Introduction
A diagnosis of chronic otitis media implies a permanent abnormality of the pars tensa or flaccida, probably resulting from earlier acute otitis media, negative middle-ear pressure or otitis media with effusion. There is a distinction between active (where there is inflammation and pus production) and inactive (where there is not, although the ear may become active at some time) forms of chronic otitis media.Reference Browning, Gleeson, Browning and Burton1 The aim of chronic otitis media treatment is to improve the symptoms of otorrhoea, close the perforation, improve hearing and reduce the number of complications, with the minimum of adverse effects. Tympanoplasty is a common procedure for treating these patients.
In the underlay and overlay techniques, graft placement is medial or lateral to the fibrous layer of the tympanic membrane, respectively, as described by House and Shea.Reference House2, Reference Shea3 Some authors have reported a modified method in which the graft is placed lateral to the malleus and medial to the tympanic remnant and annulus.Reference Stage and Bak-Pedersen4–Reference Kartush, Michaelides, Becvarovski and LaRouere6 This ‘over-underlay’ technique provides excellent exposure of the anterior middle ear, facilitates direct placement of an ossicular prosthesis under the malleus and minimises the risk of tympanic membrane medialisation or lateralisation. The over-underlay technique is reported to have excellent results in terms of graft take, absence of complications and auditory outcome.Reference Potsic, Winawer and Marsh5–Reference Yigit, Alkan, Topuz, Uslu, Unsal and Dadas7 However, success depends on many factors, and the presence of discharge before surgery makes it difficult to decide whether to operate or not. There are also contradictory reports of tympanoplasty results related to the condition of the ear at the time of surgery. Several authors reported that attempts to repair a perforation fail significantly more often in a wet ear than in a dry ear, whereas others have found no difference in outcome between the two conditions.Reference Tos8–Reference Sade, Berco, Brown, Weinberg and Avraham13 In theory, the success rate also depends on the vascularity of the remnant tympanic membrane. The graft failure risk was reported to be higher for an avascular than for a vascularised tympanic membrane.Reference Vijayendra, Rangam and Sangeeta14
This prospective study aimed to evaluate the type I tympanoplasty outcome and the tympanic membrane vascular status in dry and wet ears.
Materials and methods
Two groups of chronic otitis media patients were selected according to their presentation: wet or dry ear. One group comprised 35 consecutive patients with dry ear and another comprised 35 consecutive patients with discharge (wet ear) at the time of presentation to the operating surgeon (RSV) and during surgery. This prospective study was conducted at a tertiary care referral centre (the Postgraduate Institute of Medical Education and Research, Chandigarh, India) between January 2010 and June 2011. Patients with history of discharge for at least six weeks were included. Patients aged over 15 years (both sexes), with tympanic membrane perforation of any size and location, and mild to moderate conductive hearing loss were included. Patients with cholesteatoma and/or granulation tissue, sensorineural hearing loss, prior attempts at tympanic membrane repair, and any history of trauma to the tympanic membrane were excluded.
For all patients, surgery was performed under local anaesthesia through a standard post-auricular approach by the same surgeon. The post-auricular area and ear canal were infiltrated with 1 per cent xylocaine containing a 1 in 100 000 adrenaline solution. The perforation margin was then freshened and a piece of the remnant tympanic membrane was sent for histopathological examination. In a few patients with marginal perforations, the sample size was insufficient for histopathological examination. Thus, post-operative histopathological reports on the vascularity of the tympanic membrane margin could only be obtained for 46 out of 70 patients.
The over-underlay technique was performed for all patients. For this, a post-auricular Wilde's incision was made, followed by elevation of the subperiosteal flap. The spine of Henle was identified and the external auditory canal was entered just medial to it. After obtaining adequate exposure, a medial circumferential incision was made from the 11 o'clock to the 1 o'clock position (for the right ear) or the reverse (for the left ear), followed by elevation of the tympanomeatal flap along with the annulus of the tympanic membrane (Yung's technique). The mucosal covering of the handle of the malleus was removed, and the ossicular chain status and eustachian tube orifice were examined. A freshly harvested temporalis fascia graft was placed over the handle of the malleus and the remnant tympanic membrane. The fascia was then tucked under the annulus (all around) and the tympanomeatal flap was repositioned. The external auditory canal was packed with Gelfoam®, the wound closed in two layers and a mastoid dressing applied.
Post-operatively, patients were followed for a minimum of one year, with assessment of the wound status, graft status and hearing improvement. Histopathology reports on the remnant tympanic membranes were noted for both patient groups.
Statistical analysis
All categorical data were compared between groups using the chi-square test. Quantitative data were analysed using the Kolmogorov–Smirnov test. Paired t-tests were used to compare pre- and post-operative pure tone audiometry values within groups. The mean change in pure tone audiometry values (pre- and post-operative) were compared between the two groups using the Student's t-test. Descriptive statistics (e.g. mean and standard deviation) were calculated for measurable data and frequency and/or percentages values for categorical data. Logistic regression was used to analyse the influence of multiple variables on treatment outcome. Statistical significance was set at a p value of less than 0.05.
Results
There were no significant differences in patient demographics between the dry ear (n = 35) and wet ear (n = 35) groups (Table I).
Table I Comparison of patient demographic and success rates between the two groups

*p < 0.05
Pre-operative mean air conduction threshold measurements showed normal hearing (less than 25 dB hearing loss) in 22 patients (12 with dry ear, 10 with wet ear), mild hearing loss (26–40 dB) in 36 patients (15 with dry ear, 21 with wet ear), moderate hearing loss (41–55 dB) in 11 patients (7 with dry ear, 4 with wet ear) and moderately severe hearing loss (55–70 dB) in only 1 patient (with dry ear).
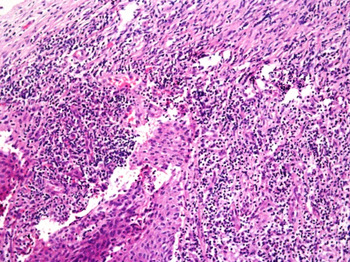
Intra-operative assessment showed that 51 patients had healthy middle-ear mucosa: 35 in the dry ear group and 16 in the wet ear group. All 19 patients in the wet ear group had oedematous mucosa. Ossicular status was assessed intra-operatively: 66 patients had intact, mobile ossicles and 4 patients had restricted ossicular mobility with associated middle-ear tympanosclerosis. Histopathological examination of tympanic membrane biopsies from 46 patients showed no evidence of vascularity in 27 (18 with dry ear, 9 with wet ear; Fig. 1) and evidence of vascularity in 19 (3 with dry ear, 16 with wet ear; Fig. 2).

Fig. 1 High power photomicrograph showing a tympanic membrane remnant with no evidence of vascularity. (H&E; ×450)
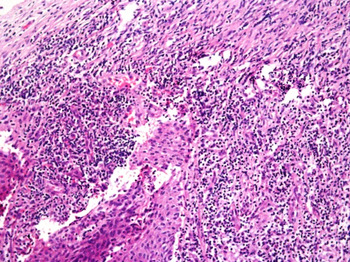
Fig. 2 High power photomicrograph showing a tympanic membrane with evidence of vascularity. (H&E; ×450)
The mean follow up was 1.2 years, with a minimum of 1 year. The overall success rate was 84 per cent (59 out of 70), with a success rate of 89 per cent (31 out of 35) in the dry ear group and 80 per cent (28 out of 35) in the wet ear group. The total failure rate in the study group was 16 per cent (11 per cent in the dry ear group, 20 per cent in the wet ear group).
Histopathological examination of the tympanic membrane remnant showed evidence of vascularity in 19 patients. Of these, graft uptake was successful in 18 and failed in 1. In all, 27 patients showed no evidence of vascularity. Within this group, graft uptake was successful in 21 patients and failed in 6. Thus, there was no significant relationship between tympanoplasty success and tympanic membrane vascularity (p = 0.115).
The success rate was 100 per cent for small perforations, 81 per cent for medium-sized perforations and 86 per cent for large perforations. Although there was a small but significant increase in the success rate for small perforations (six patients), the overall success rate was not influenced by perforation size in both the dry and wet groups (Table I). Whether the discharge was mucoid or mucopurulent did not influence the graft uptake success rate (p = 0.526), and there was no significant difference in success rate between the combined discharge types and the dry ear group (p = 0.324).
Discussion
This study included both inactive (dry) and active (wet) mucosal chronic otitis media.Reference Browning and Kerr15 Inactive mucosal chronic otitis media has a permanent tympanic membrane defect with no evidence of infection or discharge. In these patients, ears may remain inactive, become active or, occasionally, heal. In active mucosal chronic otitis media, there is evidence of active discharge and inflamed middle-ear mucosa, sometimes with granulation tissue which can become polypoidal. This condition may remain active, become inactive or progress to complications.
Surgery plays an important role in the management of chronic otitis media. Factors such as patient age, perforation aetiology, disease stage, perforation size and site, the presence of tympanosclerosis, middle-ear mucosa condition, eustachian tube function, type of graft material, surgical technique (overlay or underlay), and operating surgeon experience are not reported to influence the success rate.Reference Vartiainen and Nuutinen16–Reference Landa Aranzábal, Rodríguez García, Rivas Salas, Navarro Sampedro, Camacho Arrioaga and Algaba Guimera19
This study analysed the influence of age and illness duration on tympanoplasty success rate. The results showed that the success rate was not significantly different between patient groups. Similarly, Vartiainen and Nuutinen reported that age distribution did not influence the success rate in adults.Reference Vartiainen and Nuutinen16 Sckolnick et al. reported a poor success rate for chronic ear perforation.Reference Sckolnick, Mantle, Li and Chi20
In this study population, 61 per cent of the patients had a history of decreased hearing and 24 per cent had a history of tinnitus. No patient had vertigo or facial nerve palsy; decreased hearing and a history of ear discharge were the main presenting complaints. Sheahan et al. reported that 78 per cent of chronic otitis media patients presented with decreased hearing, 64 per cent with otorrhoea and 9 per cent with a history of dizziness and vertigo.Reference Sheahan, Donnelly and Kane21
The aim of developing the modified over-underlay tympanoplasty technique (combining the underlay and overlay techniques) was to minimise the inherent disadvantages of both techniques. Stage and Bak-Pedersen and Kartush et al. support the over-underlay procedure.Reference Stage and Bak-Pedersen4, Reference Kartush, Michaelides, Becvarovski and LaRouere6 In our patients, the tympanomeatal flap was elevated as described by Yung and fresh temporalis fascia was used for grafting.Reference Yung18 Graft placement was performed via the over-underlay technique.Reference Vartiainen and Nuutinen16, Reference Loock and Naude22 The overall success rate was 84 per cent: 89 per cent for dry ear patients and 80 per cent for wet ear patients. The overall failure rate in our study group was 15.7 per cent: 11.4 per cent for those with dry ear and 20 per cent for those with wet ear. In patients with wet ear, the success rate was not affected by discharge type (p = 0.526). The success rate in this study is comparable with those of other studies using the over-underlay technique. Stage and Bak-Pedersen reported a success rate of 91 per cent for 39 ears.Reference Stage and Bak-Pedersen4 A similar success rate (90 per cent) was achieved by Kartush et al. in a series of 120 patients who underwent over-underlay tympanoplasty.Reference Kartush, Michaelides, Becvarovski and LaRouere6 In a series of 273 ears, Glasscock reported a success rate of 91 per cent using the overlay technique and of 96 per cent using the underlay technique.Reference Glasscock23 Sheehy and colleagues reported a success rate of 97 per cent for 472 overlay tympanoplasty procedures.Reference Sheehy and Anderson24 Rizer reported success rates of 95.6 per cent in a series of 554 overlay grafts, 88.8 per cent for 158 underlay grafts and 91.4 per cent for 46 underlay grafts.Reference Rizer25, Reference Rizer26
The success rate in this study was similar between patients with dry and wet ears (p = 0.324). However, previous reports are contradictory. Nagle et al. reported an insignificant difference in success rate between patients with dry or wet ears.Reference Nagle, Jagade, Gandhi and Pawar27 However, a prospective audit study by Kotecha et al. that reviewed 1070 individuals showed that patients with dry ear or mucoid, serous or purulent discharge had failure rates of 17.7 per cent, 17.1 per cent, 11.8 per cent and 17.2 per cent, respectively.Reference Kotecha, Fowler and Topham28 Moreover, Vartiainen and Nuutinen reported success rates of 87.5 per cent and 70 per cent for dry and wet ears, respectively.Reference Vartiainen and Nuutinen16 A study by Raj and Tripathi of wet ear patients undergoing myringoplasty showed primary perforation closure in 84 per cent.Reference Raj and Tripathi29 Gersdorff et al. compared 53 dry ear patients with 20 wet ear patients and reported success rates of 79.2 per cent and 50 per cent, respectively.Reference Gersdorff, Garin, Decat and Juantegui30 In another study, Onal et al. reported success rates of 44.4 per cent for wet ear and 71 per cent for dry ear.Reference Onal, Uguz, Kazikdas, Gursoy and Gokce31 Other authors have reported that attempts to repair perforations fail significantly more often in wet ears than in dry ears.Reference Tos8–Reference Booth10
For our study group, histopathological reports were available for 46 patients. Patients with wet ear had significantly more tympanic membrane vascularity compared with dry ear patients (p < 0.001). However, the absence of vascularity in patients with dry ear could be due to sparse vascularity which could not be detected by routine histopathology. There was no significant difference in the success rate between the two patient groups (p = 0.115).
• Type I tympanoplasty success is not influenced by the presence of ear discharge
• Tympanic membrane vascularity does not influence graft uptake
• The over-underlay method provides excellent exposure of the anterior middle ear
• The complication risk is minimised by proper placement of graft anteriorly
This study showed that although the success rate was slightly higher for small perforations, the overall success rate was not influenced by perforation size. Many studies have reported that perforation size inversely correlates with successful operative closure, but others have reported that perforation size is not a determinant of surgical success.Reference Kotecha, Fowler and Topham28, Reference Gersdorff, Garin, Decat and Juantegui30, Reference Bhat and De32–Reference Lee, Kelly and Mills35 Our study has shown that perforation size is not predictive or a determinant of successful tympanoplasty.
Conclusion
A prospective analysis of type I tympanoplasty in wet and dry ears including histopathological analysis of the tympanic membrane showed that success rate is not influenced by the presence of ear discharge at the time of surgery and that tympanic membrane vascularity does not influence graft uptake. The over-underlay method provides excellent exposure of the anterior middle ear, and the risk of anterior blunting and graft lateralisation are minimised by proper placement of graft anteriorly.