Introduction
Embryological remnants of the third or fourth branchial pouches are a rare but important cause of recurrent neck abscesses in children. They account for less than 2 per cent of all branchial arch defects.Reference Ford, Balakrishnan, Evans and Bailey1–Reference Nicollas, Ducroz, Garabedian and Triglia3 They may present as recurrent (usually left-sided) neck abscesses, unilateral suppurative thyroiditis or even as an airway-compromising parapharyngeal abscess.Reference Rea, Hartley and Bailey4, Reference Yang, Cohen, Everts, Smith, Caro and Andersen5 Patients will often have had multiple infective exacerbations and/or emergency incision and drainage procedures before a definitive diagnosis is made.
The remnant comprises a tract of varying extent. It is difficult clinically to differentiate between third and fourth branchial pouch remnants, even on surgical exploration. An internal opening, usually in the left piriform fossa, is a fairly constant feature of both; thus, the term piriform fossa sinus is preferred.Reference Kim, Sung, Roh and Han6 The distal extent may vary however, ranging from a stump confined within the thyroid cartilages to a complex tract passing through the neck into the mediastinum.Reference Rea, Hartley and Bailey4, Reference Liston7, Reference Godin, Kearns, Pransky, Seid and Wilson8 It is thought that seepage of pharyngeal content into the tract is what leads to suppuration in the neck.
Traditionally, complete excision of the sinus tract has been advocated in order to prevent recurrence.Reference Edmonds, Girod, Woodroof and Bruegger2, Reference Yang, Cohen, Everts, Smith, Caro and Andersen5, Reference Godin, Kearns, Pransky, Seid and Wilson8 This can be technically challenging, however, with a significant risk of damage to neurovascular structures, especially in a neck previously exposed to multiple inflammatory episodes as a consequence of repeated infection and/or drainage procedures. Moreover, recurrent suppuration may still occur even after extensive surgery.Reference Agaton-Bonilla and Gay-Escoda9
An alternative approach to management, originally reported by Jordan et al.,Reference Jordan, Graves, Manning, McClay and Biavati10 is ablation of the internal opening of the sinus tract in the piriform fossa via an endoscopic approach. It is thought that by closing the opening in the piriform fossa, the source of infection will effectively be cut off. This approach might render formal excision of the entire tract unnecessary, or it could be used as a treatment when previous excision of the tract has been unsuccessful.
We present our experience of four cases which were treated with diathermy ablation of the sinus opening in the piriform fossa. This was performed for recurrence after formal excision in the first three cases, and as an adjunct to formal excision in the fourth case.
Case reports
Patient one
A one-year-old girl presented to our hospital with a left anterior triangle neck abscess. She had previously had a similar swelling at one week of age, which on that occasion had been treated successfully with a course of intravenous flucoxacillin.
Ultrasonography revealed a cystic collection behind the left upper thyroid lobe. This appeared to communicate with the pharynx on contrast swallow, confirming the likelihood of a third or fourth branchial pouch sinus.
At operation, simultaneous pharyngoscopy identified the internal branchial sinus opening in the left piriform fossa, and a soft ureteric catheter was passed into it to assist in identification of the tract. The upper pole of the left thyroid gland was excised and the tract was ligated flush with the oesophagus.
The patient's post-operative course was unremarkable.
The patient remained asymptomatic until the age of five years, when she presented with an abscess in the same site as before. This discharged spontaneously, despite a course of intravenous flucloxacillin.
The patient was readmitted two months later. Direct pharyngoscopy was performed to reveal the patent sinus opening at the apex of the piriform fossa (Figure 1). An insulated Abbey diathermy needle, at a setting of 15 W (coagulation), was used to apply short one- or two-second bursts of monopolar diathermy to the mucosa of the opening, resulting in its obliteration (Figures 2 and 3).
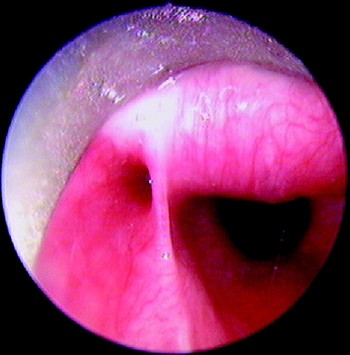
Fig. 1 Pharyngoscopic view of sinus tract opening in piriform fossa (on left) and post-cricoid opening into the oesophagus (on right).

Fig. 2 An insulated Abbey diathermy needle is used to apply monopolar electrocautery to obliterate the sinus opening.

Fig. 3 Sinus opening immediately after diathermy.
The patient was fed via nasogastric tube for two weeks, after which a further direct pharyngoscopy confirmed obliteration of the internal sinus opening (Figure 4). Oral feeding was then commenced successfully.
There was no evidence of recurrence at follow up nine months later, and the neck wound was fully healed.
Patient two
A one-year-old boy was initially referred with a continually discharging left neck wound following incision and drainage of an abscess when he was eight months old.
A contrast swallow revealed contrast leaking from the left piriform fossa.

Fig. 4 Healed sinus site, two weeks after diathermy treatment.
A formal neck exploration was performed; the tract was identified and traced proximally. It was ligated flush with the middle constrictor, which it entered. Apart from exuberant granulation tissue at the wound site, which settled after a few months, there were no other complications.
The patient remained well until two years later, when he presented with discharge of orally ingested fluids from the neck wound. Direct pharyngoscopy revealed a patent, epithelialised opening in the left piriform fossa.
An insulated Abbey diathermy needle was used to apply monopolar diathermy at a setting of 15 W (coagulation) to obliterate the sinus opening. The neck wound was simultaneously debrided.
The patient was kept nil by mouth and fed via a nasogastric tube for two weeks. There was no visible internal sinus opening on repeat pharyngoscopy at this time, and so oral feeding was commenced.
At the patient's last follow up appointment, 13 months later, there was no evidence of recurrence and the external wound had healed well.
Patient three
A seven-year-old girl was referred to our department with a history of recurrent (two episodes), left-sided neck abscess. On both occasions, these had discharged spontaneously.
A barium swallow demonstrated a sinus in the left piriform sinus.
The patient was diagnosed with a third branchial pouch sinus and underwent direct pharyngoscopy, which confirmed the presence of an internal sinus. At the same time, she underwent surgical excision of the sinus.
Her post-operative course was uneventful, and she was discharged two days later.
The patient remained well until two years later, when she presented with an abscess along the line of the surgical scar. This was incised and drained, but recurred twice over the following four months, requiring further incision and drainage procedures.
The patient was then admitted for endoscopic diathermy to the sinus opening. Monopolar diathermy was applied using a ureteric diathermy wire with a blunt tip, at a setting of 10 W (coagulation). She was discharged the same day.
A telephone interview 12 months after the procedure established that the patient had suffered no recurrence of neck abscess.
Patient four
A 10-year-old boy was referred to our hospital with a history of recurrent, left lower neck abscesses (four episodes over a five-year period). After the second abscess, an external opening had formed at the level of the anterior border of the sternocleidomastoid muscle, in its lower third. Subsequent episodes had been associated with discharge from this opening. On each occasion, the acute infection had been successfully treated conservatively with intravenous antibiotics.
A barium swallow indicated a piriform fossa sinus.
Direct pharyngoscopy under general anaesthesia confirmed the internal sinus opening at the apex of the left piriform fossa. This was cauterised with a monopolar, insulated ureteric catheter set at 15 W. An elliptical incision around the external neck opening exposed a tract, which was traced past the superior pole of the thyroid gland and ligated flush with the inferior constrictor, just posterior to the thyroid cartilage. Oral feeding was successfully commenced 24 hours later, and the patient was discharged home.
There was no evidence of recurrence at 27 months' follow up.
Discussion
The traditional management of a symptomatic third or fourth branchial pouch remnant or piriform fossa sinus is to completely excise the tract via an external neck approach, tracing it up to its origin in the piriform fossa.Reference Edmonds, Girod, Woodroof and Bruegger2, Reference Yang, Cohen, Everts, Smith, Caro and Andersen5, Reference Godin, Kearns, Pransky, Seid and Wilson8 This involves negotiating the superior pole of the thyroid gland (often excising it, as in patient one) and, more importantly, the recurrent and superior laryngeal nerves, the latter being a key landmark in distinguishing a third from a fourth branchial pouch. A third pouch tract leaves the piriform sinus in its superior aspect, pierces the thyrohyoid membrane and courses laterally above the superior laryngeal nerve and inferior constrictor (both fourth arch derivatives). In contrast, a fourth pouch tract leaves the apex of the piriform sinus and courses inferior to the superior laryngeal nerve to exit the larynx under the ala of the thyroid cartilage and the inferior constrictor muscle (all fourth arch derivatives).
In reality, the distinction between a third and fourth pouch tract is difficult, even with complete surgical exposure, and it is for this reason that they are grouped together under the term ‘piriform fossa sinuses’. The cricothyroid joint may need to be disarticulated and the thyroid ala mobilised anteriorly in order to gain access to the piriform fossa.Reference Yang, Cohen, Everts, Smith, Caro and Andersen5 Such technically challenging surgery may still leave behind a proximal stump which remains prone to recurrent infection, as occurred with three of our cases (patients one, two and three). In a series of patients with third and fourth branchial pouch abnormalities previously treated at our institution, there were two cases of recurrence out of seven cases treated by excision of the entire sinus tract.Reference Rea, Hartley and Bailey4 The recurrences occurred a year after surgical treatment. In the current series, in the three cases of recurrence following surgical excision of the tract, two (patients two and three) occurred two years after surgery, while the other (patient one) occurred four years after the original operation. Other series have quoted no recurrence after surgical excision, but this may be related to a relatively short period of follow up.Reference Pereira, Losh, Oliver and Poole11
• Third and fourth branchial pouch remnants or ‘piriform fossa sinuses’ present as recurrent (usually left-sided) neck abscesses
• There is an internal opening in the left piriform fossa, which is thought to be the entry point for infection
• Traditional management comprises surgical excision of the entire tract, a procedure that can be technically challenging
• Endoscopic diathermy to the piriform fossa sinus is a safe and effective technique that can be used as an adjunct to open excision or as a treatment for recurrence following external excision
The source of infection associated with these pouch sinuses is likely to be pharyngeal content that has seeped into the sinus. Obliteration of the proximal aspect of these sinuses as a primary procedure should therefore prevent this mechanism of abscess formation and obviate the need for a difficult neck exploration. Electrocautery appears to be an effective means of achieving this. Our four cases showed no sign of recurrence after follow-up periods ranging between nine and 27 months. Our results are comparable to those reported by Verret et al. Reference Verret, McClay, Murray, Biavati and Brown12 After neck abscess drainage, these authors obliterated the internal sinus opening of 10 patients, using electrocautery. Only one of their 10 cases had previously undergone open excision of the sinus tract. Seven of the 10 were available for follow up (average three years). None had abscess recurrence or complications. Another series reported seven children successfully treated with cautery to the sinus opening only.Reference Jordan, Graves, Manning, McClay and Biavati10 It must be stressed that electrocautery should be applied in short bursts to the superficial mucosal layers, to avoid perforation or damage to surrounding anatomy, including the superior laryngeal nerve.
Kim et al. Reference Kim, Sung, Roh and Han6 described an alternative means of obliterating the internal sinus opening. They applied trichloroacetic acid (concentration 10–40 per cent) to the internal sinus opening in 16 patients. Follow up ranged from one to 70 months. There were four incidences of recurrence, two of which had persistent internal sinus openings. These two patients responded successfully to reapplication of trichloroacetic acid, whilst the other two patients required neck exploration and sinus tract excision. An advantage of chemocauterisation in this setting may be its distal penetration into the tract. However, it may not be as effective as electrocautery in causing tissue inflammation and adherence, thus necessitating repeat application.Reference Kim, Sung, Roh and Han6, Reference Stenquist, Juhlin, Astrom and Friberg13 In addition, there is a risk of accidental spillage down the oesophagus, leading to stricture formation. More recently, endoscopic laser coagulation has been used to seal the piriform fossa opening.Reference Sayadi, Gassab, Dellai, Mekki, Golli and Elkadhi14
We were cautious about introducing immediate post-operative oral feeding in patients one and two. These patients had complex clinical and surgical histories, and it was plausible that recurrent inflammation in the vicinity may have predisposed to slower wound healing, enhancing the likelihood of reopening of the sinus. In order to prevent this, these patients were fed via nasogastric tube for two weeks post-operatively. Oral feeding was commenced after pharyngoscopic confirmation of obliteration. However, other authors have successfully commenced feeding as early as the second post-operative day,Reference Kim, Sung, Roh and Han6, Reference Jordan, Graves, Manning, McClay and Biavati10, Reference Verret, McClay, Murray, Biavati and Brown12 as was done in our patients three and four.
Closure of the piriform sinus opening in an unexplored neck will leave a completely closed sinus remnant. It is unclear whether these enclosed spaces persist or self-obliterate. The latter is likely in the context of inflammation. In any case, necks treated in this fashion have remained clinically silent.Reference Kim, Sung, Roh and Han6, Reference Jordan, Graves, Manning, McClay and Biavati10, Reference Verret, McClay, Murray, Biavati and Brown12–Reference Sayadi, Gassab, Dellai, Mekki, Golli and Elkadhi14 However, it must be acknowledged that the period of follow up for such a young population has been relatively short.
Conclusion
The relative rarity of third and fourth branchial pouch anomalies often leads to recurrent drainage procedures prior to a definitive diagnosis. Clinicians should be suspicious of such pathology in all cases of recurrent, unilateral (especially left-sided) neck abscess, and should consider performing a contrast swallow examination and an early diagnostic pharyngoscopy. Obliteration of the internal opening of these sinuses by endoscopic diathermy is a safe and effective management option for this condition, as an adjunct to open surgical excision of the tract.






