Summations
-
∙ This meta-analysis included eight high-quality randomised controlled trials.
-
∙ The effect of low-frequency repetitive transcranial magnetic stimulation on Parkinson’ disease was assessed.
-
∙ No language or year limitation was imposed.
Considerations
-
∙ Low-frequency repetitive transcranial magnetic stimulation (rTMS) had good effect on motor signs in Parkinson’s disease (PD).
-
∙ Low-frequency rTMS might be more appropriate than hight-frequency rTMS on treating PD.
-
∙ Future studies should be focus on the optimal stimulation parameters.
Introduction
Parkinson’s disease (PD) is a progressive neurodegenerative disease that predominantly affects elderly people, and thus it tends to be more prevalent as the population ages (Reference Fahn1). The number of individuals affected by PD is expected to double by 2030 (Reference Dorsey, Constantinescu and Thompson2). But the neural mechanisms that underlie levodopa-induced dyskinesias in PD are still unclear (Reference Rascol, Brooks, Korczyn, Deyn, Clarke and Lang3). Currently, the substitution of dopamine remains the primary therapy, but the degeneration of nondopaminergic neurons lead to the emergence of symptoms refractory to conventional therapy (Reference Benninger, Berman and Houdayer4). Among them, difficulties with gait and recurrent falls are common and cause disability in advanced PD.
Up to now, researchers have developed various pharmacological and non-pharmacological approaches to overcome these difficulties, such as istradefylline (Reference Zhu, Wang and Li5) and repetitive transcranial magnetic stimulation (rTMS). Istradefylline has been approved in March 2013 for manufacturing and market in Japan (Reference Dungo and Deeks6). rTMS has been studied as a potential treatment in many neurological and psychiatric disorders (Reference Chen, Liu and Zhu7,Reference Chen, Zhou and Wu8). Moreover, deep brain stimulation, which was one of treatment long before pharmacological treatment of PD and later seemed obsolete, was explored again. Some previous controlled clinical trials indicated that high-frequency (>1 Hz) rTMS could successfully apply as a potential therapy in PD (Reference Khedr, Rothwell, Shawky, Ahmed and Hamdy9,Reference Lomarev, Kanchana, Bara-Jimenez, Iyer, Wassermann and Hallett10). And one meta-analysis published in 2009 also confirmed the benefit of high-frequency rTMS on motor performance in PD (Reference Elahi, Elahi and Chen11). In regards to low-frequency (≤1 Hz) rTMS, it was unclear whether this method could produce superior effects, as randomised controlled trials (RCT) that have explored the relative efficacies of this method and sham stimulation have shown inconsistent results. For example, Shirota et al. reported that low-frequency rTMS had better efficacy than sham stimulation for motor symptoms in PD (Reference Shirota, Ohtsu, Hamada, Enomoto and Ugawa12). But Okabe et al. reported that low-frequency rTMS and sham stimulation had comparable efficacy for motor symptoms in PD (Reference Okabe, Ugawa and Kanazawa13). The aforementioned meta-analysis concluded that low-frequency had little effect on motor signs in PD (Reference Elahi, Elahi and Chen11). But this conclusion was obtained by only pooled analysing two non-RCTs. The statistical power was relatively low. Recently, several high-quality RCTs on low-frequency rTMS in PD had been published (Reference Shirota, Ohtsu, Hamada, Enomoto and Ugawa12,Reference Niu and Gou14,Reference Wang, Gu and Ma15). Therefore, there was an urgent need for additional systematic review to reassess the efficacy of low-frequency rTMS for motor symptoms in PD.
Methods
Search strategy
Relevant international databases (PubMed, CCTR, Embase, and Web of Science), two Chinese databases (CNKI and CBM-disc), two grey databases (NTIS and EAGLE), and relevant websites (Clinical Trials, Current Controlled Trials, International Clinical Trials Registry) were searched up to June 2014, with different combinations of the following keywords: ‘Parkinson’ or ‘PD’ and ‘transcranial magnetic stimulation’ or ‘TMS’ or ‘RTMS’ or ‘noninvasive brain stimulation’. No language or year limitation was imposed. In order to avoid omitting relevant clinical trials, we scanned conference summaries and reference lists of articles identified in the initial searches, and contacted authors to obtain additional information for relevant trials.
Selection criteria
Among the articles identified in the initial search, only those meeting the following criteria were selected for subsequent analysis:
-
(i) Prospective clinical studies included patients met the United Kingdom Parkinson’s Disease Society Criteria (UKPDSC) (Reference Hughes, Ben-Shlomo, Daniel and Lees16).
-
(ii) PD patients over 18 years old could give written informed consent.
-
(iii) Patients without depending with drug or alcohol and taking any excluded medications.
-
(iv) Effect size was assessed by the motor section of Unified Parkinson’s Disease Rating Scale (UPDRS part III).
-
(v) Must have a control group.
Data extraction
Two reviewers independently verified all potentially suitable clinical trials by the aforementioned inclusion criteria in addition to the completeness of data abstraction. Any disagreements were resolved by discussion. The data about the first author, the publication year, sample size, stimulation frequency, stimulation site, stimulation time, the total number of pulse, UPDRS part III score and so on were extracted. Results were summarised in a standard summary data sheet. For data that could not be directly obtained, good faith efforts were applied to obtain the missing data by dispatching e-mails to the author and researching other studies citing the trial in question.
Bias risk in individual studies
Two reviewers independently assessed the quality of each eligible clinical trial according to the Cochrane Collaboration criteria (Reference Higgins and Altman17). Bias risk was determined by: (1) outcome blinding assessment; (2) allocation concealment; (3) incomplete outcome data reporting; (4) randomisation quality and (5) baseline clinical characteristics matched. Studies with three or more bias risks were excluded from the meta-analysis.
Statistical analysis
RevMan5.1 software (Cochrane Information Management System [IMS]) was used to do meta-analysis. Effect size (d) and 95% confidence intervals (CI) were calculated. Effect size was the magnitude of a treatment effect and was calculated as the difference in scores between treatment and control groups divided by the standard deviation of the scores. Mantel–Haenszel random-effects model was used, as it was assumed that the included studies probably had varying true treatment effects (Reference Riley, Higgins and Deeks18). Meanwhile, fixed-effect model was also used to obtain a robust conclusion. When necessary, sensitivity and subgroup analysis was conducted. Heterogeneity was evaluated using the χ2-based Q test (p<0.10) and I-squared index (I2) (I2>50%) (Reference Higgins, Thompson, Deeks and Altman19). Publication bias was evaluated with the Egger regression test. Significance was set at p<0.05, unless otherwise stated. This meta-analysis was performed according to the recommendations of Sacks et al. (Reference Sacks, Berrier, Reitman, Ancona-Berk and Chalmers20).
Results
Selected studies
We performed a systematic review of the available literature according to the preferred reporting items for systematic reviews and meta-analyses guidelines. The initial electronic literature search yielded 336 potentially relevant studies from scientific and medical databases and relevant websites. 326 studies were included after removing the 10 duplicates. Among these 326 studies, 304 studies were excluded after carefully and strictly reviewing titles and abstracts. By scanning the full text of the rest of 22 studies, 14 studies were removed according to the aforementioned inclusion criteria. The articles were excluded because of the following reasons: (1) case report or review (79 studies); (2) duplicated publications (10 studies); (3) no control group (57 studies); (4) the effect size was not assessed by UPDRS (28 studies); (5) non-randomised trial (42 studies); (6) the publications were dealt with other topics (112 studies). Finally, eight RCTs would be used for subsequent pooled analysis (Reference Shirota, Ohtsu, Hamada, Enomoto and Ugawa12–Reference Wang, Gu and Ma15,Reference Shimamoto, Takasaki, Shigemori, Imaizumi, Ayabe and Shoji21–Reference Zhong, Shimamoto and Shigemori24). The selection process is shown in Fig. 1. Although references from these studies were researched for possibly omitted RCTs, no more RCTs were found.
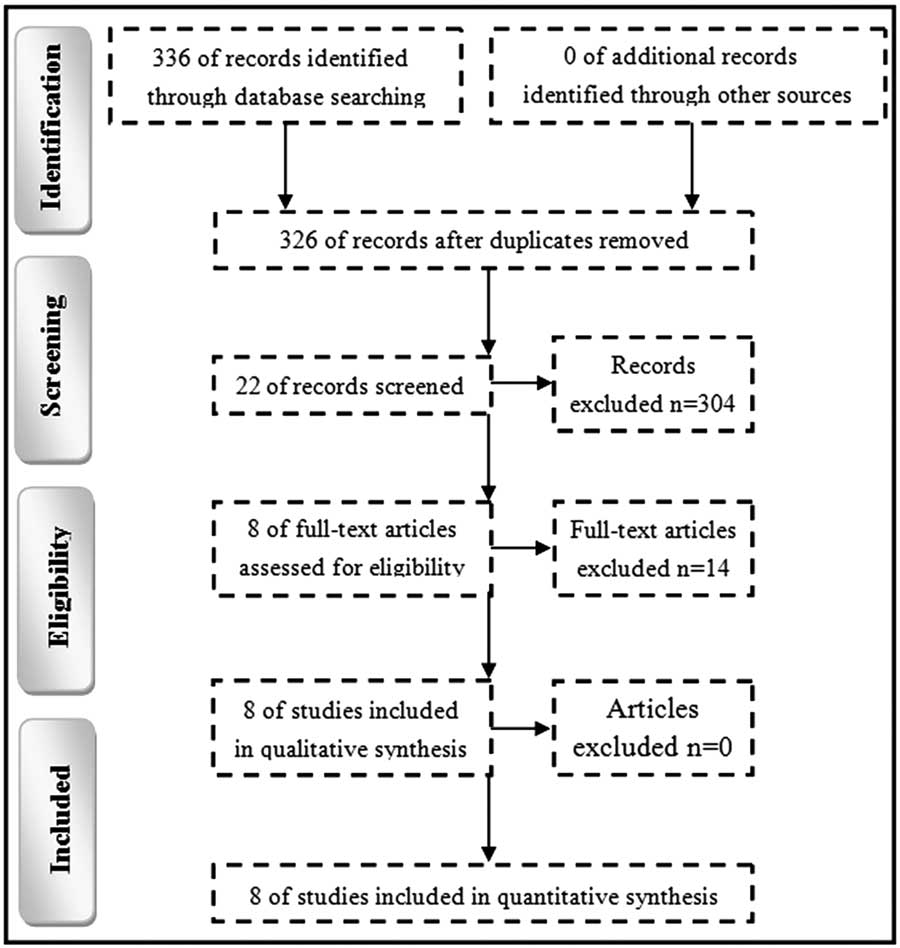
Fig. 1 Workflow of literature search.
Main characteristics
These eight RCTs contained an aggregate of 319 adult patients, composed of 145 patients receiving sham rTMS and 174 patients receiving real rTMS. Patients in four RCTs were from China, three RCTs recruited patients from Japan, and one RCT recruited patients from Italy. There were no differences in sex, mean age and mean UPDRS part III score. The rTMS was performed as an add-on therapy for most patients. Five RCTs used 1 Hz and three RCTs used 0.2 Hz. The detailed characteristics of the included RCTs are described in Tables 1 and 2. Among the seven studies using add-on treatment method, all subjects were consented to maintain antiparkinson medications, such as dopamine agonist and levodopa throughout the trial, and intervention was performed at the same time of day for each patient. Meanwhile, five studies reported that antiparkinsonian medications were used before rTMS were continued throughout the study (Reference Okabe, Ugawa and Kanazawa13–Reference Wang, Gu and Ma15,Reference Zhang, Dai, Su and Luo23,Reference Zhong, Shimamoto and Shigemori24). Four studies reported that the patients stopped using dopaminergie drugs for at least 12 h before each assessment (Reference Niu and Gou14,Reference Wang, Gu and Ma15,Reference Zhang, Dai, Su and Luo23,Reference Zhong, Shimamoto and Shigemori24) and one reported that all assessments were performed in the ‘on’ state at the same time of the day for each patient (Reference Shimamoto, Takasaki, Shigemori, Imaizumi, Ayabe and Shoji21).
Table 1 Clinical characteristic of patients in real-rTMS group

APM, antiparkinson medications; F, female; M, male; NA, not available; rTMS, repetitive transcranial magnetic stimulation; UPDRS, Unified Parkinson’s Disease Rating Scale.
Table 2 Parameters of real-rTMS

C, circular; d, day; D, double; DLPFC, dorsolateral prefrontal cortex; F, frequency; F8, figure of eight; L, left; m, month; M1, motor cortex; MT, motor threshold; NA, not available; R, right; rTMS, repetitive transcranial magnetic stimulation; SMA, supplementary motor area; T, Tesla; w, week.
Bias risk assessment
All eight included RCTs were randomised, reported incomplete data, and reported similar baseline characteristics. Five RCTs unequivocally reported allocation blinding, and five RCTs unequivocally reported outcomes of their blinding assessment. As these eight RCTs displayed minimal or no bias risk, the data from all eight studies were included in this meta-analysis (Table 3).
Table 3 Risk of bias of the included studies

B, allocation; C, blinding assess; D, incomplete data; E, baseline; N, no risk of bias; NA, not available; R, randomisation.
UPDRS III score meta-analysis
The pooled mean effect size estimate (d) was calculated using direct weights defined as the inverse of the variance of d for each study/stratum, which was −0.40 (95% CI=−0.73 to −0.06, p<0.05) for the random effect model and −0.34 (95% CI=−0.57 to −0.11, p<0.05) for the fixed effect model (Fig. 2). Therefore, with the random effects model, the true effect size was at least 0.40 lower in the treatment groups compared with the control groups. This was equivalent to a 5.05 (95% CI=−1.73 to −8.37) point decrease in UPDRS part III score in the random and fixed effect models. Moderate heterogeneity in effect size was existent (p=0.07, I2=47%). There was no significant asymmetry in the inverted funnel plots of the selected RCTs. Considering the number of selected RCTs may not have provided enough power to show a clear asymmetry, the Egger’s test was performed. This test showed that the primary outcome (p=0.24) was not influenced by publication bias.

Fig. 2 Unified Parkinson’s Disease Rating Scale (UPDRS) part III score meta-analysis.
Sensitivity analysis
Shimamoto et al. reported total UPDRS but not motor UPDRS (Reference Shimamoto, Takasaki, Shigemori, Imaizumi, Ayabe and Shoji21), which was our main outcome of interest. Therefore, we removed this RCT to perform sensitivity analysis. The pooled mean effect size was −0.32 (95% CI=−0.64 to −0.00, p<0.05) for the random effect model and −0.29 (95% CI=−0.53 to −0.06, p<0.05) for the fixed effect model. Therefore, with the random effects model, the true effect size was at least 0.32 lower in the treatment groups compared with the control groups. Moreover, significant heterogeneity in effect size was non-existent (p=0.12, I2=41%).
Subgroup analysis
We performed subgroup analysis according to the different countries (Fig. 3). Among the included eight RCTs, four RCTs were from China and three RCTs were from Japan. The pooled mean effect size of RCTs from China was −0.44 (95% CI=−0.77 to −0.12, p<0.05) for the random effect model. Therefore, with the random effects model, the true effect size was at least 0.44 lower in the treatment groups compared with the control groups. The pooled mean effect size of RCTs from Japan was −0.31 (95% CI=−1.03 to 0.41, p>0.05) for the random effect model. Therefore, in this subgroup, the results showed no significant reduction in motor UPDRS between rTMS group and control group.

Fig. 3 Subgroup analysis of different countries.
We performed subgroup analysis according to the different coil type (Fig. 4). Among the included eight RCTs, five RCTs were used the coil type of F8 and three RCTs were used the coil type of C. The pooled mean effect size of RCTs used F8 coil type was −0.45 (95% CI=−0.74 to −0.16, p<0.05) for the random effect model. Therefore, with the random effects model, the true effect size was at least 0.45 lower in the treatment groups compared with the control groups. The pooled mean effect size of RCTs used C coil type was −0.36 (95% CI=−1.17 to 0.45, p>0.05) for the random effect model. Therefore, in this subgroup, the results showed no significant reduction in motor UPDRS between rTMS group and control group.

Fig. 4 Subgroup analysis of different coil type.
Discussion
PD is a slowly progressive neurodegenerative disorder affecting up to 1% of the elderly population. As the second most common neurodegenerative disease after Alzheimer’s dementia (Reference de Lau and Breteler25), PD is a major global economic burden that will be increasing with the ‘aging’ of our society. rTMS, as a promising non-pharmacological approach for PD, has been studied by many researchers. Previous meta-analysis has concluded that high-frequency rTMS could significantly reduce motor signs in PD patients. [11] Our study confirmed that low-frequency rTMS also could exert a significant effect on motor function in PD patients. The pooled mean effect size of UPDRS part III was −0.40 with 95% CI=−0.73 to −0.06 (p<0.05), which indicated that low-frequency rTMS could have 5.05 (95% CI=−1.73 to −8.37) point decrease in UPDRS part III score than control group. This conclusion was obtained from pooled analysing eight RCTs composed of 319 patients. However, this conclusion should be interpreted with caution owing to the limited number of RCTs.
The efficacy of rTMS was tied to its stimulus parameters (Reference Xie, Chen and Wei26). One of important parameter was stimulation frequency. Previous studies have suggested that high-frequency rTMS presumably increased the excitability of the stimulated cortex, but low-frequency rTMS presumably decreased it (Reference Fitzgerald, Fountain and Daskalakis27). Moreover, rTMS with different stimulus frequencies exerted different modulations at a network level (Reference Eldaief, Halko, Buckner and Pascual-Leone28). Some studies reported that high-frequency rTMS had potential adverse effects (Reference Wassermann29,Reference Chen, Gerloff, Classen, Wassermann, Hallett and Cohen30), including induction of seizures, this might limit the wide spread clinical use of high-frequency rTMS. On the other hand, low-frequency rTMS appeared to be better tolerated, that was, patients reported less headaches, and might also minimise the risk of inducing adverse events such as seizures (Reference Schutter31). Therefore, low-frequency rTMS might be a more acceptable treatment for PD than high-frequency rTMS. Of course, this hypothesis was needed future large-scaled RCTs that directly compared the efficacy of high-frequency rTMS and low-frequecny rTMS to verify. Another important parameter was stimulation site because many brain regions were involved in PD (Reference Eidelberg32). At present, most studies have targeted the dorsolateral prefrontal cortex or primary motor cortex. The supplementary motor area (SMA) was less used, even though some studies reported the involvement of the SMA in PD (Reference Playford, Jenkins, Passingham, Nutt, Frackowiak and Brooks33,Reference Sabatini, Boulanouar and Fabre34). Meanwhile, the total pulse was also the important parameters. Although no guidelines have been established as to the number of total pulse in rTMS, recently studies showed a tendency towards a greater number of total pulses. A meta-analysis of stimulus parameter effects showed that rTMS with ⩾1200 daily stimuli had a better efficacy than rTMS with <1200 daily stimuli (Reference Xie, Chen and Wei26). Moreover, the subgroup analysis of different coil type showed that the rTMS with the coil type of F8 yielded significant reduction in motor UPDRS, but not the rTMS with the coil type of C. Our findings will be helpful for future studies to investigate optimum protocol of rTMS in treating PD.
Elahi et al. reported that low-frequency rTMS had little effect on motor signs in PD (Reference Elahi, Elahi and Chen11). They only analysed two non-RCTs to obtain a pooled effect size of −1.86 (p=0.62) in a random effects model for low-frequency rTMS treatment. But, in our study, we obtained a different conclusion that low-frequency rTMS could exert a significant effect on motor function in PD patients. This conclusion was obtained by pooled analysing eight RCTs. The more and higher-quality literature made our conclusion more robust.
A few limitations to this meta-analysis should be mentioned here. First, a relatively small sample size of PD patients in a limited number of clinical trials was included. Second, the long-term antidepressant effects and cost-effectiveness of rTMS could not be assessed here (Reference Wassermann and Zimmermann35). Third, the other rTMS parameters in the included studies were not precisely identical, which might influence our results. Fourth, as the method of locating stimulation site has been recently criticised for its inaccuracy (Reference Rosa and Lisanby36), future rTMS studies should take advantage of neuronavigation approaches (Reference Schönfeldt-Lecuona, Lefaucheur, Cardenas-Morales, Wolf, Kammer and Herwig37).
Conclusion
Several factors, such as cost and limited availability of the devices to specialised centers, skilled personnel, less knowledge about long-term side-effects, limited the wide spread clinical use of therapeutic rTMS. However, our results showed that low-frequency rTMS was a promising add-on therapy for motor symptoms of PD. Meanwhile, a large-scaled RCT with appropriate follow-up would be helpful for researchers to define its role in the treatment of PD. Future studies were also needed to find out the optimal stimulation parameters and the effects of rTMS on other aspects of PD, especially memory.
Acknowledgement
The authors thank Min Liu from The Chinese Cochrane Center for retrieving the studies for this review.
Financial Support
This research received no specific grant from any funding agency, commercial or not-for-profit sectors.
Conflicts of Interest
None.










