Introduction
Schizophrenia is a longstanding condition affecting 1% of the population with the majority of patients experiencing multiple relapses during the course of the condition (Emsley, Chiliza, Asmal, & Harvey, Reference Emsley, Chiliza, Asmal and Harvey2013; Rössler, Salize, Os, & Riecher-Rossler, Reference Rössler, Salize, Os and Riecher-Rossler2005), and most relapses tend to occur during the early stage of the condition (Chan et al., Reference Chan, So, Hui, Chang, Lee, Chung and Chen2015; Hui et al., Reference Hui, Tang, Leung, Wong, Chang, Chan and Chen2013). Relapses have a significant impact on the outcomes of patients. Studies have shown that early relapses are associated with increasing suicide mortality (Chan et al., Reference Chan, Chan, Pang, Yan, Hui, Chang and Chen2018) and poor long-term trajectories of employment (Chan et al., Reference Chan, Pang, Yan, Hui, Suen, Chang and Chen2020). About one in six patients was found to exhibit protracted impairment after relapse (Emsley et al., Reference Emsley, Chiliza, Asmal and Harvey2013). Longitudinal neuroimaging studies further provide evidence on the neuro-deterioration associated with relapse (Andreasen, Liu, Ziebell, Vora, & Ho, Reference Andreasen, Liu, Ziebell, Vora and Ho2013; van Haren et al., Reference van Haren, Hulshoff Pol, Schnack, Cahn, Mandl, Collins and Kahn2007). Relapses also carry a significant economic burden to society (Pennington & McCrone, Reference Pennington and McCrone2017). Therefore, identification of risk factors of relapse and providing effective relapse prevention intervention are critical to the long-term management of patients with schizophrenia.
Many studies have reported demographic and clinical related risk factors of relapses in patients with schizophrenia. These include medication non-adherence (Alvarez-Jimenez et al., Reference Alvarez-Jimenez, Priede, Hetrick, Bendall, Killackey, Parker and Gleeson2012), smoking (Hui et al., Reference Hui, Tang, Leung, Wong, Chang, Chan and Chen2013), older paternal age (Hui et al., Reference Hui, Chiu, Li, Law, Chang, Chan and Chen2015), and cognitive functions such as visual working memory (Hui et al., Reference Hui, Li, Li, Lee, Chang, Chan and Chen2016). Despite medication, non-adherence has been found to be the most significant clinical predictors of relapse (Caseiro et al., Reference Caseiro, Pérez-Iglesias, Mata, Martinez-Garcia, Pelayo-Teran, Tabares- Seisdedos and Crespo-Facorro2012), about 50% of patients relapsed while having good adherence to medication (Linszen et al., Reference Linszen, Dingemans, Nugter, Van der Does, Scholte and Lenior1997). Environmental, particularly family-related factors, is also important. One factor that has been examined extensively is caregiver expressed emotion (EE). The construct of EE was developed in the 1950s and it comprised four domains: critical comments (CC), hostility, emotional overinvolvement (EOI), and warmth (Amaresha & Venkatasubramanian, Reference Amaresha and Venkatasubramanian2012; Hooley & Parker, Reference Hooley and Parker2006). The role of caregiver or family EE in predicting patient relapse has been reported in many studies and has been suggested as a major predictor of relapse in both patients with first-episode and longstanding conditions in an early study (Linszen et al., Reference Linszen, Dingemans, Nugter, Van der Does, Scholte and Lenior1997).
An earlier meta-analysis study concluded that high EE is associated with approximately one-third of relapses in patients with schizophrenia (Butzlaff & Hooley, Reference Butzlaff and Hooley1998) and appears to be more prominent in patients with longstanding schizophrenia. As cultural variation may be contributed to the degree and manifestation of the EE domains, and there is a possible differential association between EE and relapse with a different culture (Kopelowicz et al., Reference Kopelowicz, Zarate, Gonzalez, Lopez, Ortega, Obregon and Mintz2002), a more recent meta-analysis specifically looks into the cross-cultural effect of the relationship between EE and relapse. The study, however, revealed no significant cultural variation of EE and the link between EE and relapse appeared to be universal among the population of a different culture (O'Driscoll, Sener, Angmark, & Shaikh, Reference O'Driscoll, Sener, Angmark and Shaikh2019). This result is similar to the earlier meta-analytic study with much less studies included, that is no regional differences were found (Butzlaff & Hooley, Reference Butzlaff and Hooley1998). However, both of these reviews suffered from some limitations. Methodologically, these meta-analyses included a noticeable amount of experimental studies that restricted the pooled effect estimation. The power issue of the included studies, as well as attrition bias, were not considered, and their findings on the moderators of the EE-relapse association were inconsistent. Furthermore, only studies using Camberwell Family Interview (CFI) (Vaugh & Leff, Reference Vaugh and Leff1976) as EE measurement were considered without taking consideration of studies using other valid EE instruments such as 5-min Speech Sample (FMSS) (Magana et al., Reference Magana, Goldstein, Karno, Miklowitz, Jenkins and Falloon1986), and Level of Expressed Emotion Scale (LEES) (Cole & Kazarian, Reference Cole and Kazarian1998). The understanding of specific roles of the individual domains of EE in relationship with relapse and time of relapse could inform the development of future intervention and yet this was not explored.
In order to fill these research gaps and overcome the limitations of previous reviews, we systematically evaluate the literature to examine the global EE-relapse association by the timing of relapse, EE domain-relapse association, and its putative effect moderators. Studies with all valid EE measures were included. Results of this meta-analysis can provide a comprehensive understanding of the relationship between EE and relapse in patients with schizophrenia, and inform the development of the family-focused intervention.
Methods
Search strategy
Potential research articles, grey literatures, and ongoing studies were identified from eight databases including Web of Science Core Collection (1956–2020), PsycINFO (1806–2020), MEDLINE (1946–2020), EMBASE (1947–2020), CENTRAL (1908–2020), CNKI (1984–2020), Airiti Library (1991–2020), ProQuest Dissertation & These A&I (1743–2020), and two trial registries, ClinicalTrials.gov (1997–2020) and ICTRP (2004–2020). The prespecified search terms used were (expressed emotion OR EE OR emotional over involvement OR EOI OR hostile OR hostility OR critical comments OR criticism OR warmth OR positive regards OR Camberwell Family Interview OR CFI) AND ti(relapse OR readmission OR rehospitalisation OR exacerbation OR course) AND ti(schizophrenia OR schizo* OR psychosis OR psychotic OR psychiatric). The search was conducted from the inception dates of the databases to May 2020 and it was limited to English and Chinese languages. We also searched the bibliography of the identified articles for more eligible research. This review was prospectively registered in PROSPERO (CRD42020173218) and was reported in line with the PRISMA checklist (Moher, Liberati, Tetzlaff, & Altman, Reference Moher, Liberati, Tetzlaff and Altman2009).
Inclusion and exclusion criteria
We used the PEO framework to screen and select the eligible studies (Moola et al., Reference Moola, Munn, Tufanaru, Aromataris, Sears, Sfetc, Mu, Aromataris and Munn2017). Studies with at least half of the patients diagnosed with schizophrenia-spectrum disorders using any valid diagnostic methods and are living or in close contact with families were included. The included studies used any valid EE measurements that allowed categorisation of the population into high EE (HEE) or low EE (LEE), and relapse events of patients in a specific time frame by EE groups were reported. In addition, we included prospective cohort studies, while experimental studies were excluded to prevent the pooled effect estimate being contaminated by the treatment allocation.
Data extraction and management
Two researchers (CFM & YLC) independently conducted a systematic literature search. All identified studies were cross-checked and the consensus was reached for any disagreement. Important study characteristics, including study geographical location, number of subjects, patients' age, length of the condition, EE measures, relapse measures, time of follow-up, attrition rate, number of relapses, and study methodological quality, were extracted and tabulated. If the length of condition was not readily available in the report, the number of prior hospitalisations was used instead. Patients with less than 5 years of onset or three prior hospitalisations would be categorised into the recent-onset group, while the remaining would be categorised into longstanding type (Butzlaff & Hooley, Reference Butzlaff and Hooley1998). The attrition rate was calculated as the loss of follow-up of the original recruited sample. Relapse events were extracted according to the operational definition of relapse in the respective studies. Besides, the timing of relapse was divided into early relapse and late relapse. Early relapse referred to relapse occurred on or before 12-month follow-up, while late relapse referred to relapse occurred after 12-month follow-up. Data extracted were cross checked by the two researchers.
Risk of bias (RoB) assessment
Two researchers (CFM & YLC) independently carried out the bias assessment. The results were cross-checked and the consensus was reached for any disagreement. Joanna Briggs Institute Critical Appraisal Checklist for Cohort Studies was used to assess the risk of bias across the studies (Moola et al., Reference Moola, Munn, Tufanaru, Aromataris, Sears, Sfetc, Mu, Aromataris and Munn2017). This eleven-item scale addresses the selection bias, information bias, misclassification bias, confounding control measures, and other important methodological issues. In parallel, STROBE Statement was used to complement the overall bias assessment (vom Elm et al., Reference vom Elm, Altman, Egger, Pocock, Gotzsche and Vandenbroucke2007). Overall low, moderate, and high RoB was determined for each study to categorise the methodological quality across studies. We graded studies with small sample size (i.e. N < 60) or high attrition rate (i.e. >20%) without appropriate imputation methods as having moderate RoB, because of the possible presence of Type II error (Akl et al., Reference Akl, Briel, You, Sun, Johnston, Busse and Guyatt2012).
Putative moderators
Apart from the covariates reported in the previous meta-analyses including the length of the condition, study geographical location and time of the study, other factors including patients' age, culture, EE measures, the proportion of schizophrenia sample, and study quality were also added as covariates in the moderator analysis of the current study. The culture was broadly grouped into Western and Eastern culture (Dwairy & Achoui, Reference Dwairy and Achoui2010a, Reference Dwairy and Achoui2010b). EE measures were categorised into CFI and other validated instruments (non-CFI). Study quality was grouped into low, moderate, and high RoB. Publication year was divided into two groups using the publication year of 1998 as a cutoff as this was the publication year of the first meta-analysis of the impact of EE on relapse of patients with schizophrenia (Butzlaff & Hooley, Reference Butzlaff and Hooley1998).
Statistical analysis
Spearman correlation test was used to examine the relationship between study methodological quality, attrition rate, and publication year. In the meta-analysis, we used random-effects model with inverse-variance weighting method to pool the effect estimates in odds ratio (OR) and 95% confidence interval (CI), as the studies were heterogeneous in terms of sociodemographic factors and selection of the outcome measures. Since random-effects model would unavoidably add more weight to the small studies, sensitivity analyses were conducted on the overall pooled effect estimate by removing the small studies and studies with high RoB. In addition, the pooled effect estimates by follow-up period and EE subscales were further analysed. EE subscales consisted of CC, EOI, hostility, and warmth. Multiple random-effects meta-regression was conducted to examine the association between study characteristics and the effect estimates. OR and 95% CI were imputed by anti-logging the β and the product of 1.96 and standard error (Bland & Altman, Reference Bland and Altman2000). Leave-one-out sensitivity analysis and cumulative analysis by chronological order were performed to ensure the stability of pooled effect estimates from individual studies and across publication periods, respectively. Lastly, to examine the publication bias or small-study effect for pooled dichotomous outcomes with between-study variances, tau-squared (τ2) > 0.01, funnel plot followed by arcsine test and trim-and-fill procedure were conducted (Higgins et al., Reference Higgins, Thomas, Chandler, Cumpston, Li, Page and Welch2020; Rucker, Schwarzer, & Carpenter, Reference Rucker, Schwarzer and Carpenter2008).
R Studio version 1.3.959 (RStudio Team, 2020), RevMan version 5.3 (Review Manager, 2014), and Open Meta-analyst version 12.11.14 (OpenMetaAnalyst, 2014) were used to carry out statistical inference and produce graphs including forest plots and funnel plot. With-in study and between-study variances could be observed by the CI width and tau-squared (τ2), while study heterogeneity and subgroup difference were determined if p was < 0.05 in Chi-squared (χ2) test and I-squared (I 2) was greater than fifty percentages (Higgins et al., Reference Higgins, Thomas, Chandler, Cumpston, Li, Page and Welch2020). To avoid Type I error caused by multiple testing, the null hypothesis in moderator analysis was rejected if both p values from Omnibus test and regression were smaller than 0.05.
Results
Study selection
The search was conducted between 1 April 2020 and 31 May 2020. PRISMA diagram (Fig. 1) shows the study selection process. In total, 33 studies comprising 38 research reports were identified and included in descriptive synthesis, while 30 studies were meta-analysed/meta-regressed on the relapse outcome and effect moderators. Three studies were excluded from the meta-analysis because the authors did not report relapse events and/or the relapse events could not be imputed and pooled. In total, 19 studies were excluded due to reasons including not cohort design (k = 14), <50% patients diagnosed with schizophrenia (k = 2), <50% patients living with families (k = 2), and patients comorbid with substance abuse (k = 1).

Fig. 1. PRISMA diagram showing the process of studies selection.
Sample and study characteristics
Table 1 summarised the characteristics of included studies. In total, 2284 patients participated in the 33 studies from 21 countries. There were 61.7% male (k = 29, N = 1175) and 55.5% of the patients were unemployed (k = 7, N = 253) with mean age of 30.8 (k = 27, s.d. = 6.5, range = 16.4–39.0). Of the total, 54.5% studies recruited patients with longstanding condition (k = 18), 66.7% studies were from Western countries (k = 22) and nearly half of these were from UK (k = 5) and USA (k = 5). The mean sample size was 69.2 (s.d. = 28.5, range = 15–134). The average follow-up duration was over a year (mean = 15.5 months, s.d. = 13.8, range = 6–84), and the attrition rate was sizable (mean = 11.3%, s.d. = 11.6%, range = 0%–39.7%). Intotal, 26 (78.8%) studies used CFI as the EE measure, while relapse measures varied among studies with four main approach including using valid instruments, clinical consultation, rehospitalisation, or mixture of these, in which 15.2% of the studies (k = 5) adopted rehospitalisation as the only relapse indicator.
Table 1. Summary of longitudinal cohort studies examining the association of global EE and relapse of people with schizophrenia
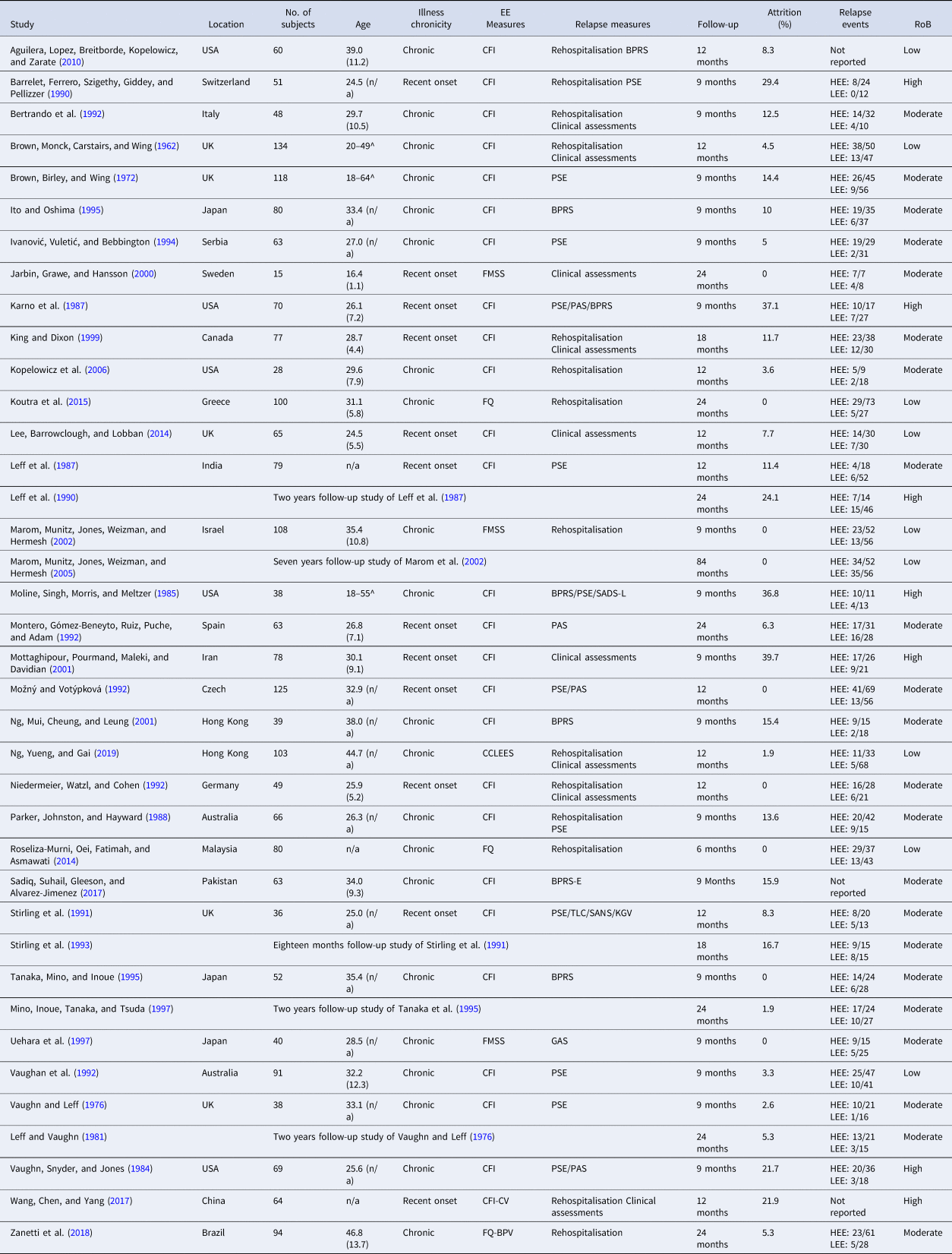
Age, Mean (s.d.); ^, Age range of the service users; HEE, High expressed emotion; LEE, Low expressed emotion; CFI, Camberwell Family Interview; BPRS, Brief Psychiatric Rating Scale; PSE, Present State Exam; Clinical assessments, deteriorated psychiatric symptoms/increased medication dosage after consultation or checking against case note; FMSS, Five Minutes Speech Sample; PAS, Psychiatric Assessment Scale; FQ, Family Questionnaire; SADS-L, Schedule for Affective Disorders and Schizophrenia; Lifetime Version, CCLEES, Concise Chinese Level of Expressed Emotion Scale; BPRS-E, Brief Psychiatric Rating Scale-Expand; TLC, Thought Language and Communication Scale; SANS, Scale for Assessment of Negative Symptoms; GAS, Global Assessment Scale; CFI-CV, Chinese version of Camberwell Family Interview; FQ-BPV, Brazilian Portuguese version of Family Questionnaire; RoB, Risk of Bias.
EE and overall relapse rate
The weighted mean of HEE family members of people with schizophrenia across studies was 50.9% (s.d. = 12.5) (k = 30, N = 1853, range = 23.3%–76.2%), in which CC (k = 14, N = 893, mean = 46.9%, s.d. = 18.3, range = 25.0%–94.1%), hostility (k = 5, N = 238, mean = 48.9%, s.d. = 32.1, range = 19.3%–80.0%), and EOI (k = 14, N = 893, mean = 36.3%, s.d. = 17.6, range = 12.0%–72.2%) were the three most reported EE among the four domains. By culture, Western countries had significantly more HEE families (k = 21, N = 1261, mean = 55.5%, s.d. = 11.4) than that of Eastern countries (k = 9, N = 592, mean = 41.1%, s.d. = 9.12, p < 0.00001), and it was similar for the CC subscale (p = 0.06). The overall relapse rate of all participants across different time points of follow-ups was large (k = 30, mean = 43.7%, s.d. = 12.7, range = 15.8–73.3%).
Meta-analysis findings: relapse prediction by global EE
Significant relation was found between HEE and relapse [k = 30, N = 1853, OR 3.74 (95% CI 2.75–5.09)] (Fig. 2). The subgroup analysis of timing of relapse found HEE had a significant effect on early relapse [k = 20, N = 1237, OR 4.90 (95% CI 3.46–6.94) and late relapse [k = 10, N = 616, OR 2.09 (95% CI 1.40–3.13)] (Fig. 2). The differences of the effects on early and late relapse were also significant (χ2 = 9.82, p = 0.002, I 2 = 89.8%). When six studies with high RoB were removed, the effect estimates on overall [OR 3.67 (95% CI 2.58–5.22)], early relapse [OR 4.87 (95% CI 3.22–7.36)], late relapse [OR 2.13 (95% CI 1.36–3.35)], and subgroup difference by timing of relapse were still significant (χ2 = 6.99, p = 0.008, I 2 = 85.7%). Similarly, when another six studies that was considered as extreme outliers (i.e. OR > 40) were removed, the effect estimates on overall [OR 3.21 (95% CI 2.37–4.34)], early relapse [OR 4.17 (95% CI 2.94–5.93)], late relapse [OR 2.02 (95% CI 1.36–2.98)], and subgroup difference remained significant (χ2 = 7.33, p = 0.007, I 2 = 86.4%). However, when focusing on the parental EE-relapse association, in which studies explicitly reported that at least 80% of the family members were parents, the pooled effect estimate dropped from 3.74 to 2.73 [k = 10, N = 506, OR 2.73 (95% CI 1.35–5.56), p = 0.005].

Fig. 2. Forest plot of association of global EE and relapse.
Meta-analysis findings: relapse prediction by EE domains
Higher CC [k = 10, N = 717, OR 2.22 (95% CI 1.16–4.26)] was significantly related to more relapse while higher level of warmth [k = 2, N = 116, OR 0.35 (95% CI 0.15–0.85)] was related to lower relapse rate (Fig. 3). Other domains of EE were not found to have significant relationship with relapse. After removing two studies with high RoB, only CC had a trend significance in relating with relapse [k = 8, N = 621, OR 1.82 (95% CI 0.94–3.52), p = 0.08].

Fig. 3. Forest plot of association of EE domain and relapse.
Factors affecting EE-relapse association
Categorical moderator analysis was computed to examine the seven putative moderators including age, proportion of schizophrenia sample, length of condition, culture, EE measures, RoB, and publication year (Table 2). None of them was significantly associated with EE-relapse linkage (p = 0.83), and the findings remained the same by changing some of the variables into continuous data such as length of condition and publication year. After removing six high RoB studies, the results of moderator analyses also remained similar (p = 0.82).
Table 2. Summary of multiple random-effects meta-regression in moderator analysis

CFI, Camberwell Family Interview, p value by Omnibus test = 0.828.
Study methodological rigor
Online Supplementary Table S1 described the results of bias assessment and the breakdown evaluation of the 11-item Joanna Briggs Institute Critical Appraisal Checklist for Cohort Studies. A total of 31 (81.6%) research reports were graded as low-moderate RoB and the included studies were found to be susceptible to selection bias, attrition bias, and reporting bias. In total, 29 (76.3%) studies did not explicitly report assessment of the covariates and its influence on the effect estimates by using appropriate statistical methods. Almost all studies used complete case analysis to treat the loss of follow-up, but only 21.1% of these studies (k = 8) met the analysis assumption. Moreover, two studies with an average 17.8% attrition rate did not explicitly describe the reasons of loss of follow-up. Only two studies reported the sample size calculation and one-third of the studies (k = 11) recruited samples of less than 60. Besides, the study methodological quality improved with time (ρ = 0.38, p = 0.03) and negatively correlated with attrition rate (ρ = –0.69, p = 0.0000081). However, no significant association was found between study methodological quality and the effect estimate (Table 2).
Leave-one-out analysis revealed that the pooled effect estimate remained stable after removing any one of the studies one at a time (online Supplementary Fig. S1). The pooled OR and the percentage changes from the baseline ranged from 3.60 (−3.74%) to 3.96 (5.88%). Cumulative analysis (online Supplementary Fig. S2) by publication year indicated that the pooled effect estimate became stable since 1992. Besides, although there were a few missing dots in the lower left quadrant in the funnel plot (online Supplementary Fig. S3), publication bias did not exist. It was confirmed by arcsine test (p = 0.25) and this concern might be caused by the small-study effect (Sterne et al., Reference Sterne, Sutton, Ioannidis, Terrin, Jones, Lau and Higgins2011). Trim-and-fill method suggested that the bias-adjusted overall OR was 3.28 (95% CI 2.39–4.49), similar to the effect estimates after removing the six small studies mentioned in the previous paragraph.
Discussion
This meta-analysis and meta-regression study critically appraised and examined the existing evidence to provide a comprehensive overview of EE-relapse association in schizophrenia. Global HEE was significantly related to relapse, more with early relapse (within 12 months) than the late relapse. Of the four domains of EE, CC predicted relapse and warmth had protective effects. Age, length of the condition, culture, EE measurements, and publication years did not significantly moderate the outcome. This review also found Western studies reported more HEE families than that from the Eastern regions.
Only cohort studies were included in the current study to minimise selection and attrition biases. We found a significant relationship between global EE and relapse, that is consistent with the previous meta-analyses result, further highlighting the significance of the EE of caregivers in relapse prevention. In exploring more comprehensively the EE-relapse relationship, the current studies provided several new findings. First, we found high EE associated with early relapse more significantly than the later relapse. This suggested a dynamic interaction between EE and relapse with time. As there are multiple factors contributing to the risk of relapse, change of factors including EE with time might impact on the relationship of EE and relapse over a longer period. Secondly, among the domains of the EE, only CC was found to be significantly related to relapse and warmth domains of EE can reduce the risk of relapse. Currently, family psychoeducation appeared to be an effective treatment modality to reduce EE domains such as EOI (Pharoah, Mari, Rathbone, & Wong, Reference Pharoah, Mari, Rathbone and Wong2010), CC (Ma, Chien, & Bressington, Reference Ma, Chien and Bressington2018; Pharoah et al., Reference Pharoah, Mari, Rathbone and Wong2010), and hostility (Pharoah et al., Reference Pharoah, Mari, Rathbone and Wong2010). However, the treatment effect on global EE was equivocal (Sin et al., Reference Sin, Gillard, Spain, Corneliu, Chen and Henderson2017). Results of the current study suggested that intervention focusing on reducing CC domains of EE might have a more significant benefit to change relapse outcomes. Two recent systematic reviews found cognitive behavioural family intervention and compassion-focused therapy may be beneficial to the schizophrenic patients and their families, in which both of the interventions target on the cognitive reappraisal and emotional resilience to foster a family climate and dynamic (Ma et al., Reference Ma, Chan, Chien, Bressington, Mui, Lee and Chen2020; Mui et al., Reference Mui, Chan, Chan, Hui, Chang, Lee and Chen2019). These evidences confirmed the foci of family intervention with the purpose of reducing EE, specifically CC domains and enhancing the sense of warmth. Though studies reported the nature of the relationship between caregiver and patients, few reported its effect on the EE-relapse relationship. The current study found parental HEE is a significant risk factor of relapse, it might be only an observational finding (Higgins et al., Reference Higgins, Thomas, Chandler, Cumpston, Li, Page and Welch2020). Further studies will be needed to explore in detail the role of nature of the relationship between caregivers and patients on the link of EE and relapse. Finally, we found that a greater number of HEE families were detected in Western countries than the Eastern countries. An earlier review suggested Western culture encourages more direct expression and individuals tend to have higher emotional arousal and that might explain the difference of EE level between culture (Hooley, Reference Hooley2007). However, similar to the previous two review studies, we found culture was not a significant factor in moderating the relationship between HEE and relapse.
Differ from the earlier meta-analysis (Butzlaff & Hooley, Reference Butzlaff and Hooley1998), length of condition was not found to be a significant moderator of the EE-relapse association. This is possible that more studies involving patients with earlier stages of the condition have been conducted since the first review. Our results suggest that EE is an important contributor to relapse among patients with different stages of the condition. The current study further explores other possible moderating factors including age, EE measures, RoB and publication years, and none were found to be significant moderators. This highlighted the robustness of the relationship between HEE and relapse. The lack of significant impact of EE measures suggested that other valid EE measurements may also be sensitive in the study of EE and relapse.
The results of the current study should be interpreted with regard to the following limitations. Firstly, the operational definitions of relapse across studies differed widely between studies with five studies used rehospitalisation solely as a relapse indicator without clinical measurements. This may have contributed to the variation of results. Secondly, in order to avoid double-counting, only studies with the longest follow-up were included for studies with multiple reporting. Thirdly, due to different covariate adjustments across studies, crude OR was extracted from individual reports rather than adjusted OR (if reported) to pool the effect estimates. Finally, because of small sample sizes in some of the subgroup analyses (k < 10), the corresponding findings should be interpreted in caution.
Conclusion
High EE is a robust predictor of schizophrenic relapse, with more impact on early relapse than that on late relapse. Among the four domains of EE, critical comments seem to be a significant factor related to relapse and level of warmth may have a protective role. Results confirmed the foci of family intervention on reducing EE, specifically reducing critical comments and improving the level of warmth.
Supplementary material
The supplementary material for this article can be found at https://doi.org/10.1017/S0033291721000209.
Acknowledgements
This research received no specific grant from any funding agency, commercial or not-for-profit sectors.
Conflict of interest
None.








