Introduction
Isolated sphenoid sinus disease can prove a challenge regarding diagnosis and management, as the underlying cause will often have an insidious onset and non-specific symptoms.Reference Socher, Cassano, Augustinho, Cassano and Felippu1 The sphenoid sinus was first described by Proetz in 1948 and has important anatomical relationships. It is situated in the skull base with close anatomical relations to cranial nerves and vascular structures.
Extramedullary haematopoiesis is the production of haematopoietic elements in areas other than the usual sites in the bone marrow of the proximal long bones, spine, sternum and pelvis. Such areas are most frequently found at sites of fetal haemoglobin production, including the liver, spleen and lymph nodes.Reference Ittipunkul, Martin, Siriwanasan, Olanratanachai and Rootman2
The authors report an unusual clivus lesion, which proved to be a site of extramedullary haematopoiesis.
Case report
A 32-year-old, Indian woman with β thalassaemia and sickle cell disease presented with a 2 cm mass in the clivus and posterior aspect of the sphenoid sinus, identified on magnetic resonance imaging (MRI). She had been under investigation by the haematologists and neurosurgeons, having presented with a two-year history of memory disturbance and headaches. The memory disturbance included both short and long term amnesia, associated with frontal and occipital headaches that were progressive and intermittent in nature. There was no history of nasal symptoms or visual disturbance. In addition to her haematological condition, the patient also suffered from migraines. She reported up to 11 sickle crises a year, requiring a significant amount of time off work. Folic acid supplements and prophylactic penicillin V had been prescribed for her sickle cell disease.
Examination revealed a nasal septal deviation to the right, with satisfactory access to the sphenoid sinus from the left. There was no evidence of any focal neurological pathology.
Laboratory investigation included a full blood count with differential and histopathological examination of a peripheral blood film, which demonstrated a microcytic anaemia with sickle cells, polychromasia, target cells and Howell–Jolly bodies. All these findings were in keeping with the patient's original haemoglobinopathy.
Radiological investigation included a computed tomography (CT) scan of the petrous bones (Figure 1) and an MRI scan of the head (Figure 2), in order to further characterise the lesion. The CT scan demonstrated a lesion affecting the base of the sphenoid and extending up to the posterior clinoids, more so on the left, and reaching the base of the pterygoid plates on the left. These features were considered to be consistent with a haemangioma. However, the MRI scan suggested that the lesion was not particularly vascular; the differential diagnosis included chordoma, dermoid cyst and fibrodysplasia, as there was little bony expansion.
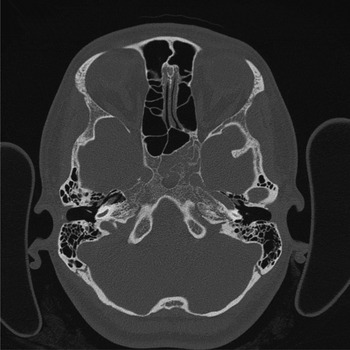
Fig. 1 Axial computed tomography scan of petrous temporal bones, demonstrating a central and left-sided, heterogeneous clivus lesion.
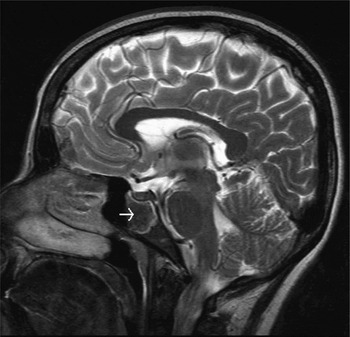
Fig. 2 Sagittal magnetic resonance imaging of the head, demonstrating a clivus lesion (arrow).
The patient underwent endoscopic, image-guided, trans-sphenoidal biopsy of her clivus lesion, which was confirmed to be quite vascular; considerable bleeding was encountered on removal of the bone overlying the lesional tissue in the basisphenoid medial to the carotid artery. However, a satisfactory tissue sample was obtained for histological analysis, and the patient made an uneventful post-operative recovery.
Histological analysis showed cellular haematopoietic tissue demonstrating erythroid hyperplasia, and small B lymphoid collections of uncertain significance. The haematologists organised a bone marrow examination. The bone marrow aspirate, trephine and cell marker studies did not show abnormal or increased lymphocyte population. The clivus biopsy was interpreted as being haemopoietic tissue consistent with a site of extramedullary haematopoiesis.
Haemoglobin electrophoresis and a positive sickle cell solubility test were consistent with compound heterozygosity for haemoglobin S and β thalassaemia. The patient was treated with hydroxycarbamide by the haematologists, which had the twin benefits of reducing her painful crises and also shrinking the 2 cm haematopoietic lesion in her head.
Discussion
Two major case series of isolated sphenoid sinus disease identified sphenoid sinus cystsReference Wang, Kanoh, Dai, Kutler, Xu and Chi3 and mucocelesReference Socher, Cassano, Augustinho, Cassano and Felippu1 as the most frequent causes, with sphenoid sinusitis as the next most common cause in both series. One of the clinical differential diagnoses considered in our patient was chordoma, recorded as one of the rare causes of isolated sphenoid sinus disease.Reference Socher, Cassano, Augustinho, Cassano and Felippu1 Fibrous dysplasia of the sphenoid sinus has been documented, presenting with headacheReference Selmani, Aitasalo and Ashamnalchi4 and seizures.Reference Mueller, Dolan and Yur5 A case series of chrondromyxoid fibromaReference Keel, Bhan, Liebsch and Rosenberg6 arising variously from the clivus and sphenoid sinus reported diagnostic difficulty upon histological assessment.
In Wang and colleagues' series of 122 cases of isolated sphenoid sinus disease, the most frequent presenting symptom was headache.Reference Wang, Kanoh, Dai, Kutler, Xu and Chi3 Our patient also complained of headache, although her memory disturbance appears to be unique when compared with the clinical picture of other sphenoid sinus lesions. Other complaints frequently reported in cases of sphenoid sinus disease are visual symptoms, cranial nerve palsies and nasal symptoms.
The radiological changes seen in (particularly homozygous) β thalassaemia patients (on skull plain radiographs) include osteopenia, widening of the diploic spaces and a ‘hair-on-end’ appearance.Reference Orzincolo, Castaldi, Scutellari and Franceschini7 It has also been reported that skeletal changes are more evident in untreated patients who have not had blood transfusions or chelation therapy.Reference Ittipunkul, Martin, Siriwanasan, Olanratanachai and Rootman2, Reference Orzincolo, Castaldi, Scutellari and Franceschini7, Reference Joseph, Rajshekkar and Chandy8 Our patient was heterozygous for the disease and such changes were not seen. It is well documented that CT and MRI are the best forms of imaging for lesions in the region of sphenoid sinus.Reference Socher, Cassano, Augustinho, Cassano and Felippu1, Reference Wang, Kanoh, Dai, Kutler, Xu and Chi3, Reference Mueller, Dolan and Yur5 Early reports describe intracranial sources of extramedullary haematopoiesis demonstrated on CT;Reference Lund and Aldridge9 however, these were not specifically located in the region of the sphenoid sinus.
Other cases of extramedullary haematopoiesis involving cranial bones have been documented. Extramedullary haematopoiesis is associated with myeloproliferative disorders, including chronic myelogenous leukaemia, polycythaemia vera, essential thrombocytosis and myelofibrosis with myeloid metaplasia, and also with chronic anaemia states, including sickle cell disease and β thalassaemia (as in our patient). Extramedullary haematopoiesis has been reported in the lacrimal fossa in a patient with known myeloproliferative disorder and myelofibrosis.Reference Baskurt, Raghavan and Trelka10 One case report has described extramedullary haematopoiesis within the marrow cavity of both the ethmoid and sphenoid sinuses, presenting with bilateral optic atrophy in a patient with β thalassaemia and haemoglobin E disease, who was successfully treated with monthly blood transfusions and low dose radiotherapy.Reference Ittipunkul, Martin, Siriwanasan, Olanratanachai and Rootman2
Proposed mechanisms for the spread of extramedullary haematopoiesis include: deposition of haematopoietic stem cells from the circulation; masses arising from fetal sources of haematopoietic stem cells; and direct extension from adjacent bone marrow.Reference Baskurt, Raghavan and Trelka10 The hypothesis that one of the former two suggested mechanisms may be responsible for our patient's presentation is appealing, but more research is needed in this area.
Extramedullary haematopoiesis has been reported within the sphenoid sinus only once before in a patient with β thalassaemia and sickle cell disease.Reference Joseph, Rajshekkar and Chandy8 This patient presented with seizures. The main difference with our patient, apart from the presentation, was that our patient's lesion involved the basisphenoid component of the clivus rather than the sphenoid sinus itself. Our patient therefore represents the first reported case of extramedullary haematopoiesis in the clivus in a patient with β thalassaemia and sickle cell disease.




