Introduction
Ménière's disease is an inner-ear disease in which the main histopathological finding is endolymphatic hydrops.Reference Hallpike and Cairns1,Reference Gürkov, Flatz, Louza, Strupp and Krause2 It is characterised by episodic vertigo, fluctuating hearing loss, tinnitus and aural fullness.3,Reference Minor, Schessel and Carey4 Although vestibular dysfunction is not incorporated into the diagnostic criteria for Ménière's disease, it is well known that some Ménière's disease patients have such dysfunction.Reference Minor, Schessel and Carey4,Reference Fujimoto, Egami, Kinoshita, Sugasawa, Yamasoba and Iwasaki5
Vestibular dysfunction in Ménière's disease patients induces dizziness and imbalance. The management of Ménière's disease is one of the most controversial topics in the field of otolaryngology. Methods for managing Ménière's disease include changes in lifestyle, oral medications, vestibular rehabilitation, intratympanic steroids or gentamicin therapy, and surgery. Betahistine and vestibular rehabilitation are first-line management methods for Ménière's disease.Reference Nevoux, Barbara, Dornhoffer, Gibson, Kitahara and Darrouzet6,Reference Magnan, Özgirgin, Trabalzini, Lacour, Escamez and Magnusson7
Postural instability and imbalance can be evaluated through static and dynamic posturography. The Tetrax Posturography System for balance assessment is a static posturography test consisting of four integrated but independent plates that measure postural sway in eight sensory conditions.Reference Gorski, da Silva, Cusin, Cesaroni, Ganança and Caovilla8 It compares the values of the anterior and posterior parts of each foot (toes and heels), and those of each heel with the anterior part of the contralateral foot, based on the pressure difference exerted on each plate, and calculates the risk that the individual has of falling.Reference Gorski, da Silva, Cusin, Cesaroni, Ganança and Caovilla8 The Tetrax fall index, a Tetrax balance assessment parameter, provides the doctor with an accurate fall risk for an individual in terms of balance ability.Reference Gorski, da Silva, Cusin, Cesaroni, Ganança and Caovilla8
The Dizziness Handicap Inventory, which is the most widely used quality of life measure for patients with vestibular disorders, can be used to identify the impact of vestibular impairment on functional, emotional and physical aspects.Reference Jacobson and Newman9
This study assessed changes in the quality of life and risk of falling in patients with Ménière's disease before and after treatment with betahistine and vestibular rehabilitation (Tetrax biofeedback).
Materials and methods
Sixty-six patients with a clinical diagnosis of definite Ménière's disease according to the American Academy of Otolaryngology – Head and Neck Surgery criteria,3 accompanied by dizziness and imbalance, were enrolled in the study. All patients had undergone a standardised physical and auditory-vestibular examination, and those with cognitive dysfunction, neuromuscular system disorders, central nervous system or spinal cord defects, middle-ear diseases, or other acute medical conditions were excluded.
All 66 patients were randomly allocated to 1 of the following 3 groups (n = 22 patients per group): (1) betahistine group, in which patients were treated with betahistine (3 × 12 mg daily) for a month; (2) Tetrax group, in which patients received vestibular rehabilitation (Tetrax biofeedback) for 30 minutes per day for a month; and (3) the control group, in which patients received no treatment.
During the one-month study period, two patients were unable to participate in vestibular rehabilitation (Tetrax biofeedback) on time, and three patients experienced a vertigo attack; these patients were excluded from the study. Thus, 61 patients with Ménière's disease completed the programme: 21 in the betahistine group, 20 in the Tetrax group and 20 in the control group. The three groups had similar sex and age distributions, Ménière's disease stages (stages 1–4), and functional level scales (levels 1–6; all p > 0.05) (Table 1). The stages and functional level scales of Ménière's disease were based on American Academy of Otolaryngology – Head and Neck Surgery criteria.3
Table 1. Baseline characteristics of patients in each group

*n = 21; †n = 20; ‡n = 20. SD = standard deviation; M = male; F = female
Vestibular rehabilitation (Tetrax biofeedback) was performed using the Tetrax Posturography System (BeamMed, Petach Tikva, Israel) under the supervision of a trained physical therapist. The Dizziness Handicap Index and Tetrax fall index scores, obtained one day before and one day after treatment, were used as the evaluation measures of therapy intervention before and after treatment. The Dizziness Handicap Index, which comprises 25 items, assesses the impact of dizziness on emotional (9 items), functional (9 items) and physical (7 items) subdomains. There are three answers to each question, namely ‘yes’, ‘sometimes’ and ‘no’, with corresponding scores of ‘4’, ‘2’ and ‘0’. Hence, a score of 0 indicates that dizziness has no effect on the patient. The maximum score is 100. The higher the score, the more serious the effect of dizziness. The Tetrax fall index, obtained using the Tetrax Posturography System, represents the quantitative risk of falling, with a higher fall index indicating a greater likelihood of falling.Reference Song, Chun, Kim, Lee, Yi and Park10
All data were analysed with SPSS® (version 22) statistical software and expressed as mean ± standard deviation values. The age of patients with Ménière's disease among the groups was analysed using a one-way analysis of variance. Gender was analysed using the chi-square test, and Ménière's disease stage and functional level were analysed using the Kruskal–Wallis H test. Linear correlation analysis (Pearson method) was performed between the Dizziness Handicap Index and fall index scores. We used the paired t-test to analyse the differences in the Dizziness Handicap Index and fall index scores after treatment versus before treatment. Analysis of covariance was used to compare the improvements of Dizziness Handicap Index and fall index scores among the three groups, and the Bonferroni method was performed for comparison between groups after analysis of covariance. Differences with a p-value of less than 0.05 were considered statistically significant.
Results
The correlation analysis showed that whether before or after treatment, there was a significantly positive correlation between Dizziness Handicap Index and fall index scores in Ménière's disease patients with dizziness and imbalance (pre-treatment: r = 0.824; post-treatment: r = 0.834; both p < 0.001) (Table 2).
Table 2. Correlation between Dizziness Handicap Index and fall index scores

Linear correlation analysis (Pearson method) was performed (n = 61)
Patients in the betahistine group and Tetrax group showed significant improvements in Dizziness Handicap Index and fall index scores after treatment versus before treatment (all p < 0.001), but there were no improvements for the control group (Dizziness Handicap Index, p = 0.176; fall index, p = 0.180) (Table 3). Additionally, there were statistically significant differences in post-treatment improvements for Dizziness Handicap Index and fall index scores between the three groups (Dizziness Handicap Index, F = 3.052, p = 0.035; fall index, F = 4.083, p = 0.022). The improvements in the Tetrax group were significantly better than those in the betahistine group (Dizziness Handicap Index, p = 0.007; fall index, p = 0.041), and the improvements in the betahistine group were significantly better than those in the control group (Dizziness Handicap Index, p = 0.019; fall index, p = 0.002) (Figure 1).
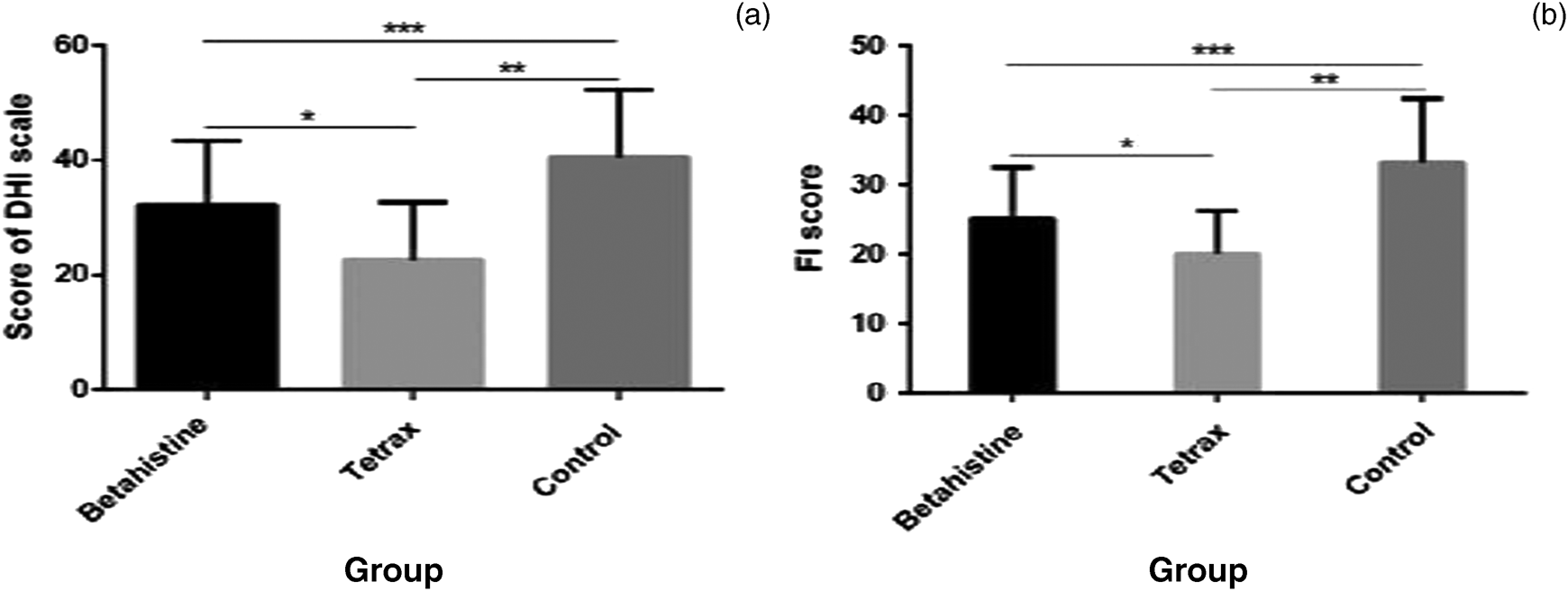
Fig. 1. Graphs showing: (a) the Dizziness Handicap Index (DHI) scores in the three groups after treatment, *p = 0.007, **p < 0.001, ***p = 0.019; and (b) the fall index (FI) scores in the three groups after treatment, *p = 0.041, **p < 0.001, ***p = 0.002. Values presented as mean ± standard deviation. Analysis of covariance was used to compare the improvements of Dizziness Handicap Index and fall index scores among the three groups, and the Bonferroni method was performed for comparison between groups.
Table 3. Dizziness Handicap Index and fall index scores

*n = 21; †n = 20; ‡n = 20. Values presented as mean ± standard deviation, unless indicated otherwise
Discussion
Ménière's disease is a common peripheral vestibular disease. In addition to vertigo symptoms, patients with Ménière's disease also experience dizziness and imbalance. Dizziness and imbalance will affect the patient's quality of life and increase their risk of falling. Studies have shown that patients with unilateral vestibular hypofunction have a higher risk of falling than healthy individuals.Reference Quitschal, Fukunaga, Ganança and Caovilla11,Reference Pothula, Chew, Lesser and Sharma12 In our study, we found a positive correlation between Dizziness Handicap Index and fall index scores in patients with Ménière's disease. This suggests that patients’ quality of life is positively correlated with the risk of falling in Ménière's disease patients with dizziness and imbalance.
Betahistine is a strong H3 receptor antagonist and a weak histamine H1 receptor agonist.Reference Magnan, Özgirgin, Trabalzini, Lacour, Escamez and Magnusson7 It is widely used in the management of vertigo and is the most frequently prescribed drug in Europe.Reference Lacour, van de Heyning, Novotny and Tighilet13,Reference Casani, Guidetti and Schoenhuber14 Regarding Ménière's disease, studies have indicated that betahistine is useful for the treatment of dizziness and vertigo during the inter-critical phase of the disease.Reference Casani, Guidetti and Schoenhuber14–Reference Murdin, Hussain and Schilder17
Tetrax biofeedback balance training is a vestibular rehabilitation protocol. Vestibular rehabilitation has been shown to be effective in improving the balance function of patients with peripheral vestibular dysfunction.Reference Hsu, Fang, Yeh, Su, Wang and Wang18,Reference Hillier and McDonnell19 In addition, vestibular rehabilitation reduces the risk of falling in patients with unilateral vestibular dysfunction.Reference Horning and Gorman20 Studies have also shown that it is a safe and effective management method in Ménière's disease.Reference Gottshall, Hoffer, Moore and Balough21,Reference McDonnell and Hillier22
In the present study, the Dizziness Handicap Index and fall index scores significantly decreased after treatment with betahistine or Tetrax biofeedback when compared with scores before treatment. It is argued that both betahistine and vestibular rehabilitation (Tetrax biofeedback) are effective in improving the quality of life and reducing the risk of falling in patients with Ménière's disease. These treatments are favourable for Ménière's disease patients with dizziness and imbalance.
We also found that post-treatment improvements, in terms of Dizziness Handicap Index and fall index scores, were significantly greater in the Tetrax group than the betahistine group. This may be because Ménière's disease patients are more dependent on vision and proprioception in maintaining balance;Reference Fujimoto, Egami, Kinoshita, Sugasawa, Yamasoba and Iwasaki5 vestibular rehabilitation can integrate visual, proprioceptive and residual vestibular function, reduce the fear of episodic vertigo, and improve patients’ confidence in maintaining balance.Reference Hsu, Fang, Yeh, Su, Wang and Wang18,Reference Yeh, Chen, Wang, Su, Chang and Tsai23
To our knowledge, the present study is the first to evaluate the effects of betahistine and vestibular rehabilitation (Tetrax biofeedback) on the quality of life and risk of falling in patients with Ménière's disease. The results of this study suggest that both interventions improved the quality of life and reduced the risk of falling in these patients, although vestibular rehabilitation was more effective than betahistine. However, two possible limitations in this study should be noted. First, given the short duration of our study, we do not know the long-term effects of betahistine and vestibular rehabilitation (Tetrax biofeedback). Second, we did not evaluate whether the improvements in quality of life and fall risk were maintained after completion of the programme.
• Ménière's disease patients experience dizziness and imbalance which negatively affects their quality of life and fall risk
• Both betahistine and vestibular rehabilitation are first-line management methods for Ménière's disease
• Patients treated with betahistine or vestibular rehabilitation (Tetrax biofeedback) showed significant improvements in Dizziness Handicap Index and fall index scores
• There were no such post-treatment improvements in the control group
• These improvements were significantly greater in the Tetrax group than the betahistine group
• Vestibular rehabilitation is better than betahistine in improving quality of life and reducing fall risk in Ménière's disease patients
Conclusion
Both betahistine and vestibular rehabilitation (Tetrax biofeedback) can improve the quality of life and reduce the risk of falling in patients with Ménière's disease, although vestibular rehabilitation was more effective than betahistine. The findings provide a reference for physicians on the management of Ménière's disease.
Acknowledgements
This study was funded by the Wu Jieping Medical Foundation (grant number: J1834).
Competing interests
None declared






