Introduction
Vertigo and dizziness are common symptoms observed in clinical practice. The population census in 2016 from the Ministry of Health, Labour and Welfare of Japan reported that approximately 2.8 million people had vertigo or dizziness. Vertigo and dizziness are very common complaints among patients who are 75 years or older,Reference Neuhauser, von Brevern, Radtke, Lezius, Feldmann and Ziese1 and their prevalence has been increasing in elderly populations, which results in increasing medical costs.
Unfortunately, misdiagnosis of vertigo and dizziness is a major issue, especially in primary care.Reference Grill, Strupp, Muller and Jahn2 An accurate medical history and clarification of the patient's complaints are necessary to ensure an accurate diagnosis, an appropriate medical strategy for the treatment of vertigo and dizziness and patient satisfaction. However, this requires considerable experience and can be challenging because patient complaints are often vague. In fact, 40–80 per cent of patients are not definitively diagnosed in the long-term and do not receive adequate therapy.Reference Grill, Strupp, Muller and Jahn2 Additionally, patients with vertigo or dizziness tend to simultaneously consult physicians of different specialties such as otorhinolaryngologists, neurologists, internists or orthopaedists.Reference Grill, Strupp, Muller and Jahn2 In these cases, the patients are rarely satisfied with their diagnosis and treatment, which can lead to so-called ‘doctor shopping’. This process generates unnecessary or redundant medical examinations and causes a financial burden on the healthcare system.Reference Neuhauser, von Brevern, Radtke, Lezius, Feldmann and Ziese1–Reference Neuhauser, Radtke, von Brevern, Lezius, Feldmann and Lempert3
The aim of the present study was to identify the characteristics of patients referred to specialised neurotologists to assess differences in diagnosis between primary-care physicians and specialised neurotologists. Our end goal was to improve the diagnostic accuracy of vertigo and dizziness.
Materials and methods
The medical ethics committee of our university approved this study (certificate number: 0889). All patients provided informed consent in accordance with the Declaration of Helsinki.
Patients
A total of 217 patients who visited the vertigo and dizziness centre at our university hospital from April 2017 to November 2018 were enrolled in the present study. The chief complaint of all patients was vertigo or dizziness.
Study design
This was a retrospective study. Data collection was performed in the vertigo and dizziness centre of our university hospital. Because the Japanese government requires patients to see a primary-care doctor before visiting major hospitals, almost all patients visiting our centre had reference letters from primary-care physicians. To delineate the diagnostic procedures followed by these referring physicians, and to identify differences in diagnosis between these physicians and neurotologists in our institution, we reviewed the referral letters and clinical records from our centre. Data were collected independently by two physicians (with 3 and 10 years of experience). When the two physicians disagreed on some aspect of the collected data, a third physician (with 40 years of experience) examined the reference letters or clinical records, and then a consensus was reached with consultation among the three physicians.
Diagnostic procedures followed by the previous physicians
We used the reference letters from the previous physicians to gather data on the diagnostic procedures and final diagnosis. If the letters lacked sufficient data, we used medical questionnaires that were completed by the patients.
From the reference letters, we collected the following information: (1) the intervals during which the patients were under treatment by previous physicians; (2) the medical examinations, such as pure tone audiometry, magnetic resonance imaging (MRI) and computed tomography (CT), that were performed by previous physicians; and (3) the final diagnoses of previous physicians.
From the medical questionnaires, we collected the following information: (1) the intervals during which the patients were under treatment by previous physicians; (2) the number of clinics or hospitals that they had visited before the first visit to our centre; and (3) the medical examinations, such as pure tone audiometry, MRI and CT, that they had received before the first visit to our centre; (4) the diagnoses reached by the previous physicians; and (5) the number of visits to previous physicians.
Diagnostic procedure by neurotologists at our centre
Neurological and neurotological histories were obtained, and examinations were performed by the neurotologists at our centre. Furthermore, patients were examined using pure tone audiometry, the Schellong test, electronystagmography (ENG), the caloric test with ENG, posturography and gait analysis. Following this, patients received additional examinations, including vestibular-evoked potential tests, the video head impulse test, electrocochleography and MRI to show presence of endolymphatic hydrops.Reference Ito, Inui, Miyasaka, Shiozaki, Hasukawa and Yamanaka4 A diagnosis was reached according to the classification of vestibular disorders from the Barany SocietyReference Bisdorff, Von Brevern, Lempert and Newman-Toker5–Reference von Brevern, Bertholon, Brandt, Fife, Imai and Nuti11 and Japan Society for Equilibrium Research in 1987 and 2017 (in Japanese). In addition, orthostatic dysregulation was diagnosed according to the criteria defined by Joseph et al.,Reference Joseph, Wanono, Flamant and Vidal-Petiot12 and psychogenic dizziness was diagnosed according to the criteria by Dieterich et al.Reference Dieterich, Staab and Brandt13 and by consultation with specialised psychiatrists.
Results
Patient characteristics
Our patient population consisted of 75 men and 142 women, with ages ranging from 16–89 years (median, 64.5 years). The median number of hospitals or clinics that the patients had visited was 2, ranging from 1–20. The types of hospitals or clinics where the patients saw the previous physicians are shown in Figure 1. The reference letters were provided by otorhinolaryngologists and internists in 62.2 per cent (135 of 217) and 29.5 per cent (64 of 217) of the cases, respectively. The interval during which the patients were under treatment by previous physicians was 5 months (median), ranging from 1–400 months. In total, 32.3 per cent (70 of 217) of the patients stopped visiting their previous physicians within 1 month, and of these patients 55.7 per cent (39 of 70) consulted their previous doctor only once.

Fig. 1. The types of hospitals or clinics that patients visited to acquire the reference letters to our centre. Otorhinolaryngologists referred 62.2 per cent (135 of 217) of the patients, and internists referred 29.5 per cent (64 of 217) of the patients. The others were referred by Departments of Neurosurgery (8 of 217), Psychiatry (3 of 217), Obstetrics and Gynaecology (2 of 217), General Surgery (2 of 217) and Orthopaedics (1 of 217).
Diagnoses by the previous physicians
Table 1 shows the diagnoses of the previous physicians. In 47.0 per cent (102 of 217) of the patients, the previous physicians did not diagnose vertigo or dizziness. When confirming their diagnosis, the previous physicians performed medical examinations in 78.3 per cent (170 of 217) of the patients. The most popular examination was pure tone audiometry, performed in 71.5 per cent (123 of 217) of the patients. All pure tone audiometry tests were performed by otorhinolaryngologists. The previous physicians performed CT or MRI in 43.3 per cent (94 of 217) of the patients. Interestingly, CT or MRI was ordered by 51.9 per cent (28 of 54) of the internists, and this was the only examination used to diagnose vertigo or dizziness in the department of internal medicine.
Table 1. The diagnoses of previous physicians and neurotologists

A diagnosis could not be reached by the previous physicians for 47.0 per cent (102 of 217) of the patients. The most frequent diagnosis by the previous physicians was MD (25.8 per cent, 56 of 217). Conversely, the most frequent diagnosis by the neurotologists was BPPV (33.6 per cent, 73 of 217). BPPV = benign paroxysmal positional vertigo; MD = Ménière's disease; SD = sudden deafness; UVD = unilateral vestibular disorder; BVD = bilateral vestibular disorder; VN = vestibular neuritis; Central = central vertigo; OD = orthostatic dysregulation
Diagnosis by the neurotologists
The diagnoses by the neurotologists are also shown in Table 1. All neurotologists confirmed the diagnosis in all patients. Among the diagnoses, 33.6 per cent (73 of 217) and 27.6 per cent (60 of 217) of the patients had diagnoses of benign paroxysmal positional vertigo (BPPV) and Ménière's disease, respectively.
Comparing diagnoses of previous physicians and neurotologists
In 67.3 per cent (146 of 217) of the patients, there was a difference in diagnosis between the previous physicians and the neurotologists. Seventy-six patients were misdiagnosed by otorhinolaryngologists and 70 patients were misdiagnosed by physicians from other specialities. Among all the patients in the present study, the most frequent misdiagnosis was BPPV (24 and 26 patients by otorhinolaryngologists and physicians from other specialities, respectively). The second most frequent misdiagnosis was Ménière's disease (13 and 13 patients by otorhinolaryngologists and physicians from other specialities, respectively).
Figure 2a shows the diagnosis that was established by neurotologists of patients who were initially diagnosed with BPPV by previous physicians. BPPV was diagnosed in 66.7 per cent (24 of 36) of the patients; 16 patients were diagnosed by the otorhinolaryngologists. The most frequent misdiagnosis was Ménière's disease (4 and 1 by otorhinolaryngologists and physicians from the other specialities, respectively). Figure 2b shows the diagnosis that was established by neurotologists of patients who were initially diagnosed with Ménière's disease by previous physicians. Ménière's disease was diagnosed in 60.7 per cent (34 of 56) of the patients; all 34 patients were diagnosed by otorhinolaryngologists, and all patients diagnosed with Ménière's disease by physicians from other specialities received a misdiagnosis. The most frequent misdiagnosis was BPPV (10 and 2 by otorhinolaryngologists and physicians from other specialities, respectively). Figure 2c shows the diagnosis that was established by neurotologists for patients who were not diagnosed by previous physicians. Of those, 34.3 per cent (35 of 102) were diagnosed with BPPV, 16.7 per cent (17 of 102) with Ménière's disease and 17.6 (18 of 102) with orthostatic dysregulation.
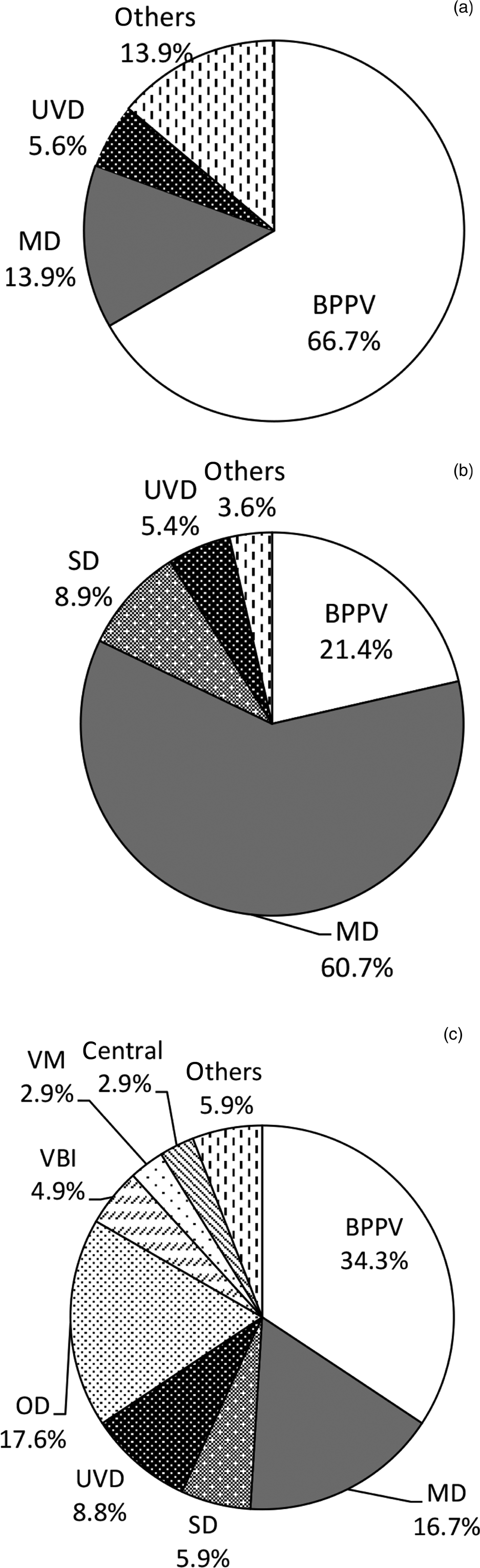
Fig. 2. Diagnosis by specialised neurotologists at our centre showing: (a) neurotologist diagnoses for patients who were diagnosed with BPPV by previous physicians, (b) neurotologist diagnoses for patients diagnosed with MD by previous physicians and (c) neurotologist diagnoses for patients who could not be diagnosed by the previous physicians. Among the patients diagnosed with BPPV by the previous physicians (a), the neurotologists diagnosed 66.7 per cent with BPPV (i.e. the same diagnosis), 13.9 per cent with Ménière's disease and 5.6 per cent with UVD. Among the patients diagnosed with Ménière's disease by the previous physicians (b), the neurotologists diagnosed 60.7 per cent with Ménière's disease (i.e. the same diagnosis), 21.4 per cent with BPPV, 8.9 per cent with sudden deafness (SD) and 5.4 per cent with UVD. Among the patients who could not be diagnosed by the previous doctors (c), the neurotologists diagnosed 34.3 per cent with BPPV, 16.7 per cent with Ménière's disease and 17.6 with OD. UVD = unilateral vestibular disorder; MD = Ménière's disease; BPPV, benign paroxysmal positional vertigo; SD = sudden deafness; VM = vestibular migraine; central = central vertigo; VBI = vertebrobasilar insufficiency; OD = orthostatic dysregulation
Discussion
In the present study, we examined differences in the diagnosis of patients with vertigo or dizziness between previous physicians and neurotologists. There was a difference in the final diagnosis in 67.3 per cent of the cases with reference letters to our centre. In addition, 47.0 per cent of the previous physicians could not establish a definitive diagnosis and only noted the symptoms as vertigo or dizziness on the reference letters to our centre. Geser et al. showed that in 70 per cent of the reference letters to the specialised neurotological centre in Switzerland, a clear diagnosis was not established and only ‘unclear dizziness’ was mentioned; the primary-care physicians often misdiagnosed patients.Reference Geser and Straumann14 The results in the present study are consistent with those of Geser et al.Reference Geser and Straumann14 In addition, our results were consistent with the results of a study by Grill et al., which reported that 40–80 per cent of patients had long-term vertigo or dizziness without a correct diagnosis and adequate treatment in Germany.Reference Grill, Strupp, Muller and Jahn2 These results suggest that misdiagnoses by primary-care physicians are a significant problem. The criteria for a vertigo or dizziness diagnosis require precise history taking;Reference Bisdorff, Von Brevern, Lempert and Newman-Toker5–Reference von Brevern, Bertholon, Brandt, Fife, Imai and Nuti11 therefore, we argue that physicians should receive appropriate training and accumulate sufficient experience to collect adequate information to reach an accurate diagnosis.
Patients may describe their symptoms in an ambiguous manner.Reference Blakley and Goebel15 In our prefecture, because primary doctors are extremely busy, otorhinolaryngologists see approximately 20 patients per hour. Taken together, these factors highlight the challenges for primary physicians attempting to diagnose vertigo or dizziness. Conversely, the diagnostic procedures for vertigo or dizziness do not require special examination equipment, indicating that primary-care physicians can reach an accurate diagnosis if they can obtain an accurate patient history. Approximately 45 per cent of patients with vertigo or dizziness are treated by primary-care physicians;Reference Sloane16 however, the diagnoses differ from the final diagnosis of specialised neurotologists. This shows the importance of neurotological skills in primary-care physicians, which should be improved, or the development of artificial intelligence systems that could support the diagnostic procedure.
Feil et al. reported that an accurate diagnosis can be reached using an iPad®-based medical device.Reference Feil, Feuerecker, Goldschagg, Strobl, Brandt and von Muller17 When physicians input patient symptoms and the results of physical examinations into the iPad application, the application reports the appropriate examination and diagnostic procedure required. This system mimics the physicians’ thinking and supports the physicians’ diagnostic reasoning in an effortless and congenial way. Using this device, physicians can reach an accurate diagnosis: the accuracy of diagnosing BPPV and Ménière's disease was 92.6 per cent and 94.1 per cent, respectively, using this device. Material to assist in the diagnosis, such as diagnostic computer programs, must be developed to ensure that primary-care physicians can reach an accurate diagnosis. If a correct diagnosis is reached, specific effective treatment depending on the cause is often available with drugs or surgery and physiotherapy or psychotherapy. For example, most patients with BPPV can be treated with an appropriate repositioning manoeuvre for the affected semi-circular canal, and those with Ménière's disease can be treated with diuretic drugs. Thus, the development of methods to assist in the diagnosis is essential for the treatment and improvement of the quality of life for patients with vertigo or dizziness.
The sensation of vertigo or dizziness is a burden and affects quality of life. Eighty per cent of patients with vertigo or dizziness require sick leave or a medical consultation.Reference Neuhauser18 In addition, Murdin and Schilder showed that 27 per cent of patients changed jobs, 21 per cent stopped working, 50 per cent reported reduced efficiency at work, 57 per cent experienced disruptions to their social life, 35 per cent experienced family difficulties, and 50 per cent reported travel difficulties with vertigo or dizziness.Reference Murdin and Schilder19 An accurate diagnosis and adequate treatment enables patients to return to their normal daily life and contribute to society.
The present study had some limitations. First, it was conducted in a university hospital. Almost all patients who visited our centre had intractable vertigo or dizziness, and previous physicians could not provide satisfactory treatments. In addition, patients gather information about specialists through the internet or television programmes quite easily. In the present study, some patients only visited the previous doctor to obtain the reference letter to our centre, which may have affected the number of diagnoses of unclear dizziness.
In the present study, there was a great difference (approximately 70 per cent of the reference letters) between primary-care physicians and neurotologists. Neurotologists have the responsibility to reduce this difference. Neurotologists should educate primary-care doctors regarding diagnostic procedure and criteria to allow the latter to improve their skills and diagnostic accuracy. Moreover, in order to monitor the diagnostic accuracy of primary-care physicians, the clinical records of primary-care physicians should be reviewed by neurotologists. This could also be effective in improving diagnostic accuracy and decreasing the number of patients with vertigo or dizziness.
• Vertigo and dizziness are very frequent patient complaints in clinical practice
• Approximately 40–80 per cent of patients do not receive a definitive diagnosis and appropriate therapy
• In the present study, 47.0 per cent of the reference letters did not include a definitive diagnosis
• Of all patients, 67.3 per cent received a different diagnosis from primary care physicians than from specialised neurotologists, and inappropriate therapies were delivered
• Training or artificial intelligence systems with diagnostic strategies for vertigo and dizziness can help to improve diagnostic accuracy
Acknowledgements
We would like to thank the physicians at the affiliated clinics and hospitals who provided us with the medical information of the patients. We also thank Editage (www.editage.jp) for English language editing. This work was supported by the Japan Society for the Promotion of Science KAKENHI grant (number 18K09354 Grant-in-Aid for Scientific Research (C)), Japan Agency for Medical Research and Development (grant number 18dk0310092h000) and a Health and Labour Sciences Research grant for Research on Rare and Intractable Diseases (H29-Nanchito (Nan)-Ippan-031) from the Ministry of Health, Labour and Welfare of Japan.
Competing interests
None declared





