Introduction
The increasing elderly population in developed countries is unprecedented, poised to become a central social transformation with implications for all sectors of 21st-century society. According to the statistical office of the European Union, the number of older people aged 65+ in the 27 European Union countries is predicted to follow an upward trend, with a relative share of the total population of approximately 28.5 per cent in 2050 (European Commission – Eurostat, 2019). The Revised World Population Prospects 2019, created by the Department of Economic and Social Affairs from the United Nations Secretariat, also predicts that by 2050 one in four persons living in Europe and North America could be aged 65 or over (United Nations, 2019). This growing sector of the population will demand products and services that are appropriate for their needs. Since older people are increasingly active, wanting to maintain their autonomy and stay integrated in the environment around them, a challenge for global society will be to afford them the means and opportunities to age actively and healthily.
Over the past decades, recreational gambling has become an increasingly popular leisure activity among older adults, and potential health and wellbeing correlates have been described (such as opportunities for socialisation, and sensory and cognitive stimulations) (Desai et al., Reference Desai, Maciejewski, Dausey, Caldarone and Potenza2004). But the proliferation of multiple favoured gambling activities in elderly people during the last years (such as slot machines, bingo, lotteries or casinos) (Ariyabuddhiphongs, Reference Ariyabuddhiphongs2012; Medeiros et al., Reference Medeiros, Leppink, Yaemi, Mariani, Tavares and Grant2015; Granero et al., 2020), and the growth rate of gambling participation among older adults (largely as a consequence of the ageing population and the ease of access to multiple platforms offering numerous forms of offsite/online gambling), make necessary a wide investigation of health correlates, particularly for problem and disordered gambling. The diverse personal and contextual circumstances of gambling, as well as the different impacts on the physical and psychological states, must be recognised for preventing the progression from recreational gambling to problematic and/or disordered gambling. This study is aimed at identifying profiles of older-age gamblers and potential risk factors for impairing gambling, the results of which can contribute for preventing unnecessary dependence and guaranteeing functional autonomy (which is the core condition of successful ageing).
Positive active ageing
As in other health research areas, there is no consensus regarding the definition of old age in the context of gambling disorder (GD) (substantially variations in literature exist, usually from age 50+ to 75+ years). Indeed, since the age which qualifies as elderly in health studies is related to a large set of personal and contextual features (such as medical conditions, geographical areas or culture), it is difficult to achieve a standardised universal definition. Global organisations such as the World Health Organization (WHO) do not provide a clear definition either, and although fixing around 60–65 as the beginning of being elderly, WHO (2018) also recognises that old age should be defined by new roles and not by years. As a result, some studies based on a population-ageing metric focused on a chronological conception of age and set the boundary of 60–65 as the beginning of being elderly, coinciding with administrative purposes (this threshold is required for becoming eligible for senior social programmes and retirement), and with the idea that above these ages the resources required to support individuals increase. Other works consider the onset of old age as 50+ years, considering that at this age a variety of biopsychological changes can cause health to decline, with higher likelihood of physical and mental conditions (Skoog, Reference Skoog2011; Di Rosa et al., Reference Di Rosa, Mapelli, Arcara, Amodio, Tamburin and Schiff2017). Research among elderly in the GD area is scarce compared with the large number of works within other age groups, which makes it even more difficult to reach consensus on the onset of old age. Our study selected 50+ as the lower boundary since this cut-off coincides with current studies analysing the profiles and determinants of GD in elderly people (Guillou Landreat et al., Reference Guillou Landreat, Cholet, Grall Bronnec, Lalande and Le Reste2019).
Traditionally, it has been widely considered that many changes that occur in old age are negative, and with advanced age many skills acquired during the preceding stages of life are lost. Certainly, during the elderly stage, losses in both cognitive and physical abilities occur (Fabricio et al., Reference Fabricio, Chagas and Diniz2020; Ungvari et al., Reference Ungvari, Tarantini, Sorond, Merkely and Csiszar2020), with an ongoing impairment in skills related to fluid intelligence (such as working/episodic memory, reasoning or even spatial orientation) and mobility being typical. High rates in the global consumption of health-care systems in parallel with ageing reinforce the assumption of ageing deterioration (Ahmad et al., Reference Ahmad, Mat Ludin, Shahar, Mohd Noah and Mohd Tohit2020), which has largely conditioned the products and services made available to this sector of the population (most of them addressed towards relieving the impacts of such changes and deficiencies). These views are not consistent with the empirical data provided by current research on ageing, which reveal that many older people who reach retirement age remain healthy, active and with a capacity to undertake new challenges (Platzer et al., Reference Platzer, Singler, Dovjak, Wirnsberger, Perl, Lindner, Liew and Roller-Wirnsberger2020). Despite the typical ageing-specific deterioration in functional abilities, empirical research also highlights that healthy older people have behavioural plasticity (Navarro and Calero, Reference Navarro and Calero2018), and if stimulating environments are provided, behavioural benefit habits can also be adopted and/or modified (Martin et al., Reference Martin, Palmer, Rock, Gelston and Jeste2015; Bendayan et al., Reference Bendayan, Piccinin, Hofer, Cadar, Johansson and Muniz-Terrera2017). Accurate knowledge of the factors related to the social and structural determinants of wellbeing are required to improve further the challenges of effectively managing the care needs of the community's older adults, with the aim of maintaining adequate levels of function and restoring any lost abilities.
Participation in leisure activities positively affects multiple aspects of human behaviour, and it has been identified as a crucial predictor of life satisfaction in the lifecycle (Browne et al., Reference Browne, Rawat, Greer, Langham, Rockloff and Hanley2017; Browne and Rockloff, Reference Browne and Rockloff2018; Farrell, Reference Farrell2018; Blackman et al., Reference Blackman, Browne, Rockloff, Hing and Russell2019). Gambling is also a widespread leisure activity in elderly individuals, who tend to perceive certain betting games as a nice break from routine life and a way of socialising (Subramaniam et al., Reference Subramaniam, Satghare, Vaingankar, Picco, Browning, Chong and Thomas2017b). Numerous positive effects of recreational gambling have been reported among older ages, such as increasing levels of happiness, improving mood states, addressing loneliness (a typical situation among older-age individuals who have lost a partner and/or other loved ones), contributing to greater social support (some forms of gambling lead individuals to socialise and interact with their fellow elders), helping alleviate feelings of uselessness (also common after retirement), and even enabling skills to be picked up (individuals learn to be more observant, and some games of skill can exercise the brain and help keep the mind active and working) (Dixon et al., Reference Dixon, Nastally and Waterman2010; Hilbrecht and Mock, Reference Hilbrecht and Mock2019). Several harmful effects affecting quality of life have also been associated with gambling across the spectrum of risk levels among older people, who are likely to present multiple and severe negative consequences when they lose control of the gambling activity. It is therefore necessary to review the key components of the GD as a mental psychiatric condition, and identify the specific profile/s of this disorder when it occurs in old-age subjects.
Gambling activity and older age
GD is defined as a psychiatric condition in which individuals display a recurrent maladaptive gambling activity (people report persistent difficulties in limiting money or time spent on gambling), with severe consequences or impairment in several areas (psychological functioning, work performance, monetary status and family/social relationships). In fact, gambling activity can be considered to be a continuous vector, ranging from none to a great deal. Depending on the points along this continuum, individuals can experience impairment and problems associated with their gambling behaviour and, therefore, the position in the range can be considered to be a measure of the gambling severity. For example, the most recent edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5; American Psychiatric Association, 2013) offers a classification of the GD symptom severity boundaries defined by the number of criteria met out of a maximum of nine: mild GD (four or five criteria), moderate GD (six or seven criteria) and severe GD (eight or nine criteria).
Current epidemiological studies have attempted to estimate and compare the prevalence of gambling involvement, problematic gambling and GD across age groups. Although the estimates among older adults show substantial differences depending on the classification schemes, sampling procedures, age thresholds and measurement tools, it seems that between 62 and 75 per cent of individuals recruited from general populations reported having gambled in the last year (Welte et al., Reference Welte, Barnes, Tidwell and Hoffman2011; Tse et al., Reference Tse, Hong, Wang and Cunningham-Williams2012; Takamatsu et al., Reference Takamatsu, Martens and Arterberry2016), and between 0.5 and 6 per cent met the criteria for current pathological gambling or disordered gambling (Tse et al., Reference Tse, Hong and Ng2013; Subramaniam et al., Reference Subramaniam, Wang, Soh, Vaingankar, Chong, Browning and Thomas2015; Calado and Griffiths, Reference Calado and Griffiths2016). Some epidemiological research also suggests than the telescoping effect is typical in older age (gambling problems develop more quickly than in younger age groups) (Bjelde et al., Reference Bjelde, Chromy and Pankow2008), and that ageing-related cognitive distortions are main contributors to this phenomenon and to maintaining and exacerbating gambling problems (Subramaniam et al., 2017a).
Motivations for gambling among elderly people can be similar to those identified in younger adults, including social interaction, fun/excitement and relief from emotional distress (Ariyabuddhiphongs, Reference Ariyabuddhiphongs2012). Some studies have identified specific age-related environmental and individual-level factors that could act as motivators for elderly individuals to initiate and/or maintain their gambling habits: relieving boredom (people may have more free time than expected upon retirement), escaping loneliness and social isolation, relieving tension or coping with depression due to the loss of a loved one, or winning money (Tira et al., Reference Tira, Jackson and Tomnay2014; Medeiros et al., Reference Medeiros, Leppink, Yaemi, Mariani, Tavares and Grant2015; Subramaniam et al., Reference Subramaniam, Wang, Soh, Vaingankar, Chong, Browning and Thomas2015). Cognitive decline and physical-mental illness also play a role in the onset, maintenance and escalation of gambling behaviours among older adults (Pilver et al., Reference Pilver, Libby, Hoff and Potenza2013; Subramaniam et al., Reference Subramaniam, Chong, Browning and Thomas2017a; Parke et al., Reference Parke, Griffiths, Pattinson and Keatley2018). It is well known that the brain becomes more vulnerable with age, with typical neuroanatomical and neurochemical changes that can lead to multiple deficits in cognitive functioning and executive control. The affectation in frontal structures during elderly correlates with reasoning slowness, lower ability to shift attention from positive to negative information, limited ability to gain explicit insight into the rules of ambiguous decision tasks and the difficulty of choosing the less risky events after the rules have been fully understood (Schiebener and Brand, Reference Schiebener and Brand2017). These potential interactions have been proposed as powerful risk factors for the onset of gambling-related problems during the old-age stage in lifetime gamblers who had no such difficulties during early adulthood (McCarrey et al., Reference McCarrey, Henry, von Hippel, Weidemann, Sachdev, Wohl and Williams2012). A relationship has also been suggested between the increases in the gambling severity, with higher levels of impulsivity among older-age individuals who exhibit cognitive deficits (von Hippel et al., Reference von Hippel, Ng, Abbot, Caldwell, Gill and Powell2009). The cognitive distortions related to the illusion of control observed within older adult gamblers (who persistently belief that they have special skills, knowledge or other advantages for controlling the gambling outcome) seems to play a key role in both maintaining and increasing the severity of gambling behaviours (especially the self-perceived concept of luck, chasing wins/losses, miscalculating the win/loss ratio, superstitious beliefs and the perception that gambling is a skill) (Subramaniam et al., Reference Subramaniam, Chong, Browning and Thomas2017a). Finally, it has been observed that at older age when gambling becomes a problematic behaviour, the motivations may change: while some individuals may begin to gamble for excitement or to combat boredom, the reasons can shift towards managing stress, guilt or emotional distress when they lose control of their gambling habits (Pattinson and Parke, Reference Pattinson and Parke2017). It has also been observed that the increased availability of multiple forms of gambling in recent years (a high number of systems are now operating online) will also affect gambling motivations and habits in older adults, who can easily find numerous and stimulating media to gamble (Sauvaget et al., Reference Sauvaget, Jiménez-Murcia, Fernández-Aranda, Fagundo, Moragas, Wolz, Veciana De Las Heras, Granero, del Pino-Gutiérrez, Baño, Real, Aymamí, Grall-Bronnec and Menchón2015; Luce et al., Reference Luce, Kairouz, Nadeau and Monson2016; Ioannidis et al., Reference Ioannidis, Treder, Chamberlain, Kiraly, Redden, Stein, Lochner and Grant2018).
Regarding gambling preferences, older adults tend to engage in particular forms of gambling, including lottery tickets, bingo and slot machines (Ariyabuddhiphongs, Reference Ariyabuddhiphongs2012; Moragas et al., Reference Moragas, Granero, Stinchfield, Fernández-Aranda, Fröberg, Aymamí, Gómez-Peña, Fagundo, Islam, del Pino-Gutiérrez, Agüera, Savvidou, Arcelus, Witcom, Sauchelli, Menchón and Jiménez-Murcia2015; Bangma et al., Reference Bangma, Fuermaier, Tucha, Tucha and Koerts2017; Jiménez-Murcia et al., Reference Jiménez-Murcia, Granero, Fernández-Aranda and Menchón2020). These games are included within the group labelled non-strategic games (also called chance-based games), characterised by the individual's lack of capacity or skill to influence the game outcome (Odlaug et al., Reference Odlaug, Marsh, Kim and Grant2011). On the contrary, strategic games (also called skill-based games) allow gamblers to use game-related knowledge to influence/predict the game outcome (such as poker and other cards, betting on sports events or dice). It has been argued that elderly individuals are more likely to gravitate towards non-strategic games based on their simplicity, since this gambling behaviour involves quick, unplanned, reward-driven decisions, and little deliberation (Grant et al., Reference Grant, Odlaug, Chamberlain and Schreiber2012; Subramaniam et al., Reference Subramaniam, Abdin, Vaingankar, Shahwan, Picco and Chong2016; Schiebener and Brand, Reference Schiebener and Brand2017). It must be underlined that the characterisation of ‘non-strategic’ is based on the mechanism of the game (the outcomes are 100% chance depending), while non-strategic players also hold cognitive biases related to their gambling behaviours (such as irrational fallacies/perceptions regarding their capacity predicting gambling outcomes). Some studies in the neuropsychological area suggest that the specific age-related vulnerabilities of the brain should contribute towards explaining the preference for chance-based games: potential impairment in frontal structures could affect risky decision-making tasks, causing reasoning slowness and poor ability to gain explicit insight into the rules of ambiguous decisions, or even difficulty in choosing less risky events even when the rules have been processed (Boggio et al., Reference Boggio, Campanhã, Valasek, Fecteau, Pascual-Leone and Fregni2010; Lorains et al., Reference Lorains, Dowling, Enticott, Bradshaw, Trueblood and Stout2014; Lorenz et al., Reference Lorenz, Gleich, Beck, Pöhland, Raufelder, Sommer, Rapp, Kühn and Gallinat2014; Halfmann et al., Reference Halfmann, Hedgcock, Kable and Denburg2016; Di Rosa et al., Reference Di Rosa, Mapelli, Arcara, Amodio, Tamburin and Schiff2017; Schiebener and Brand, Reference Schiebener and Brand2017). It must be outlined, however, that multiple factors contribute on gambling preferences among older subjects, and the choice of gambling varies according to the individual and social/contextual characteristics. For example, casino trips, scrabble clubs or card games are perceived by some elderly people as a playful socialisation activity. Availability and legislation can also impact on gambling practices, particularly among vulnerable people (such as old-age people) (Medeiros et al., Reference Medeiros, Leppink, Yaemi, Mariani, Tavares and Grant2015).
Finally, problematic and disordered gambling in older adults has been found to be associated with multiple negative outcomes. Many of the harmful effects of addictive gambling are similar across age, including low self-esteem, impaired relationships with family and friends, social isolation, financial problems, and poor physical and/or mental health (such as more obesity-related conditions, higher levels of anxiety and depression, substance abuse/dependence) (Tse et al., Reference Tse, Hong, Wang and Cunningham-Williams2012; Pilver et al., Reference Pilver, Libby, Hoff and Potenza2013; Sauvaget et al., Reference Sauvaget, Jiménez-Murcia, Fernández-Aranda, Fagundo, Moragas, Wolz, Veciana De Las Heras, Granero, del Pino-Gutiérrez, Baño, Real, Aymamí, Grall-Bronnec and Menchón2015; Assanangkornchai et al., Reference Assanangkornchai, McNeil, Tantirangsee and Kittirattanapaiboon2016; Nicholson et al., Reference Nicholson, Mackenzie, Afifi, Keough and Sareen2019). The role of these harmful effects in the GD process (onset and progression) is not clear in elderly people. On the one hand, it has been hypothesised that problematic gambling may represent a coping strategy to manage age-related distress (such as anxiety and depression caused by retirement) (Parke et al., Reference Parke, Griffiths, Pattinson and Keatley2018). It has also been suggested that psychopathological disorders could indicate progression of the problematic gambling (van der Maas et al., Reference van der Maas, Mann, McCready, Matheson, Turner, Hamilton, Schrans and Ialomiteanu2017). Whatever the case, the causes of harm related to the gambling activity are multifactorial, reflecting an interaction of individual, social and environmental processes (Wardle et al., Reference Wardle, Reith, Langham and Rogers2019). This harm increases as the risk of problem gambling increases, and it can be experienced by elderly people on a spectrum that extends from minor negative effects to crisis point. Unfortunately, it has been observed that ageing adults with severe affectation could only perceive and recognise these difficulties when the more adverse consequences have already occurred (Bischof et al., Reference Bischof, Meyer, Bischof, Guertler, Kastirke, John and Rumpf2014). Since the first step towards developing effective harm prevention plans lies in identifying the nature and scale of the construct, research studies are needed to gain a broader understanding of gambling habits in elderly people and the determinants of the adverse impacts.
Objectives
The increasing incidence of problematic and disordered gambling among elderly people highlights the need to prioritise studies to identify the specific gambling profiles in this population, a prior requirement for designing evidence-based prevention and education programmes. The objectives of this work are: (a) to assess the patterns of gambling in elderly people recruited from the general population; (b) to estimate the prevalence of the gambling severity (no risk, problematic gambling and GD) in this developmental stage; and (c) to identify what variables were related to the gambling severity, considering as potential predictors the socio-demographic profile (sex, age, immigration status, civil status, education, employment status and income), total number of lifetime life events, substance use (tobacco, alcohol and other illegal drugs) and psychopathological state. Based on the empirical evidence available, we hypothesised that non-strategic games will be the most preferred in the sample, that prevalence of problematic or disordered gambling will be around 1–10 per cent and that higher gambling severity will be related to worse psychopathological state.
Methods
Participants
The data analysed in this study pertained to a global wider research project carried out at the Pathological Gambling Outpatient Unit of University Hospital of Bellvitge, focusing on the analysis of gambling habits at older ages. This work analysed the control group of this global project, and it was recruited at the Podiatry and Dentistry Clinics on the Bellvitge University Hospital campus, between November 2016 and February 2018. This setting was selected for recruiting the controls to guarantee equivalent origin between the cases and the control groups. Since the Podiatry and Dentistry Clinics attend to individuals from the community (without a specific disorder), the sample analysed in this work is labelled ‘community sample’ or ‘population-based sample’. Inclusion criteria were age of 50 or over and adequate cognitive capacity to complete the study's self-report measures.
The sample included N = 361 participants recruited from the general population in the age range 50–90: 226 women (62.6%) and 135 men (37.4%). Many participants were born in Spain (95.3%), with primary or lower education levels (85.6%), were retired (98.1%) and did not require social aids (93.9%). Civil status was distributed as follows: 16 participants were single (4.4%), 223 were married or lived with a stable partner (61.8%), 12 were divorced or separated (3.3%) and 110 were widowed (30.5%). Table S1 in the online supplementary material includes the complete descriptive for the study sample, including all the variables analysed in this research.
Instruments
Diagnostic Questionnaire for Pathological Gambling (according to DSM criteria) (Stinchfield, Reference Stinchfield2003)
This diagnostic questionnaire allows the presence of GD to be assessed through 19 items based on the DSM taxonomy (for the DSM-IV-TR, American Psychiatric Association, 2010; for the DSM-5 versions, American Psychiatric Association, 2013). The Spanish adaptation of the scale achieved good psychometric properties (α = 0.81 calculated for the general population and α = 0.77 for clinical sample) (Jiménez-Murcia et al., Reference Jiménez-Murcia, Stinchfield, Álvarez-Moya, Jaurrieta, Bueno, Granero, Aymamí, Gómez-Peña, Martínez-Giménez, Fernández-Aranda and Vallejo2009). In this study, the total number of DSM-5 criteria for GD was analysed, as well as the classification of the GD based on the gambling activity (GD absent (no criteria), problematic gambling (one to three criteria), low GD (four or five criteria), moderate GD (six or seven criteria) and severe GD (eight or nine criteria)). Internal consistency for this scale in the sample of the study was adequate (α = 0.71).
South Oaks Gambling Severity Screen (SOGS) (Lesieur and Blume, Reference Lesieur and Blume1987, Reference Lesieur and Blume1993)
This self-report questionnaire was designed to screen GD-related problems with 20 items. The SOGS total score generated as the sum of the items is usually used as a measure of the GD severity (this dimensional measure is in the range 0–20, with higher scores indicating higher impairing gambling). The questionnaire can also be used in a categorical manner for screening for the presence of possible problem gambling (0: non-problematic gambling; 1–4: potential problematic gambling, 5 or more: probable pathological gambling). The Spanish validation of this questionnaire showed adequate psychometric properties (test–retest reliability R = 0.98, internal consistency α = 0.94, convergent validity R = 0.92) (Echeburúa et al., Reference Echeburúa, Báez, Fernández and Páez1994). Internal consistency for this scale has obtained good internal consistency in the sample of the study (α = 0.84).
Symptom Checklist – Revised (SCL-90-R) (Derogatis, Reference Derogatis1994)
This self-report tool was designed as a measure of the global psychological state, including 90 items (coded in an ordered scale: 0 = not at all, 1 = a little bit, 2 = moderately, 3 = quite a bit and 4 = extremely) structured in nine primary dimensions (somatisation, obsessive-compulsive, interpersonal sensitivity, depression, anxiety, hostility, phobic anxiety, paranoid ideation and psychoticism) and three global indices (global index of severity (GSI), positive index of discomfort (PSDI) and a total of positive symptoms (PST)). The raw scores for the primary dimensions are obtained as the mean of the items retained in each factor (the range for the scores is 0–4, and higher values indicate worse psychological state). The GSI and the PSDI global scores are also in the range 0–4 (higher values indicate greater severity and distress) and the PST is in the range 0–90 (the higher the score the greater the number of psychopathological symptoms). The Spanish version of this scale obtained good psychometric indices (mean α = 0.75) (Gonzalez De Rivera et al., Reference Gonzalez De Rivera, Derogatis, De las Cuevas, Gracia Marco, Rodríguez-Pulido, Henry-Benitez and Monterrey1989). Internal consistency in the sample of this study was also in the good (α = 0.72 for the hostility scale) to excellent (α = 0.95 for the global indexes) range.
Life events
A self-report questionnaire was developed for this study, focused on identifying potential lifetime exposure to traumatic events (including life-threatening accidents, physical/sexual abuse, death of close relatives, physical assault, separation/divorce, major financial problems, serious illness, etc.). Respondents are asked to report whether each event occurred (yes or no), the number of times it occurred, age at time of the event and affectation. The total number of cumulated life events was used in this work. Internal consistency in the sample of this study was good (α = 0.74).
Other clinical and socio-demographic variables
A semi-structured clinical interview with the participant measured all additional data, which included socio-demographic measures (such as sex, education level, civil status and employment status), gambling-related variables (age of onset of the gambling problem, duration of the gambling problem, bets per gambling-episode and accumulated debts due to gambling behaviour), and the social position index according to the Hollingshead's algorithm (which provides a global measurement based on the participants’ education level and profession; Hollingshead, Reference Hollingshead2011).
Procedure
The study was approved by the Ethics Committee of the Research Team (Hospital of Bellvitge, in Barcelona, centre of origin of the data). The clinics at the Podiatry and Dentistry unit informed their patients about the research and invited them to participate. Then, psychologists and psychiatrists with extensive experience in GD collected the semi-structured clinical interview information, and they also helped the participants to complete the self-report tools with the aim of guaranteeing that all the items were answered and no data was missing due to lack of understanding. The assessment took place in a single session lasting about 45 minutes, in the waiting rooms of the Podiatry and Dentistry clinics (located inside the hospital grounds) and without the presence of other people apart from the participant and the clinician. There was no financial or other compensation for being part of the study sample.
Regarding the order for answering questionnaires measuring GD profiles, the Diagnostic Questionnaire for Pathological Gambling was completed first with the help of the clinicians. This is diagnostic tool totally matched to the DSM criteria. The SOGS was completed next by the participants. This is a screening tool assessing signs of gambling and the consequences of gambling behaviours, and it was used as a measure of the GD severity. The SOGS is not matched to the DSM criteria for GD, and it covers cognitive, emotional and other behaviours related to problem gambling, such as lying about gambling activity, losses and debts, taking time off work, arguments with family or close friends, feeling guilty, borrowing money to gamble and performing illegal acts to finance gambling. The items examining the consequences of gambling in the SOGS are considerably more numerous than the item specifically measuring gambling behaviour.
Statistical analysis
Statistical analysis was carried out with Stata 16 for Windows (StataCorp, 2019). The comparison between the categorical variables between the groups was done with chi-square procedures (χ2) and between the quantitative variables with a t-test. The estimation of the effect size for the mean differences in this study was based on the standardised Cohen's d coefficient, considering poor–low effect size for |d| > 0.20, moderate–medium for |d| > 0.5 and large–high for |d| > 0.80 (Kelley and Preacher, Reference Kelley and Preacher2012). For categorical measures, Cohen's h was obtained as a measure of the effect size, based on the difference of the arcsine transformation (2 × arcsin × √p) of the proportions estimated in each group (Cohen, Reference Cohen1988). In addition, Type-I error due to the multiple statistical tests was controlled with the Finner's method (a familywise error rate stepwise procedure which offers a more powerful test than the classical Bonferroni correction) (Finner, Reference Finner1993).
Results
Gambling profile in the sample
For the total sample (Table S1 in the online supplementary material), the gambling activity which achieved highest prevalence in the sample was lotteries (60.4%), followed by pools (13.9%) and bingo (11.9%). The lowest prevalence was for video games (0%), gambling rooms (0.3%), sports bets (0.3%), horse-racing bets (0.8%), competition games (0.8%), casino (1.1%), bets on the internet (1.1%), stock market (1.4%), slot machines (3.0%) and cards with money (3.3%). Regarding gambling type, 35.5 per cent of the participants indicated no gambling activities, 46.0 per cent only non-strategic forms of gambling, 2.2 per cent only strategic games, and 16.3 per cent both non-strategic and strategic gambling. The mean age of onset of the gambling activities was 37.6 years of age (standard deviation (SD) = 16.0) and the duration of the gambling behaviours was 37.0 years (SD = 16.5). Most common was reporting no gambling activities, or only one preferred gambling activity (the mean number of games was 1.1, SD = 1.1). Only one participant indicated cumulative debts due to gambling activities in the past.
Within the group of participants with gambling-related problems (N = 34, with at least one DSM-5 criteria for GD), lotteries was also the most preferred gambling activity (N = 28, 82.4%), followed by bingo (N = 14, 41.2%) and betting-pools (N = 13, 38.2%). The mean age of onset of the gambling activities in this group was 36.0 years (SD = 14.5) and the mean duration of the gambling behaviours was 38.7 years (SD = 14.2). The number of gambling activities ranged between one and five, with two games being the most common (N = 16, 47.1%).
GD prevalence
Regarding prevalence estimates in the complete sample (N = 361), most participants were in the absent problem gambling group (participants with no DSM-5 criteria: N = 327, 90.6%, 95% confidence interval (95% CI) = 87.6–93.6), while the problematic gambling group included N = 29 participants with one to three DSM-5 criteria (prevalence = 8.0%; 95% CI = 5.2–10.8), and N = 5 participants achieved DSM-5 criteria for GD (prevalence = 1.4%; 95% CI = 0.2–2.6).
Table 1 contains the prevalence estimates and comparison by sex and age group (two age groups were defined, based on the median – 50th percentile – in the sample). Differences between men and women were found (χ2 = 8.31, p = 0.040): men obtained a higher prevalence of participants in the problematic group compared to women (11.1% versus 6.2%), but a lower prevalence of individuals who met criteria for GD (GD-moderate was met for 1.8% of females while 0.7% of males were in the GD-low group). No differences in the severe gambling group were found comparing the two age groups (χ2 = 1.07, p = 0.784).
Table 1. Prevalence of the gambling disorder (GD) severity group in the study

Notes: CI: confidence interval. 1. Age groups are generated based on the median (50th percentile) in the sample.
Comparison of gambling profile by sex and age
Table 2 includes the comparison of the gambling profile between men and women. As a whole, a higher percentage of men reported gambling activities in their different forms (the proportion comparisons for lotteries, pools, slot machines, cards and stock market forms achieved statistical differences). A higher percentage of women reported no gambling activity (39.8% versus 28.1%), while a higher percentage of men reported both non-strategic and strategic gambling forms (27.4% versus 9.7%). The mean age of onset of the gambling activities was younger for men (33.9 years versus 40.3 years), while the bets per gambling-episode and the number of total games was higher in the male group. Regarding the comparison based on age group in Table 2, differences were found only in the age of onset of gambling (older age in elderly participants) and the duration of the gambling activities (longer duration in the elderly group).
Table 2. Comparison of the profile of gambling in the old-age general population based on sex and age
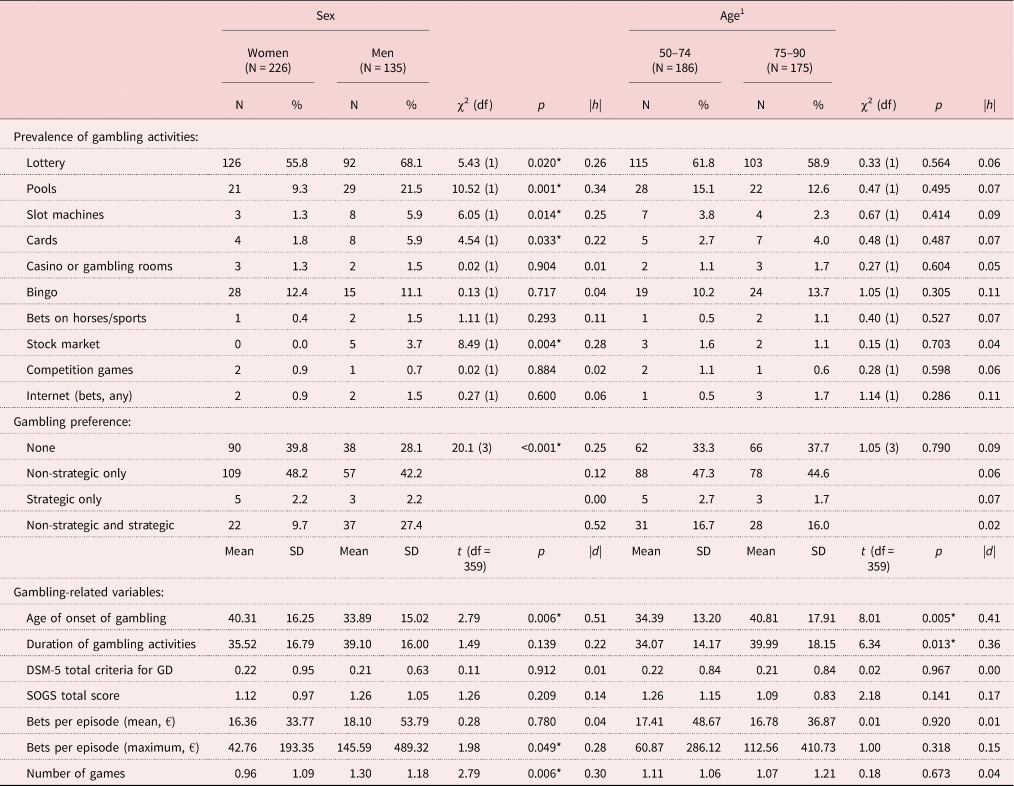
Notes: df: degrees of freedom. SD: standard deviation. DSM-5: Diagnostic and Statistical Manual of Mental Disorders, 5th Edn. GD: gambling disorder. SOGS: South Oaks Gambling Severity Screen. 1. Age groups are generated based on the median (50th percentile) in the sample. Effect size: |d| or |h| < 0.20 lower; |d| or |h| > 0.20 mild–moderate; |d| or |h| > 0.50 moderate–mild; |d| or |h |> 0.80 large–high.
Significance level: * Significant comparison.
Variables related to gambling severity
Table 3 includes the comparison of the socio-demographic and clinical profile between participants in the absent problem gambling group (those who reported no DSM-5 criteria for GD) and in the problematic or disorder gambling group (participants with one to nine DSM-5 criteria for GD). This study has grouped participants with at least one DSM-5 criterion for GD because the number of individuals who met criteria for GD was too few to allow statistical comparisons (N = 5). The results of the proportion and mean comparisons in this table suggest that the risk factors for gambling-related problems in the study are not having been born in Spain and a higher number of lifetime life events. In addition, the group with any DSM-5 criteria for GD registered a higher prevalence of tobacco and alcohol use-abuse and worse psychopathological state (higher means in the SCL-90-R scales). Chronological age was in the range 50–85 among individuals with and without gambling-related problems, and no differences by age were obtained when comparing both groups (p = 0.758).
Table 3. Comparison of the profiles in the old-age general population based on the gambling disorder severity group
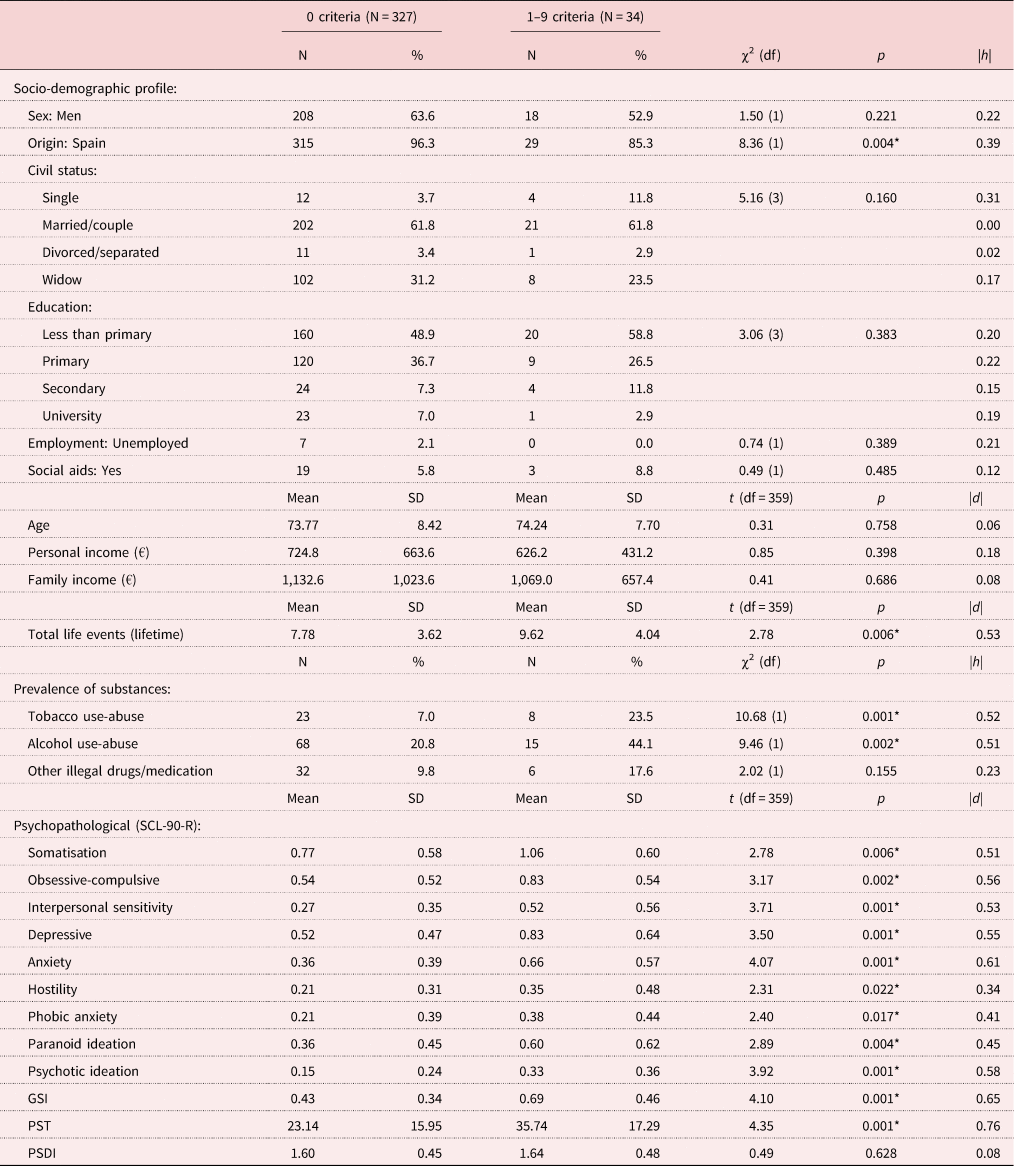
Notes: df: degrees of freedom. SD: standard deviation. SCL-90-R: Symptom Checklist – Revised. GSI: global index of severity. PSDI: positive index of discomfort. PST: total of positive symptoms. Effect size: |d| or |h| < 0.20 lower; |d| or |h| > 0.20 mild–moderate; |d| or |h| > 0.50 moderate–mild; |d| or |h |> 0.80 large–high.
Significance level: * Significant comparison.
Discussion
This population-based study examined gambling activity among elderly people, in a population-based sample composed of individuals of a large range of ages (between 50 and 90 years), and explored the socio-demographic and clinical variables related to the most severe gambling profile. The prevalence of individuals who reported gambling activity was 65.5 per cent, with non-strategic games (mainly lottery tickets) being the most preferred form. The prevalence of GD was 1.4 per cent, and problematic gambling was reported by 8.0 per cent of the participants. The most severe gambling was related to immigration, stressful life events, worse psychopathological state and substance use.
The high prevalence of participants who reported gambling behaviour (around 72 per cent of men and 60 per cent of women) is consistent with previous research studies, which show that gambling is a common leisure activity among elderly people in developed countries (Alberghetti and Collins, Reference Alberghetti and Collins2015; Pattinson and Parke, Reference Pattinson and Parke2016; Subramaniam et al., Reference Subramaniam, Satghare, Vaingankar, Picco, Browning, Chong and Thomas2017b). The higher preference of non-strategic gambling was also an expected result, confirming that elderly people usually select simple games (Black et al., Reference Black, Coryell, McCormick, Shaw and Allen2017; Granero et al., 2020; Jiménez-Murcia et al., Reference Jiménez-Murcia, Granero, Fernández-Aranda and Menchón2020). Specifically, lottery tickets were the most usual game in the study for both men and women (with participation rates of 68.1 and 55.8%, respectively). Many older people like to dream of winning the lottery, and going to buy the tickets can be perceived as a great opportunity for socialising and a nice break from routine life (Granero et al., Reference Granero, León-Vargas, Martín-Romera, Fernández-Aranda, Mena-Moreno, del Pino-Gutiérrez, Codina, Gómez-Peña, Moragas, Aymamí, Mestre-Bach, Agüera, Vintró-Alcaraz, Lozano-Madrid, Casalé-Salayet, Menchón and Jiménez-Murcia2020c). While the vast majority of participants in the study gambled without problems, the high proportion of people participating in lotteries (as well as in other gambling subtypes) (Luce et al., Reference Luce, Kairouz, Nadeau and Monson2016; Godinho et al., Reference Godinho, Kushnir, Hodgins, Hendershot and Cunningham2018) should be taken very seriously. Firstly, the signs of a gambling problem may be subtle among elderly people, and in some cases other family members or close friends do not realise the scope of the problem until they help them pay bills or balance a chequebook. Some studies have even observed that what elderly people consider to be gambling varied compared to younger adults. For example, among some older adults, lotteries or bingo are not considered forms of gambling, but rather as social or light-hearted activities, and sports betting or pools are perceived as hobbies because of their love of sports or football (Tira and Jackson, Reference Tira and Jackson2015). In Spain, there are many different forms of lotteries, and this is a highly prevalent activity among the general population (Dirección-General-Ordenación-Juego, 2017). Its simplicity, wide publicity and general social acceptability can contribute towards reinforcing the image of lotteries as a safe activity among elderly people, who may even believe that this game is an easy way to achieve a better economic position (Lutter et al., Reference Lutter, Tisch and Beckert2018). These particular conceptions, associated with the lifestyle of many elderly people (availability of time and financial resources – Social Security income or pensions) can contribute towards intensifying the gambling frequency and therefore their vulnerability. In addition, primary care physicians and geriatricians are the professionals closest to older people who usually need to monitor their health and the medication they are taking for age-related illnesses. It would be advisable for these health specialists to explore the existence of gambling problems during their routine visits, in order to identify potential problems with gambling activity and be able to refer them to the treatment facilities, as quickly as possible, before the consequences and damage caused by this behaviour increases. Often, older people are alone, have less contact with their sons and daughters (who are working and have their own families at the time), have more limited income, and may feel embarrassed about their debts and financial problems, so they may be reluctant to seek help. Therefore, it is important that the doctors who usually monitor their medication and health status explore this issue. This scenario requires appropriate evidence-based programmes, such as preventive services which include education and increased public awareness of problematic behaviours related to any form of gambling. The objective should not be to eliminate gambling among older adults, but to improve knowledge of responsible gambling to reduce harm.
Regarding the prevalence of GD in the study, 1.4 per cent of the participants met DSM-5 criteria for disordered gambling, while problematic gambling was reported by 8%. The prevalence of GD was also higher for women compared to men (1.8% versus 0.7%), but the prevalence of problematic gambling was higher for males compared to females (11.1% versus 6.2%). These results confirm the prevalence estimated in the epidemiological area, which reports that GD can occur at any age and in both sexes during senescence (Black et al., Reference Black, Shaw, Coryell, Crowe, McCormick and Allen2015). Beyond the estimate of the prevalence of the GD profile among elderly people, our results are particularly useful for identifying early indicators of problematic and disordered gambling. Specifically, being an immigrant and having a higher number of stressful life events was significantly associated with the most severe gambling activity. These are two common risk factors systematically reported in the bibliography across ages (Subramaniam et al., Reference Subramaniam, Wang, Soh, Vaingankar, Chong, Browning and Thomas2015; Smith et al., Reference Smith, Hategan and Bourgeois2017). In fact, immigration constitutes a multiple-stressor situation that involves cognitive appraisals and coping efforts, and it has been associated with greater psychological distress and depressive symptoms (Lanzara et al., Reference Lanzara, Scipioni and Conti2018). The occurrence of lifespan stressful life events has been identified as a powerful contributor to the onset of gambling activity, but also to the severity levels and even to the changes in gambling habits over time (Luce et al., Reference Luce, Kairouz, Nadeau and Monson2016; Godinho et al., Reference Godinho, Kushnir, Hodgins, Hendershot and Cunningham2018). Experiencing these events has achieved predictive capacity in both the short and long term: stressful episodes in childhood, adolescence or early adulthood have been connected with increases in the frequency and severity of gambling behaviour in later life (Storr et al., Reference Storr, Lee, Derevensky, Ialongo and Martins2012). Since older individuals can suffer the effects of cumulative lifespan stressful life events, the presence of new ageing-related stressors (isolation, insecurity, financial difficulties and unhealthy conditions) makes them more vulnerable to increasing and/or modifying their gambling activity (Luce et al., Reference Luce, Kairouz, Nadeau and Monson2016; Godinho et al., Reference Godinho, Kushnir, Hodgins, Hendershot and Cunningham2018). Betting on games is usually viewed by elderly people as an attractive coping strategy for persistent stress (Guillou Landreat et al., Reference Guillou Landreat, Cholet, Grall Bronnec, Lalande and Le Reste2019), with the eventual consequence of increases in impairment and harm.
Differences in the gambling profile comparing sexes showed among men higher prevalences for different gambling activities, higher preference for mixed games (non-strategic and strategic), younger age of onset and higher bets per gambling-episode. These results are consistent with epidemiological and risk factor studies in elderly people, which have obtained higher odds of gambling, younger onset and more severity in males (Pilver et al., Reference Pilver, Libby, Hoff and Potenza2013; Sauvaget et al., Reference Sauvaget, Jiménez-Murcia, Fernández-Aranda, Fagundo, Moragas, Wolz, Veciana De Las Heras, Granero, del Pino-Gutiérrez, Baño, Real, Aymamí, Grall-Bronnec and Menchón2015; Subramaniam et al., Reference Subramaniam, Wang, Soh, Vaingankar, Chong, Browning and Thomas2015). Comparison of the gambling profile by age group showed differences in the age of onset and the duration of the gambling activities (later onset and longer evolution in the 75–90 years group). Age of onset and duration of the illness are two relevant but relatively understudied factors in GD. It is well known that this disorder may have its onset in a wide range of ages (from adolescence to old age), and individuals with gambling-related problems may seek treatment at different moments in the GD course (Blaszczynski and Nower, Reference Blaszczynski and Nower2002). Some factors could explain the longer duration in the older age group, such as the reduced progression speed with age (Medeiros et al., Reference Medeiros, Redden, Chamberlain and Grant2017) or the usual decrease in the impulsivity levels with ageing (Hamilton et al., Reference Hamilton, Littlefield, Anastasio, Cunningham, Fink, Wing, Mathias, Lane, Schütz, Swann, Lejuez, Clark, Moeller and Potenza2015; MacKillop et al., Reference MacKillop, Weafer, Gray, Oshri, Palmer and de Wit2016). Current meta-analyses have linked GD to dysfunctions of cognitive domains regulating impulsive behaviour, as well as deficits in GD across all evaluable domains of impulsivity (van Timmeren et al., Reference van Timmeren, Daams, van Holst and Goudriaan2018; Ioannidis et al., Reference Ioannidis, Hook, Wickham, Grant and Chamberlain2019). Decreases in impulsivity levels at older ages could contribute to lower GD severity and lower impact in non-gambling-related areas, and therefore reduce the responsiveness to treatment.
The correlation between the more problematic gambling activity and worse psychopathological state and the higher prevalence of substance use is particularly alarming. As has been systematically reported across age groups, at-risk gambling is usually accompanied by the presence of co-occurring disorders, including mood-anxiety problems and substance use (Pilver et al., Reference Pilver, Libby, Hoff and Potenza2013; Assanangkornchai et al., Reference Assanangkornchai, McNeil, Tantirangsee and Kittirattanapaiboon2016; Nicholson et al., Reference Nicholson, Mackenzie, Afifi, Keough and Sareen2019). This situation is especially problematic among elderly people, since it has been observed that older adults with a GD often experience higher levels of psychological distress and/or comorbidity compared with younger adults (van der Maas et al., Reference van der Maas, Mann, McCready, Matheson, Turner, Hamilton, Schrans and Ialomiteanu2017; Parke et al., Reference Parke, Griffiths, Pattinson and Keatley2018). Unlike younger gamblers, who usually report looking for action and excitement as a primary motivation for gambling (Armstrong et al., Reference Armstrong, Rockloff and Browne2020), many older people use gambling as an escape, and seniors with the greatest need for that escape are those with previous physical and/or psychological disease (who are precisely the most vulnerable to developing gambling problems) (Tira et al., Reference Tira, Jackson and Tomnay2014; Medeiros et al., Reference Medeiros, Leppink, Yaemi, Mariani, Tavares and Grant2015; Subramaniam et al., Reference Subramaniam, Wang, Soh, Vaingankar, Chong, Browning and Thomas2015; Pattinson and Parke, Reference Pattinson and Parke2016). People who have recently lost their partner, or even those who have retired from work, are at risk of suffering from anxiety or depression, and they can find an opportunity to cope with distress in gambling and in the use of comorbid substances (Botterill et al., Reference Botterill, Gill, McLaren and Gomez2016). It should be kept in mind that, as a rule, older adults want to prevent the aggravation of their functionality and health (McGilton et al., Reference McGilton, Vellani, Yeung, Chishtie, Commisso, Ploeg, Andrew, Ayala, Gray, Morgan, Chow, Parrott, Stephens, Hale, Keatings, Walker, Wodchis, Dubé, McElhaney and Puts2018), and therefore if they are helped to recognise the potential risk associated with the gambling activity, they can attempt to cut back. A new diagnosis often motivates elderly individuals to modify their daily routines and health-care behaviours, which usually takes time and effort and becomes quite difficult for some subjects (Morales-Asencio et al., Reference Morales-Asencio, Martin-Santos, Kaknani, Morilla-Herrera, Cuevas Fernandez-Gallego, Garcia-Mayor, León-Campos and Morales-Gil2016). Frequently some care-givers take on the role of directing this change process, but they may have reservations about how to handle these situations, resulting in a new source of stress between the elderly adult and the care-giver. Ultimately, care-givers and older adults usually disagree on how to remain healthy, and on the limits of individual independence (Naganathan et al., Reference Naganathan, Kuluski, Gill, Jaakkimainen, Upshur and Wodchis2016). Identifying the comorbid correlates of the most severe forms of gambling in elderly people is a first step towards developing prevention and treatment recommendations, useful for all the members involved in the elderly adult's wellbeing (the participant themselves, care-givers and clinicians). Future research should explore the underlying mechanisms of the harm caused by gambling practices to prevent and minimise the negative consequences for individuals, care-givers and their contexts.
Limitations and strengths
This work should be interpreted considering several limitations. First, only data recruited in a population-based sample was analysed, so it is not clear how our results are generalisable to other treatment-seeking and clinical samples. Second, analyses were performed on cross-sectional data, which provide measures of association but do not allow causal relationships to be confirmed. Third, the non-random sampling procedure limits the capacity to generalise, since there is no guarantee of potential biases regarding coverage of the different levels of gambling risk in the original population of elderly people. Fourth, the lack of physical measures related to the ageing process (such as the use of medical services or medication, poorer overall health status and/or higher chronic conditions) hinders their distribution into the empirical clusters and the estimate of their potential relation with gambling problems/severity. Finally, this study was carried out with a quantitative methodology (future qualitative research should provide additional evidence about attitudes and opinions regarding gambling contents).
But despite this set of limitations, this work also has several strengths. First, a relatively large set of measures has been analysed to provide a comprehensive picture of the gambling activity in older age. Besides providing the profile of the gambling activity, several indicators have been used to measure the clinical severity related to the gambling behaviour, such as the number of DSM-5 criteria, the bets per gambling-episode, the cumulative debts due to the gambling behaviour and even other psychopathological comorbid correlates. Second, the large sample size analysed in the study, including both sexes, provides high external validity to our research.
Conclusion
Gambling is a commonplace social activity across cultures, which can be a harmless recreational activity contributing to subjective wellbeing among elderly people. For older adults who have increased leisure time and/or for those individuals whose health status may limit participation in activities that they previously enjoyed, responsible gambling may provide an alternative for entertainment. However, some elderly individuals are especially vulnerable to gambling-related problems due to multiple factors, including declining health, loneliness, personal and role losses, social isolation and lower incomes. This high-risk group can develop GD, with the consequences of increased impaired functioning and reduced quality of life.
There is a rising interest in the study of gambling behaviour in elderly people, but the cumulated evidence available so far should be interpreted with caution. Data evaluating frequency, motivations, preferences, risk factors, and evolution of non-problematic and problematic gambling among older adults are relatively scarce (compared to other age groups), largely because of the low sample sizes for this age group in the research area. This study provides new empirical knowledge of gambling habits in a large population-based sample of elderly individuals. Our results can contribute to the development of more person-centred approaches for intervening in the field of gambling among seniors. Studies focused on the issues related to the access to treatments and therapy efficacy for GD outline that meeting the specific needs of individuals contributes to an increase in the number of people who initiate the treatments, continue the therapy and achieve good outcomes (Dabrowska et al., Reference Dabrowska, Moskalewicz and Wieczorek2017). Efforts to respond better to the treatment needs of individuals with impairing gambling behaviour and improve the quality of therapies should take into account the heterogeneity component of the gambling problem, and the specificity of each subject.
Results of this study also contribute to the intervention areas. It is essential that the diverse clinical settings explore and screen the presence of early symptoms and negative consequences of the gambling activity among older-age individuals (including primary care settings), with the aim of incorporating strategies to reduce these potential adverse impacts and prevent the progression to problematic and/or disordered gambling. The adequate identification of the multiple processes and correlates of GD is crucial for planning effective treatment tools, since interventions should be addressed to alleviating gambling-related impairing behaviours as well as other concurrent psychiatric conditions. GD is a highly disabling mental circumstance which carries a great deal of stigma, and its developmental course is greatly worsened within highly vulnerable populations (since old-age individuals can be particularly exposed to age-related brain dysfunctions). Therefore, evidence-based integrative intervention plans should be specifically developed for elderly people, addressed to the full range of physical and emotional problems, as well as the environmental influences that affect the subjects’ health. Healing-oriented holistic programmes should include strategies to increase self-control and reduce impulsively (such as training in working memory and response inhibition), to improve emotional regulation, to prevent or reduce chronic stress, and to increase social skills. Medication should also be required in those cases with brain chemical imbalances.
Supplementary material
The supplementary material for this article can be found at https://doi.org/10.1017/S0144686X21000258.
Data
Data cannot be shared publicly due to being part of a public hospital clinical database. Data are available from the Hospital Universitari de Bellvitge – Institutional Data Access/Ethics Committee (IDIBELL; otri@idibell.cat) for researchers who meet the criteria for access to confidential data.
Acknowledgement
We thank the CERCA Programme/Generalitat de Catalunya for institutional support.
Author contributions
Conceptualisation and design: AdP-G, RG, SJ-M. Data analysis and interpretation of data: RG, SJ-M. Funding acquisition: SJ-M, FF-A. Investigation: TM-M, GM-B, MG-P, EC, CV-A, ML-M, ZA, JS-G, GC, IB, IS, HL-G. Methodology: RG, SJ-M. Project administration: SJ-M, FF-A, JMM. Resources: AdP-G. Supervision: SJ-M. Visualisation: AdP-G, SJ-M, IG, MG-B, AS, JMM. Writing – original draft preparation: RG, SJ-M. Writing – review and editing: SJ-M, RG.
Financial support
This work was supported by the Ministerio de Economía y Competitividad (grant number PSI2015-68701-R); the Ministerio de Ciencia, Innovación y Universidades (grant number RTI2018-101837-B-100); the Delegación del Gobierno para el Plan Nacional sobre Drogas (grant numbers 2017I067, 2019I47); Instituto de Salud Carlos III (ISCIII) (grant numbers FIS PI14/00290, PI17/01167) (CIBERObn and CIBERsam are both initiatives of ISCIII); FEDER funds/European Regional Development Fund (ERDF), A Way to Build Europe; the Secretariat for Universities and Research of the Ministry of Business and Knowledge of the Government of Catalonia; and the Ministerio de Educación, Cultura y Deporte (TMM, grant number FPU16/02087; CVA, grant number FPU16/01453; MLM, grant number FPU15/02911). The funders had no role in the design of the study; in the collection, analyses or interpretation of data; in the writing of the manuscript; or in the decision to publish the results.
Conflict of interest
The authors declare no conflicts of interest.
Ethical standards
All procedures were carried in accordance with the Declaration of Helsinki. Ethical approval was obtained from the Ethics Committee of Bellvitge University Hospital (Ref: PR286/14). All the participants were informed about the study and all provided informed consent.





