Nepal is home to the highest summit on earth of the world’s tallest mountain but is vulnerable to seismic events owing to the presence of several active faults.Reference Malla, Kayastha and Sharma 1 Nepal has experienced 5 major earthquakes in the past 100 years.Reference Simkhada, van Teijlingen, Pant, Sathian and Tuladhar 2 On April 25, 2015, Nepal experienced an earthquake of a magnitude of 7.6 on the Richter scale that resulted in 8790 casualties, 22,300 persons injured, and over half a million homes destroyed. According to a post-disaster needs assessment, the total damage and losses are estimated at US $7.5 billion. 3
Response activities after the 2015 earthquake started gradually but soon caught up to critical response tasks. A joint effort was made by government authorities and the international community in the week following the tragedy, and many lives were saved because of the relief effort. However, the public was concerned about how effectively the response was performed. This article summarizes the outcomes of 4 workshops held in 2015 and a national “Lessons Learnt” conference held in April 2016. The workshops and conference were an opportunity to review the experiences of the public and private hospitals of Kathmandu valley, the district (public) health offices of the affected districts, and the 10 public hospitals and 18 private hospitals of the 14 severely affected and 5 moderately affected districts (Figure 1). 3

Figure 1 Categories of Earthquake Affected Districts. Source: National Planning Commission 3 (map prepared by Dr Bhagawat Rimal).
IMMEDIATE RESPONSE
Within an hour of the earthquake, the Ministry of Health (MoH) activated the Health Emergency Operation Center (HEOC) and held its first emergency committee meeting. Hub-hospitals, district hospitals, district/public health offices (D[P]HOs), and rapid response teams (RRTs) at the central, regional, and district level 4 were activated.
The MoH set up a triage point at the airport accompanied by the Nepal Army Medical Team. The immediate priorities were to treat critical patients received by airlift and to perform basic screening and referrals. 5 A Health Information Management Unit was established at the HEOC to collect situation reports from the districts. All governmental, nongovernmental, community, and private hospitals were asked to provide free, 24-hour service.
The RRT concept was first initiated for outbreak preparedness and response activities in 2001. Since 2003, RRTs have been the main focal point for health sector preparedness and response to any kind of disaster. There are 4 levels of RRTs: central, regional, district, and community. The central- and regional-level RRTs are responsible for resource arrangement, technical support, and capacity enhancement of the district and community RRTs. Community RRTs are the first responders to any disaster. District-level RRTs pre-position medicines, medical supplies, and logistics at different strategic locations and communicate with local stakeholders and community, regional, and central RRTs.
D(P)HOs were responsible for overall health- and health services-related responses. In addition, the World Health Organization (WHO) and United Nations Children’s Fund (UNICEF) jointly supported nutrition, sanitation, vaccination, and communication efforts with other United Nations (UN) agencies and its field offices. The government also put in place additional governance and oversight mechanisms. The grassroots level of the community was reached through local health practitioners, female community health volunteers, private clinics, and other volunteers.
HUB-HOSPITALS AND LOGISTICS SUPPLY
The main objective of the hub-hospital system was to mobilize human resources and logistics to the right hospital at the right time for the right use. An illustrative prototype of the hub-hospital system is outlined in Figure 2. During the 2015 Nepal Earthquake, 6 pre-identified emergency hub-hospitals were activated within Kathmandu valley, which coordinated with designated satellite hospitals. Altogether, a network of 51 satellite hospitals functioned under the hub-hospitals. All hub-hospitals in Kathmandu valley and 7 of 11 district hospitals outside the valley remained functional. All private hospitals (>50 beds) and public hospitals were accountable to their corresponding hub-hospital.
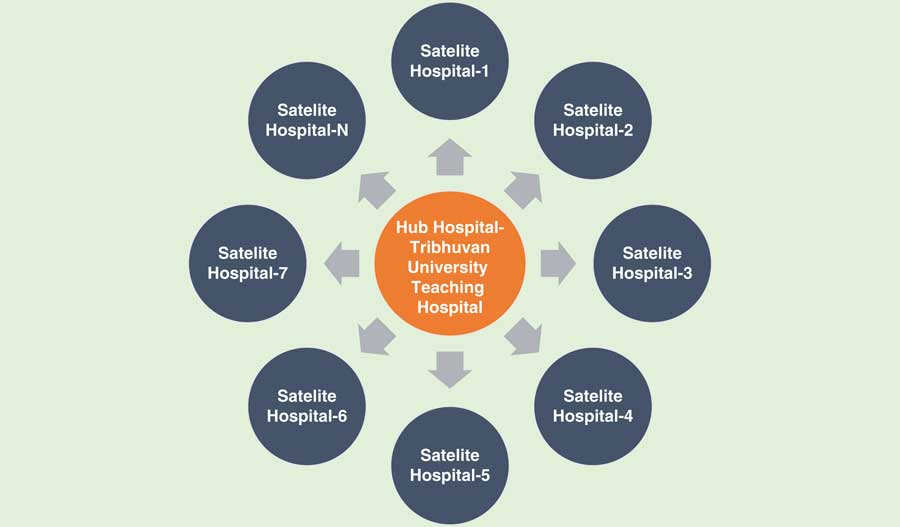
Figure 2 A Prototype Map of a Hub-Hospital.
The Logistic Management Division (LMD) played a crucial role in estimating, procuring, and supplying logistics. The Department of Drug Administration performed stocking, secured essential supplies and equipment, ensured drug availability, verified drug quality, regulated registration status, and authorized donations. The supply chain was managed through LMD to regional medical stores onto D(P)HOs and then dispatched to health facilities, hospitals, or clinics or nongovernment facilities. 4 , 5
COORDINATION AND COMMUNICATION
Government of Nepal activated a cluster coordination mechanism with UN where 11 clusters (health, nutrition, emergency communication, camp management, education, food security, logistics, protection, shelter, water/sanitation, and early recovery) coordinated overall response activities.
Under the leadership of the MoH, the health cluster was co-led by the WHO, together mainly with UNICEF, United Nations Population Fund, World Food Program, and other cluster member organizations (Nepal Red Cross, International Organization for Migration, etc). Sub-clusters were formed under the health clusters, for example, for reproductive health, mental health, injuries management, physical rehabilitation and tuberculosis treatment. The above-mentioned clusters/sub-clusters worked closely with D(P)HOs at local level. Nongovernmental organizations, academic institutions, private institutions, volunteers, and researchers also offered assistance to the health clusters. All relief activities at the district level were coordinated through the District Disaster Relief Committee led by the Chief District Office. The MoH and the Ministry of Home Affairs worked together to manage the bodies of the deceased.
The HEOC established regular communication with the National Emergency Operation Centre, the hub-hospitals, and the D(P)HOs. A 24-hour toll-free hotline was established for the emergency management. A separate desk was established with the National Health Education, Information and Communication Centre to disseminate messages about epidemic prevention with a special focus on children, pregnant women, mothers and newborns, and elderly, disabled and internally displaced persons. Information was circulated by use of different media, and rumors were addressed and managed. A post-earthquake communication plan was developed and implemented through frontline health workers and civil society organizations.
MOBILIZATION OF MEDICAL TEAMS
When the Government of Nepal appealed for international assistance, the MoH received an influx of foreign medical teams (FMTs). All FMTs were either registered by the WHO before arrival in the country or registered as an FMT directly with the HEOC, where their eligibility was assessed and they were oriented and deployed to places of need. The FMT coordination team established by the HEOC comprised a MoH focal point, a WHO coordinator, and other representatives from the Nepal Army, and other organizations.
FMTs were asked to use national protocols while managing cases (e.g. emergency trauma protocols on spinal cord injuries, open fracture) to ensure uniformity in treatment and referral. They were instructed to maintain detailed documentation for trauma and amputation clients who required follow-up and rehabilitation, and daily reporting on templates issued by the MoH.
More than 137 FMTs 5 and over 100 national medical teams were deployed through the HEOC. The FMTs offered services including general surgery, orthopedics, gynecology, obstetrics, and psychiatric services through mobile clinics, field hospitals, primary health care centers, and health posts. FMTs became very supportive in lifesaving efforts. The HEOC also facilitated an exit process for the teams as soon as they completed their assignments.
TREATMENT AND EPIDEMIC SURVEILLANCE
Entire hospitals were engaged in providing trauma and emergency services. A total of 20 field hospitals were established for rapid rescue and emergency services. 5 This helped to ensure the provision of safe blood supplies at the hospitals and other treatment facilities. 6 Temporary health services were managed through hospital tents and mobile health services. The MoH confirmed free follow-up services for preexisting chronic disease.
Post-earthquake hospital-based syndromic surveillance was activated within 1 week. This surveillance system covered 96 treatment sites including 66 hospitals and temporary camps within the Kathmandu valley and 30 hospitals and temporary camps outside the valley. Through December 2015, epidemiological surveillance continued and 59,000 cases were classified into 8 syndromes such as severe acute respiratory infection, acute watery diarrhea, and bloody diarrhea and so on. No major outbreaks were reported. The RRTs remained functional for early identification and containment of possible outbreaks.
RESUMPTION OF PRIMARY HEALTH CARE SERVICES
Over 80% of health facilities in the affected districts were either damaged or destroyed in the earthquake. 3 , 6 Primary health care services like immunization, maternal and neonatal services, nutrition, family planning, and reproductive health were major concerns in the temporary and internally displaced campsites. Tents for health facilities, medical supplies, reproductive health kits and hygiene kits, bed nets, 7 drugs, and additional human resources and rehabilitation support were provided. Mass vaccination campaigns were launched against measles/rubella/polio, and cholera. Thus, routine health care was maintained. However, some criticism on implementation of preventive measures such as health education, health promotion, and community engagement was noted.Reference Adhikari, Mishra and Raut 8
CHALLENGES
Coordination was a challenge from the beginning to streamline national and sub-national level’s responses. There was an environment of uncertainty due to network failures, power cuts, damaged roads and bridges, and landslides.Reference Simkhada, van Teijlingen, Pant, Sathian and Tuladhar 2 , 5 Limited airport capacity and logistics management created bottlenecks. Bad weather and powerful aftershocks further inhibited access. In addition, some medicines supplied were not registered or were near expiration. Problems with the distribution of emergency drugs were also noted. 5 Hospitals were overcrowded with post-surgery patients. Shifting surgical equipment, transferring supply lines, supplying water in the tents, and the insufficiency of major equipment were also a challenge for managing casualties. 4 , 5
LESSONS LEARNED
In general, the health sector response to the 2015 earthquake was successful through the UN cluster coordination mechanism, which worked closely with the established national disaster response mechanisms.Reference Austin, Grosso and Oneil 9 In a review of the effectiveness of the earthquake relief efforts, one study noted that “the aid distribution and support was also relatively fair.”Reference Paul, Acharya and Ghimire 10 However, some weaknesses at the planning and management levels, such as in governance, affordability and gaps in communication and coordination have been revealed. 4 , 5 , Reference Austin, Grosso and Oneil 9 , Reference Paul, Acharya and Ghimire 10 These issues should be considered in the future. The main lessons learned were as follows:
∙ Better coordination, 4 , Reference Cook, Shrestha and Htet 11 - 13 alternate means of communication, faster deputation of medical teams, 4 and improved hospital resilience infrastructure 13 are needed.
∙ All emergency response guidelines must be updated and followed to meet the minimum standards of humanitarian relief. 4 , 5
∙ Preparedness plans need to indicate responsibilities across all sectors to avoid overlap.
∙ The language barrier affects communication with and assistance from FMTs.Reference Cook, Shrestha and Htet 11 , Reference Merin, Yitzhak and Bader 14 FMTs who worked with national medical teams found it easier to apply lifesaving procedures (due to familiarity with local medical practices).
∙ Impaired infrastructure in the affected area may not only hinder the provision of basic and emergency health care services but also halt continued gains in maternal and child health and other important health indicators.Reference Regmi, Aryal, Pant, Van Teijlingen, Simkhada and Devkota 15
LIMITATIONS
Critical and negative voices may not have been expressed by participants, which could have resulted in an unequal representation of responses.
CONCLUSIONS
Overall, the health sector’s response was concluded to be largely satisfactory because it focused not only on emergency clinical care, but also on the resumption of basic health services and other preventive health care (eg, sanitation, risk communication) equally. Post-disaster disease outbreak did not occur because effective surveillance and outbreak monitoring was one of the priority actions. However, services related to birthing centers, neonatal services, and vaccinations were impeded in some rural areas. Some weaknesses in planning, coordination, and management were also noted. The lessons learned can provide the impetus to strengthen future preparedness and response mechanisms.
Disclosures
We declare no conflicts of interests.
Acknowledgments
The authors thank Dr Guna Raj Lohani, Coordinator for HEOC; Mahendra Prasad Shrestha, Senior Public Health Administrator (MoH); Dr Shyam Thapa, formerly Research Scientist (WHO/Switzerland); Dr Jos Vandelaer (Country Representative/WHO); and Dr Hendrikus Raaijamakers (Chief-Health Section-UNICEF) for helpful comments on earlier drafts of this paper. We express our appreciation to all the participants who shared their time, experiences, and insights with us. We thank the WHO for assisting the MoH in co-leading the health cluster for the entire health cluster response and for technical and financial assistance to organize the district, national, and regional-level reviews, and the workshops. Thanks also to Christopher Fraser Dyson and Jennifer Holmes for their review and editorial assistance.




