCTs. The number of sessions was between two and 44 (median = 5). Interventions were provided by health professionals (nurses, therapists, midwives, gynecologists, psychiatrists, clinical psychologists and clinical social workers), predoctoral and postdoctoral students in clinical psychology, paraprofessionals from the same cultural background as the participants, social workers and other trained interventionists. Three RCTs were self-guided online interventions. In seven RCTs, the setting was a hospital or perinatal clinic or center. Interventions were delivered through home visits or combining home visits and hospital interventions, telephone interventions (Howell et al., Reference Howell, Balbierz, Wang, Parides, Zlotnick and Leventhal2012) and in places adapted to carry out interventions such as offices or home visit sites. The comparators were usual care in 12 RCTs, active control in four RCTs and no intervention in one RCT.
Regarding the outcome on PPD, six RCTs reported postpartum depressive symptomatology, two RCTs reported the incidence of PPD and nine RCTs reported both. The last follow-up evaluation was carried out 42 days after delivery, during the third or sixth month postpartum and at 12 or 18 months postpartum.
Risk of bias of the included studies
From the quantitative criteria, five RCTs had a low risk of bias, six had a moderate risk of bias and six had a high risk of bias. From the qualitative criteria, two RCTs had a low risk of bias, five had a moderate risk of bias and 10 had a high risk of bias. The risk of bias of each study is reported in online Supplementary eAppendix 3.
Effectiveness of psychological interventions to prevent PPD
For MA calculations we used 15 RCTs reported in 16 articles. The pooled SMD was −0.175 (95% CI −0.266 to −0.083; p < 0.001) for the random model. Heterogeneity was low (I 2 = 21.20%) and not statistically significant (Q = 17.46, 14 df, p = 0.218). This finding indicates that, although preventive psychological interventions for PPD had a statistically significant effect, it was smaller than the effect size considered small according to Cohen's criteria (0.20) (Cohen, Reference Cohen1989). Figure 2 shows the forest plot for the overall and individual effect sizes. All pooled SMDs decreased in the sensitivity analyses, although when only RCTs with a low risk of bias from qualitative criteria were included, the pooled SMD decreased substantially (SMD: −0.101; CI −0.241 to 0.038). See Table 2.

Fig. 2. Forest plot.
Table 2. Effectiveness of psychological interventions to prevent PPD

a The first post-intervention measure assessed after delivery.
b Between-study variance estimate (τ2): 0.000 (95% CI 0.000–0.048).
c Taking the different post-intervention evaluations as the mean.
d The RCT that most increased heterogeneity. Exclusion of RCTs according to the quantitative coding criteria: risk of bias ⩾6.
e Inclusion of RCTs according to the quantitative coding criteria: risk of bias ⩽ 3.
f Exclusion of RCTs according to the qualitative coding criteria: any item (1, 2, 4, 5 or 6) coded as high risk of bias.
g Inclusion of RCTs according to the qualitative coding criteria: all of items (1, 2, 4, 5 and 6) coded as low risk of bias.
h The CI cannot be calculated because the degrees of freedom (n-1) must be at least 2.
Publication bias
Egger's (intercept, −0.42; 95% CI −1.42 to 0.58; p = 0.381) and Beg and Mazumdar's (z = 0.49; p = 0.62) tests to detect publication bias were not statistically significant. The funnel plot (see Fig. 3) was symmetrical, and Duval and Tweedie's trim-and-fill procedure did not impute missing RCTs. Therefore, no statistical evidence for the presence of publication bias was found.

Fig. 3. Funnel plot.
Subgroup analysis, meta-regression and stratified meta-analysis
Subgroup analysis suggested that there was a tendency for greater effectiveness in interventions targeting only primiparous women and women without a previous history of depression. Intervention effectiveness was not associated with age, focus on a specific ethnic minority group, the type of preventive intervention, when the intervention was performed, the intervention orientation or sample size (online Supplementary eAppendix 4).
Unadjusted meta-regressions using standard errors by the Knapp & Hartung method showed that the interventions focused on primiparous women and on women without a previous history of depression were significantly (p < 0.005) associated with higher effectiveness to reduce depressive symptoms. When adjusted for the risk of bias in the meta-regression models, both variables lost statistical significance (online Supplementary eAppendix 5).
The final meta-regression model including one variable explained 100% of the heterogeneity (I 2 residual = 0). Interventions conducted only with primiparous women were significantly associated with higher effectiveness [β- = 0.3304 (95% CI −0.6355 to −0.0253); p = 0.036]. The goodness of fit was good (see online Supplementary eAppendix 6).
The stratified MA according to the variable previous deliveries shows that interventions focused on primiparous women [−0.467 (95% CI −0.737 to −0.083; p = 0.001)] are more effective than interventions focused on primiparous and multiparous women [−0.137 (95% CI −0.205 to −0.069; p < 0.001)] for the random model. Heterogeneity between subgroups was low (I 2 = 21.20%) but statistically significant (Q = 5.47, 1 df, p = 0.019). See online Supplementary eAppendix 7.
Quality of evidence
The initial grading of the quality of evidence was high since only RCTs were included. Heterogeneity was low and there was no publication bias. Although only a small number of studies were included, they were sufficient for the precision of the MA. Indirectness was low since the target population, interventions and outcome did not differ from those of primary interest. Approximately one-third of the RCTs from the quantitative criteria and one-twentieth from the qualitative criteria had a low risk of bias, and the rating therefore decreased from high to moderate.
Discussion
Summary of findings
Psychological interventions had a very small effect on preventing PPD in non-depressed women and this result was robust in the sensitivity analyses. The results from this SR were derived from 17 RCTs, 15 of them included in the MA, carried out in six countries including a total of 4958 participants. There was no evidence of publication bias. Only two RCTs had an overall low risk of bias. Heterogeneity was low and was fully explained by a meta-regression model including one variable: interventions carried out only with primiparous women, which had a statistically significant association with higher effectiveness. The meta-regression stratified by the variable previous deliveries also shows that interventions focused on primiparous women are more effective than those focused on primiparous and multiparous women. According to GRADE, the quality of evidence was moderate.
Comparison with previous research
The overall effect size obtained in this SR/MA was very small. In previous SRs/MAs in the field, the effect size obtained ranged from small to moderate (Cluxton-Keller & Bruce, Reference Cluxton-Keller and Bruce2018; Dennis & Dowswell, Reference Dennis and Dowswell2013; Lin et al., Reference Lin, Xue, Yang, Li and Cao2018; Yasuma et al., Reference Yasuma, Narita, Sasaki, Obikane, Sekiya, Inagawa and Nishi2020). However, these previous SR/MAs included studies involving the participation of women with depression at baseline. Small effect size was also found in a subgroup analysis focused on studies that excluded participants with depression at baseline in one SR/MA in the field (Sockol et al., Reference Sockol, Neill Epperson and Barber2013). Other SRs/MAs focused on preventing depression in different populations in which non-depressed participants at baseline or preventing the onset of depression (Bellón et al., Reference Bellón, Moreno-Peral, Motrico, Rodríguez-Morejón, Fernández, Serrano-Blanco and Conejo-Cerón2015; Conejo-Ceron et al., Reference Conejo-Ceron, Moreno-Peral, Rodriguez-Morejon, Motrico, Navas-Campana, Rigabert and Bellon2017; van Zoonen et al., Reference van Zoonen, Buntrock, Ebert, Smit, Reynolds, Beekman and Cuijpers2014) also showed a small effect size.
Meaning and implications
Given that the results of the present study refer to prevention, despite the small size of the effect found, from a public health perspective the positive impact could be large: the improvement in the health and quality of life of women and their babies and the reduction of costs for society and health services. Therefore, the need to carry out PPD preventive programs through different channels (face-to-face or on-line) are affirmed. Furthermore, the greater efficacy found in interventions focused only on primiparous women rather than on joint interventions with multiparous women, suggest that, if future research confirms this finding, this type of intervention could begin from the first pregnancy of each woman. Being a first-time mother or having more children has been associated with PPD as a risk factor with contradictory results (Hartmann, Mendoza-Sassi, & Cesar, Reference Hartmann, Mendoza-Sassi and Cesar2017; Martínez-Galiano, Hernández-Martínez, Rodríguez-Almagro, Delgado-Rodríguez, & Gómez-Salgado, Reference Martínez-Galiano, Hernández-Martínez, Rodríguez-Almagro, Delgado-Rodríguez and Gómez-Salgado2019). Beyond this, primiparous women and multiparous women usually have different concerns. Primiparous women have to deal with insecurity, need for mastery and role definition, while women that have more children are concerned about how to appropriately divide time between their children (Haga, Lynne, Slinning, & Kraft, Reference Haga, Lynne, Slinning and Kraft2012; Krieg, Reference Krieg2007). Similarly, primiparous women need more support from relatives and healthcare workers (Salarvand, Mousavi, Esmaeilbeigy, Changaee, & Almasian, Reference Salarvand, Mousavi, Esmaeilbeigy, Changaee and Almasian2020). Thus, the different concerns or needs of first-time mothers and multiparous mothers may hold the key to creating differentiated preventive interventions for each, instead of grouping them together. The results from this SR/MA suggest that encouraging preventive interventions focused on primiparous women may be useful to reduce the symptoms or incidence of PPD in non-depressed women, although, due to the small sample of trials focused on primiparous women, this recommendation should be taken with caution.
Strengths and limitations
To the best of our knowledge, this is the first SR/MA to examine the effectiveness of psychological interventions in the prevention of PPD that exclusively included RCTs in which the participants were non-depressed at the study baseline. This SR/MA explored a large number of RCTs from the most relevant databases in the field, as well as extensive supplementary hand searching. Furthermore, the broad range of search terms used and imposing no restrictions on language, setting or publication year contributed to achieving a highly sensitive search. This SR/MA included a reasonable number of participants representing a large population of individuals with different characteristics and from diverse contexts. This study also included a wide spectrum of psychological interventions (including those with psychoeducational and psychosocial approaches) for PPD and implemented by a variety of professionals in different settings. These aspects give the study a wide scope, which supports its external validity. In addition, the strict inclusion criteria, analyzing only RCTs with a study population free from depression at baseline, allowed us to distinguish prevention effectiveness from treatment effectiveness. Study selection, data extraction and risk of bias assessment were performed by trained, independent reviewers, achieving good inter-observer reliability. We applied a rigorous methodology to conduct the SR/MA process and to evaluate the quality of the evidence. The absence of publication bias and the low heterogeneity, which is fully explained through the meta-regression model, as well as the moderate quality of evidence, support the robustness of the pooled SMD obtained.
Several limitations should be considered when interpreting the results. First, most of the RCTs included were conducted in high-income countries, so the inferences should be limited to these types of countries. Second, the duration of follow-up only extends to the end of the postpartum year in six of the 17 RCTs included. Therefore, conclusions cannot be drawn about effectiveness throughout the entire postpartum period. Third, the number of RCTs in each subgroup category was low; in these cases, the lack of statistical power precludes definitive conclusions. Fourth, there were only two RCTs with an overall low risk of bias, and in these, the effect size was irrelevant. Thus more trials with a low risk of bias are needed. Finally, although some studies measured PPD results with standardized clinical interviews, in six RCTs the reduction in PPD symptoms measured by scales was the only outcome, even though standardized diagnostic interviews generally have greater validity.
Future research
This SR/MA suggested that psychological interventions that aim to prevent PPD in non-depressed women have questionable effectiveness. This effectiveness tends to be greater in interventions focused solely on primiparous women. However, given the small number of RCTs that have been conducted exclusively with primiparous women, further research focused on this target population is needed. In addition, only two RCTs had an overall low risk of bias, indicating the need to conduct more trials with low risk of bias, paying attention to the attrition bias as it is frequent in the studies analyzed. Similarly, given that women are most susceptible to developing PPD during the 12 months after giving birth (American College of Obstetricians and Gynecologists Committee on Health Care for Underserved Women, 2018; Gavin et al., Reference Gavin, Gaynes, Lohr, Meltzer-Brody, Gartlehner and Swinson2005; O'Hara & McCabe, Reference O'Hara and McCabe2013; Yim et al., Reference Yim, Tanner Stapleton, Guardino, Hahn-Holbrook and Dunkel Schetter2015), future research should involve booster sessions and evaluations through the end of the first year postpartum as, to date, few RCTs have done this. Moreover, only three RCTs have used the internet to deliver interventions. Today, when almost everything can be done using the mobile phone, online interventions to prevent PPD could be a very feasible option. Furthermore, online psychological and psychoeducational interventions to prevent depression have been shown to be effective (Rigabert et al., Reference Rigabert, Motrico, Moreno-Peral, Resurrección, Conejo-Cerón, Cuijpers and Bellón2020). Perinatal women also appear to be open to receiving preventive PPD interventions delivered online (Osma, Suso-Ribera, Martínez-Borba, & Barrera, Reference Osma, Suso-Ribera, Martínez-Borba and Barrera2020), and e-mental health applications have been assessed by health professionals as very useful in maternal depression (Sprenger, Mettler, & Osma, Reference Sprenger, Mettler and Osma2017). This format would also prevent interruption of the intervention (as would happen in a face-to-face intervention) during unforeseen events such as the current global pandemic (Van Daele et al., Reference Van Daele, Karekla, Kassianos, Compare, Haddouk, Salgado and De Witte2020). Additional research into this format is therefore encouraged. Finally, there is also a need for further RCTs that assess the incidence of new cases of PPD through standardized diagnostic interviews.
Supplementary material
The supplementary material for this article can be found at https://doi.org/10.1017/S0033291722000071
Acknowledgements
We thank Jaewoo Sung for helping us to translate Korean articles, as well as Dr Patricia Trautmann-Villalba for doing the same with the articles in German. Furthermore, we would like to thank the authors from the included RCTs who replied to our data request in order to conduct the meta-analysis.
Author contributions
CMG and EMM designed the study, and PMP, JAB, SCC, HCP, IGG, AR and IB collaborated on the design. CMG drafted the manuscript, and EMM, PMP, JAB, SCC, IGG, AR, IB and HCC conducted a critical revision of the manuscript for important intellectual content. CMG and HCP independently screened the potential studies and together with SCC extracted the data. CMG, PMP and SCC assessed the risk of bias and completed the data synthesis. CMG, IGG, PMP and JAB performed the analysis. CMG, PMP, JAB, SCC, HCP, IGG, AR, IB and EM, read, provided feedback, discussed and approved the final manuscript.
Financial support
This study was supported by Carlos III Health Institute, through the Primary Care Prevention and Health Promotion Network (redIAPP, RD12/0005/0001; RD16/0007/0001), and by the EU ERDF funds (European Regional Development Fund).
Conflict of interest
None.








