Chest pain is a common presenting complaint to paediatrics, paediatric cardiology, and paediatric emergency departments. The majority of chest pains in otherwise healthy children have a non-cardiac cause.Reference Balfour and Rao 1 – Reference Zavaras-Angelidou, Weinhouse and Nelson 4 Although a cardiac cause for chest pain is uncommon in children, concern for this possibility prompts referral to a paediatric cardiologist. It has been reported that chest pain complaint accounts for 5.2% of all paediatric cardiology consultations.Reference Geggel 5 Few studies have investigated patients with chest pain referred to a paediatric cardiology clinic.Reference Evangelista, Parsons and Renneburg 2 , Reference Tunaoglu, Olgunturk, Akcabay, Oguz, Gucuyener and Demirsoy 3 , Reference Fyfe and Moodie 6 – Reference Friedman, Kane and Rathod 8 In this study, we prospectively evaluated the clinical characteristics and causes of chest pain in children referred to our paediatric cardiology unit.
Methods and materials
Study population
This study enrolled children under the age of 18 years who were referred to our pediatric cardiology unit with the chief complaint of chest pain over a period of 10 months (April, 2010–January, 2011). The study was approved by the local ethics committee and written informed consent was obtained from the parents of the patients.
Demographic and clinical data were collected for all patients. Data on past medical history, family history, and symptoms, including chest pain characteristics and associated symptoms, were prospectively collected during the paediatric cardiology unit visit. The presence of associated symptoms, including dizziness, syncope, palpitations, and exertional dyspnoea, was investigated.
Family history was considered positive if any of the following was present in a first-degree relative: sudden or unexplained death, cardiomyopathy, severe familial hyperlipidaemia, and premature cardiovascular disease. Family history of premature cardiovascular disease was considered positive if any of the following was present in a first-degree relative: myocardial infarction, angina pectoris, peripheral or cerebral vascular disease, and sudden death before the age of 55 years. 9 , Reference Daniels and Greer 10
All children underwent complete physical examination, including weight and height measurements. The body mass index was calculated as weight (in kilograms) divided by height (in metres) squared. Children were defined as obese if they had a body mass index greater than or equal to 95th percentile, and overweight if they had a body mass index between 85th and 94th percentile for age and gender based on the standards of the Centers for Disease Control and Prevention.Reference Daniels and Greer 10 Blood pressure was measured with a standard mercury sphygmomanometer after a 10-minute rest. Abnormalities detected on physical examination, which were considered pertinent positives, included tenderness on palpation over the chondrosternal or costochondral junction, swelling at the chondrosternal junction, murmur, click, gallop, pericardial rub, abnormal second heart sound, distant heart sounds, hepatomegaly, decreased femoral or peripheral pulses, peripheral oedema, painful or swollen extremities, and tachypnoea.
The following studies were performed by a paediatric cardiologist: complete blood count in all patients; fasting total cholesterol, high-density lipoprotein cholesterol, low-density lipoprotein cholesterol, and triglycerides levels in overweight and obese children and children with a family history of premature cardiovascular disease; electrocardiogram, chest X-ray, two-dimensional and colour Doppler, and pulsed and continuous Doppler echocardiogram (ProSound Alpha 7, Hitachi-Aloka Medical, Tokyo, Japan), and if necessary 24-hour electrocardiogram monitoring and/or exercise stress tests were performed.
Test interpretation
Electrocardiogram interpretation was based on documented findings in the paediatric cardiologist's clinic note. Ventricular hypertrophy, atrial enlargement, pathologic ST-segment or T-wave changes, atrioventricular block, ventricular or atrial ectopy, axis deviation, and other miscellaneous findings – for example ventricular preexcitation – were classified as abnormalities. Incomplete right-bundle branch block and early repolarisation were considered to be normal variants.
Echocardiogram and exercise stress test results were obtained from reports generated at the time of the study. Diagnoses that were considered potential cardiac causes of chest pain included coronary artery anomalies, cardiomyopathies, myocarditis, pericarditis, pulmonary hypertension, aortic dissection, arrhythmia, and moderate or greater left ventricular outflow tract obstruction. Findings considered to be positive on the exercise stress test included ST-segment or T-wave changes concerning ischaemia or tachyarrhythmias. Similarly, tachyarrhythmias or bradyarrhythmias on 24-hour electrocardiogram monitoring were considered to be positive findings.
Cut-off points to define elevated total cholesterol, low-density lipoprotein cholesterol, non-high-density lipoprotein cholesterol, and triglycerides and low high-density lipoprotein cholesterol in children and adolescents were reported previously.Reference Daniels and Greer 10 Patients were considered to have dyslipidaemia if one or more of these lipid or lipoproteins were abnormal.
Children with a history of positive psychological findings were evaluated by a child psychiatrist using the Diagnostic and Statistical Manual of Mental disorder-IV-Text Revision (DSM-IV-R) diagnostic criteria. 11
Causes of chest pain were categorised mainly as cardiac-related causes and non-cardiac-related causes – musculoskeletal, respiratory, psychological, gastrointestinal, and miscellaneous disorders and idiopathic chest pain – as previously reported by Selbst.Reference Selbst 12
Statistical analysis
Clinical symptoms were expressed as counts and percentages. Statistical analyses were performed using a computer software package (SPSS for Windows, version 15.0).
Results
During the study period, 440 patients presented or were referred to our unit with the chief complaint of chest pain. A total of 60 patients were excluded from the study because of refusal to participate in the study. The remaining 380 patients comprised 190 (50%) girls and 190 (50%) boys. The mean age of the girls was 10.9 plus or minus 2.7 years with a median of 11 years and a range of 4–17 years and the mean age of the boys was 10.8 plus or minus q2.8 years with a median of 11 years and a range of 4–16 years.
In all, 21 patients had previously diagnosed disease, including familial Mediterranean fever in four patients, asthma in seven patients, and previously known echocardiographic abnormalities in 10 patients. There were 15 patients with a positive family history of premature cardiovascular disease.
In all, 56 (14.7%) patients had used paracetamol and 13 (3.4%) patients had used aspirin; 185 (48.7%) patients were passive cigarette smokers; 16 patients had a severe cough history for 1 month; 54 patients had characteristic features of precordial catch syndrome pain with sudden onset, most frequently at rest, well-localised, sharp, stabling, needle-like pain, exacerbated by deep breathing, with each episode lasting for 30 seconds to 3 minutes.Reference Gumbiner 13
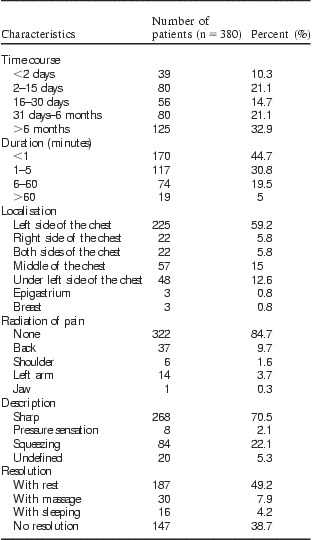
Table 1 shows characteristics of the chest pain in children. A total of 125 (32.9%) patients had pain for at least 6 months. The duration of the pain was variable. The most common location of the chest pain was the left side of the chest (225 patients, 59.2%). The most common radiation of chest pain was none (322 patients, 84.7%). A total of 268 (70.5%) patients described their pain as sharp; 79 patients (20.8%) reported chest pain only with exercise; and 195 patients (51.3%) had pain both with exercise and at rest. Less-reported triggering factors were anxiety (65 patients) and eating (12 patients). In 29 patients, no precipitating events were identified. In 187 (49.2%) patients, chest pain did not resolve at rest.
Table 1 Characteristics of chest pain in children.

Palpitations were the most common associated symptom, with chest pain reported in 116 (30.5%) patients. Dizziness and exertional dyspnoea were the other commonly associated symptoms, with reports by 85 (22.3%) patients and 73 (19.2%) patients, respectively. Syncope was reported in 16 (4.2%) patients. No associated symptoms were reported in 90 (23.6%) children.
On physical examination, the mean weight was found to be 37.1 plus or minus 14.1 kilograms with a range of 13–88 kilograms and the mean height was found to be 140.3 plus or minus 16.0 centimetres with a range of 91–180 centimetres. The mean body mass index was 18.19 plus or minus 3.63 kilograms per square metre with a range of 10.12–33.53 kilograms per square metre. In all, 27 patients (7.1%) had obesity, 17 patients (4.4%) were overweight, and nine patients (2.3%) had failure to thrive. The mean systolic and diastolic blood pressures were 100.2 plus or minus 10.3 millimetres of mercury with a range of 80–120 millimetres of mercury and 63.2 plus or minus 8.0 millimetres of mercury with a range of 50–80 millimetres of mercury, respectively. None of the patients had elevated blood pressure (above the 95th percentile for age and sex). Owing to breast pain, three patients (two gynaecomastia, one telarche) had chest pain. In all, five patients had ecchymosis on the thorax; eight patients had chest wall deformities, that is, four with pectus excavatum, four with pectus carinatum; 14 patients had pectoral muscle myalgia; and 127 patients had chest pain on palpation of their costochondral joints and were diagnosed as having costochondritis. These patients were treated with paracetamol or ibuprofen. A total of 112 patients had murmurs or clicks on physical examination. Of them, 10 (8.9%) had a pathological murmur, and findings on echocardiogram were consistent with the physical examination findings. Of the 10 patients, four had mitral valve prolapsus, two patients had pulmonary valve stenosis, three patients had ventricular septal defects, and one patient had bicuspid aortic valve. The remaining patients were diagnosed as having innocent murmurs. Chest auscultation revealed crepitan rales in two patients and sibilant rales in seven patients. Chest X-rays revealed pneumonic consolidation and hyperaeration in these patients, respectively. These patients were referred to paediatric pulmonology and paediatric allergy departments.
The electrocardiogram was normal in 376 (98.9%) patients. However, four patients (1.1%) had an abnormal electrocardiogram; these abnormalities were infrequent premature ventricular contractions in three patients and pathologic ST-segment and T-wave abnormalities in one patient. In these three patients, 24-hour electrocardiogram recordings revealed infrequent premature ventricular contractions. These three patients reported palpitations with chest pain. Exercise stress tests were performed in 12 patients who had exertional chest pain, all of which were normal.
Complete blood count revealed anaemia in 12 patients and leukocytosis in 20 patients according to their ages. Patients who had anaemia and/or leukocytosis were referred to the department of paediatrics. In the fasting state, there was dyslipidaemia in 3 of 27 obese children, in 3 of 17 overweight children, and in 3 of 15 patients who had a family history of premature cardiovascular disease. A total of 9 of 380 patients (2.3%) had dyslipidaemia. Overweight and obese patients without/with dyslipidaemia were referred to our paediatric endocrinology unit. Patients who had a family history of premature cardiovascular disease will be followed-up in our paediatric cardiology unit.
A total of 150 of 380 patients (39.4%) who presented with chest pain and whose serum troponin I levels were studied during the paediatric emergency department visit before paediatric cardiology visit were found to be normal.
There were four patients who were diagnosed as having gastroesophageal reflux disease by gastroesophageal scintigraphy and referred to the paediatric gastroenterology unit.
Of the 65 patients referred to a child psychiatrist for psychiatric evaluation, 41 (10.7%) patients were found to have a psychological disorder. The most common diagnoses were adjustment disorder (29.3%), generalised anxiety disorder (22%), and depressive disorder (17.1%). Table 2 shows the results of the psychiatric evaluation.
Table 2 Psychological disorders diagnosed in children with chest pain.

Echocardiogram were performed in all patients in order to diagnose a possible abnormality of a coronary artery origin, coexisting acquired or congenital heart diseases. A total of 10 patients had a previously known echocardiographic diagnosis, including one with a muscular ventricular septal defect, two with perimembranous ventricular septal defect, four with secundum-type atrial septal defect, two with mild valvular pulmonary stenosis, and one with rheumatic heart disease – mitral valve regurgitation. Echocardiogram revealed pericarditis in one patient as a cause of cardiac-related chest pain. In all, 25 (6.5%) patients had incidental cardiac diagnoses discovered during the chest pain evaluation, which were unrelated to the presenting complaint of chest pain. Incidental echocardiographic diagnoses included nine mitral valve prolapsus, three parachute mitral valve, two mild aortic regurgitation, four bicuspid aortic valve without aortic valve stenosis, one aneurysmatic interatrial septum, three patent foramen ovale, one idiopathic pulmonary artery dilatation, and two increased left ventricular trabeculation. A follow-up cardiology evaluation was recommended in these patients.
Only 1 of 380 (0.3%) patients had chest pain because of cardiac-related causes according to the previous classification reported by Selbst,Reference Selbst 12 in which the patient had pericarditis. This patient had pericardial friction rub on physical examination, ST-segment and T-wave changes on electrocardiogram consistent with pericardial disease, and echocardiogram showing small pericardial effusion.
There were a total of 409 paediatric cardiology visits. There were 20 patients (5.2%) who had two or more clinic visits, accounting for a total of 29 repeat visits, with the remaining 360 patients having a single clinic visit. There was one patient who was admitted for inpatient evaluation of chest pain. This patient was hospitalised secondary to pericarditis.
In all, 111 patients (29.2%) were not found to have any causes to explain their chest pain. These patients were considered to have idiopathic chest pain.
Table 3 shows the causes of chest pain in patients. Non-cardiac-related causes accounted for 99.7% and cardiac-related causes accounted for 0.3%. Musculoskeletal disorders (37.1%) were the most common diagnosis. Musculoskeletal, psychological disorders, and idiopathic chest pain were more common in girls, whereas miscellaneous and respiratory disorders were more common in boys.
Table 3 Causes of chest pain in children.

Discussion
Our study is one of the largest studies that has evaluated chest pain in children referred to paediatric cardiology clinics. In this prospective study, we report demographic and clinical characteristics, as well as causes of chest pain in children referred to our paediatric cardiology unit. In recent years, news and media reports on sudden deaths in athletes have created concern among both families and physicians. Primary care and emergency department physicians may be fearful of missing cardiac pathology and assuming responsibility for clearing athletes to participate in sports. Although serious, fatal heart disease is extremely rare among children, families seek reassurance.Reference Cava and Sayger 14 About one-third of children with chest pain are awakened from sleep by the pain and one-third miss school because of the pain.Reference Selbst, Ruddy, Clark, Henretig and Santulli 15 In one study, 16% of children with chest pain had more than one visit to the emergency department with the same complaint.Reference Selbst 16 Chest pain often becomes a chronic problem, lasting more than 6 months in 7–45% of children.Reference Selbst, Ruddy, Clark, Henretig and Santulli 15 , Reference Rowe, Dulberg, Peterson, Vlad and Li 17 About 8% of children have chest pain for more than 1 year.Reference Selbst 16 In our study, chest pain had lasted for more than 6 months in 32.9% of the children and approximately 5% of children with chest pain had more than one visit to our unit with the same complaint.
In this study, we suggest that careful history and physical examination are enough to diagnose the causes of chest pain. In our study, electrocardiogram and echocardiogram were performed on all patients as part of their evaluation. The high percentage of patients with this comprehensive testing should increase the likelihood of documenting the presence of cardiac pathology, if it is present. In addition, we did not exclude patients who had known cardiac abnormalities if they were referred for evaluation of chest pain. This also would be expected to increase the likelihood of finding patients with a cardiac cause for their chest pain.
The serious cardiac causes of paediatric chest pain, including anomalous coronary origins, cardiomyopathy, pulmonary hypertension, myocarditis, and pericarditis, can be diagnosed by history, cardiac examination, electrocardiogram, and echocardiogram.Reference Friedman, Kane and Rathod 8 Our results emphasise the findings of previous reports showing that cardiac aetiologies of paediatric chest pain are rare. The incidence of a cardiac cause of chest pain was 1 in 380 (0.3%) in our study and it was lower than the previously reported results.Reference Evangelista, Parsons and Renneburg 2 – Reference Zavaras-Angelidou, Weinhouse and Nelson 4 , Reference Cava and Sayger 14 Mitral valve prolapse may cause chest pain by papillary muscle or left ventricular endocardial ischaemia. Mitral valve prolapse is not a frequent cause of paediatric chest pain and it is no more common in children with chest pain than in the general population.Reference Selbst 18 We did not include mitral valve prolapsus as a cause of cardiac chest pain, but it was an incidental echocardiographic finding.
Musculoskeletal disorders are perhaps the most common causes of chest pain in children.Reference Selbst, Ruddy, Clark, Henretig and Santulli 15 , Reference Massin, Bourguignont, Coremans, Comté, Lepage and Gérard 19 Careful physical examination reveals chest wall tenderness or pain with movement of the torso or upper extremities. Costochondritis is a common musculoskeletal disorder in children. The diagnosis is made by eliciting tenderness over the costochondral junctions with palpation.Reference Cava and Sayger 14 In our study, as previously reported in literature, musculoskeletal disorders (37.1%) including costochondritis, chest wall strain, and direct trauma/contusion from non-cardiac-related causes were the most common diagnosis.
Psychogenic disturbances cause chest pain in both boys and girls at equal rates.Reference Selbst, Ruddy, Clark, Henretig and Santulli 15 , Reference Massin, Bourguignont, Coremans, Comté, Lepage and Gérard 19 In our study, psychogenic disturbances were mild more common in girls (56%). In a study reported by Tunaoglu et al,Reference Tunaoglu, Olgunturk, Akcabay, Oguz, Gucuyener and Demirsoy 3 74% of children and adolescents with chest pain were found to have psychological symptoms, with “anxiety” being the most common problem. In another study, unexplained chest pain in the paediatric emergency department was found to be frequently associated with potentially treatable anxiety disorders.Reference Lipsitz, Gur and Sonnet 20 However, in our study, the most common psychological disorder was adjustment disorder rather than anxiety disorder.
Miscellaneous causes of chest pain include pain related to underlying diseases. Precordial catch is one of them, a syndrome of left-sided chest pain that is brief (less than 5 minutes duration) and sporadic. The aetiology remains unclear.Reference Gumbiner 13 In our study, 54 patients had characteristic features of precordial catch syndrome.
Idiopathic chest pain is diagnosed when no clear aetiology can be found. In 20–45% of cases with paediatric chest pain, no clear aetiology can be found.Reference Selbst, Ruddy, Clark, Henretig and Santulli 15 , Reference Driscoll, Glicklich and Gallen 21 In our study, idiopathic chest pain was present in 29.2% of the patients.
To our knowledge, no studies have been published that report on the risk factors in relation to chest pain frequency and severity among children experiencing chest pain. It would seem that a study assessing the type and magnitude of risk factors is warranted. Some of these risk factors occur in both adult and paediatric groups, for example certain beverages like coffee and carbonated drinks. Other risk factors such as aspirin use, non-steroidal anti-inflammatory drug use, smoking, and alcohol use are more of an issue in an adult group; however, this does not exclude the possibility of them being of importance in some paediatric presentations for chest pain. In our study, 13 patients (3.4%) had a history of aspirin use and 185 (48.7%) patients were passive cigarette smokers.Reference Eslick 22
Obesity may be important on its own or in combination with other conditions, such as gastroesophageal reflux disease.Reference Eslick 22 Another potential reason that more children with chest pain are being referred to paediatric cardiology is the increased number of overweight and obese children. It is possible that with increasing concern for premature coronary disease in overweight children. Our study population included 4.4% overweight and 7.1% obese children. In recent years, the screening of a lipoprotein profile is proposed if either obesity or overweight is detected per se, regardless of the presence of other non-lipid cardiovascular disease risk factors. This recommendation is congruent with the recent guidelines from the American Academy of Pediatrics.Reference Daniels and Greer 10 , Reference Kwiterovich 23 We detected dyslipidaemia in 3 of 27 obese children and in 3 of 17 overweight children with chest pain.
The National Cholesterol Education Program (NCEP) Expert Panel on Blood Cholesterol Levels in Children and Adolescents 9 recommended the following screening: (1) a lipoprotein profile in youth whose parents and/or grandparents required coronary artery bypass surgery or balloon angioplasty before the age of 55 years; (2) a lipoprotein profile in those with a family history of myocardial infarction, angina pectoris, peripheral or cerebral vascular disease, or sudden death before the age of 55 years.Reference Kwiterovich 23 In our study, we detected dyslipidaemia in 3 of 15 patients with chest pain who had family history of premature cardiovascular disease.
Limited information is available, however, regarding the use of serum troponin screening for risk stratification in children with chest pain. In a recent study, Brown et alReference Brown, Hirsh and Mahle 24 evaluated patients under 22 years of age, who presented with chest pain, who were not previously known to have cardiac disease, and whose troponin levels were evaluated by the emergency department during a 7-year period. Of the 212 patients who presented with chest pain, troponin levels were increased in 37 (17%) patients. Of these 37 patients, 18 (48%) cases were attributed to a primary cardiac diagnosis, with the most common discharge diagnosis being myocarditis or pericarditis. In our study, serum troponin I levels were studied in 150 of 380 patients (39.4%) who presented with chest pain and were found to be within normal limits in all patients.
Conclusions
Chest pain is a common referral complaint in children. In this study, the most common aetiologies of chest pain in children were musculoskeletal disorders, idiopathic chest pain, and miscellaneous disorders, respectively. Although a paediatric cardiology referral may provide reassurance to the primary care and emergency department physicians, our results show that cardiac causes of chest pain are very rare in children. Our results suggest that many patients in this study could have been adequately evaluated using careful history and physical examination. We think that echocardiographic examination may not be necessary in the routine evaluation of children with chest pain.