Critical aortic stenosis is defined as ductal-dependent systemic perfusion and/or moderate to severe left ventricular dysfunction requiring neonatal surgical aortic valvotomy or balloon aortic valvuloplasty. It is often associated with a variable degree of hypoplasia of other left heart structures, including the mitral valve, left ventricle, and aorta. Reference Hickey, Caldarone and McCrindle1 The management of a neonate with critical aortic stenosis may be aortic valve intervention to maintain biventricular circulation versus univentricular palliation. This depends on the combination of defects and degree of hypoplasia, as there is a spectrum of what constitutes acceptable left heart structures to support a full cardiac output.
In order to predict successful outcome associated with biventricular versus univentricular palliation in neonates with critical aortic stenosis, there are several published scoring systems: Rhodes, Reference Rhodes, Colan, Perry, Jonas and Sanders2 Congenital Heart Surgeons’ Society (CHSS) 1, Reference Lofland, McCrindle and Williams3 Discriminant, Reference Colan, McElhinney, Crawford, Keane and Lock4 CHSS 2 Reference Hickey, Caldarone and Blackstone5 ; all calculate a risk score based on patient and echocardiographic characteristics like left heart dimensions and appearance of the left ventricular endocardium. Currently, the scores are available to risk stratify individual patients with critical aortic stenosis. In addition, the more recently described 2 V score predicts success of biventricular palliation in neonates with evidence of left ventricular hypoplasia. Data are limited on their comparative applicability and success retrospectively in predicting outcome.
This study aims to determine retrospectively whether any published scoring system accurately predicted outcomes in a series of neonates with critical aortic stenosis who underwent neonatal aortic valve intervention with the expectation of successful biventricular circulation after this intervention alone based on local expert opinion. Given the spectrum of left heart disease and variability in the size/anatomy of left heart structures in critical aortic stenosis, Reference Cohen6,Reference Ma and Huang7 we hypothesise that the scoring systems may incorrectly favour a univentricular palliation in many neonates who were able to tolerate biventricular circulation.
Methods
This was a single centre, retrospective cohort study including all neonates with critical aortic stenosis at Children’s Hospital of Wisconsin who underwent only neonatal aortic valve intervention with intent to sustain biventricular circulation. Decision to proceed with surgical versus transcatheter intervention was based on local clinical consensus at the time of neonatal presentation, and echocardiographic scoring systems were not prospectively applied.
Demographic data, date, and type of initial intervention (surgical aortic valvotomy versus balloon aortic valvuloplasty), outcome including success of biventricular circulation, and need for other procedures were collected from the medical record. Success of biventricular circulation was defined as survival to discharge home following the initial aortic valve intervention with intact biventricular circulation.
In addition, the following echocardiographic data (as shown in Tables 1 and 2) from the initial postnatal study prior to aortic valve intervention were collected: mitral valve annulus diameter (long axis, apical 4 chamber); left ventricle long axis, right ventricular long axis, and heart long axis length; minimum left ventricular outflow tract diameter, aortic valve, aortic root (sinus), ascending aorta, mid aortic arch, and main pulmonary artery diameter; endocardial fibroelastosis grade (0 = none, 1 = only papillary muscle involvement, 2+ some endocardial involvement, and 3 = extensive endocardial involvement), left ventricle dysfunction (none, mild, moderate, severe), and tricuspid regurgitation (none, mild, moderate, severe).
Table 1. Demographics of patients undergoing surgical versus transcatheter intervention

p-values by Mann–Whitney tests.
BiV: biventricular; LV: left ventricle; LVOT: left ventricular outflow tract; MPA: main pulmonary artery; MV: mitral valve.
Table 2. Relationship of echocardiographic parameters with outcome

p-values by Mann–Whitney tests.
BiV: biventricular; LV: left ventricle; LVOT: left ventricular outflow tract; MPA: main pulmonary artery; MV: mitral valve.
These parameters were used to calculate the following scores: Rhodes, CHSS 1, Discriminant, CHSS 2, and 2 V score (Table 3). While Rhodes score predicted mortality, CHSS 1, 2, Discriminant score, and 2 V score predicted survival benefit. With CHSS 1 and 2 scores, a positive number favoured Norwood palliation and the magnitude of the number represented the predicted difference in percent survival benefit for the optimal pathway.
Table 3. Formula and cut-off utilised for the individual scores
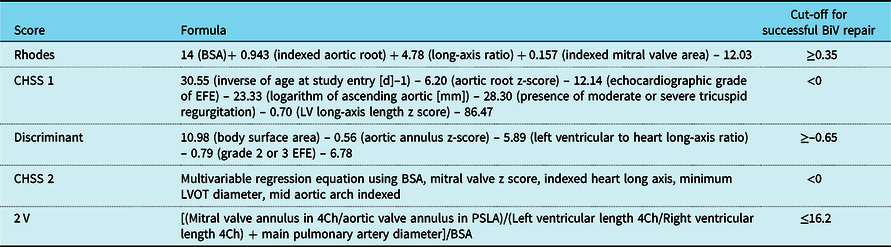
BiV: biventricular; EFE: endocardial fibroelastosis; LVOT: left ventricular outflow tract.
Statistical analysis
Mann–Whitney tests were used to compare demographic and anatomic characteristics between those who maintained a biventricular circulation following only aortic valve intervention versus those who did not maintain biventricular circulation at hospital discharge. Mann–Whitney tests were also used to compare the distribution of the various scores for these two groups of patients. Positive predictive value of the scores (percent successful biventricular palliation among those predicted to have a successful biventricular palliation) was calculated using cut-off values for the scores recommended by the authors. Reference Rhodes, Colan, Perry, Jonas and Sanders2–Reference Hickey, Caldarone and Blackstone5
Results
Between January 1999 and December 2017, 68 patients with critical aortic stenosis underwent neonatal surgical aortic valvotomy versus balloon valvuloplasty. Diagnosis was confirmed by initial echocardiogram at a median age of 1 day (range 0–28 days). Average birth weight was 3.2 kg (range 1.9–4.9 kg). Median age at initial intervention was 4 days (range 1–29 days); 35 (51%) patients underwent surgical valvotomy; and 33 patients (49%) underwent balloon valvuloplasty. There were no significant differences between the groups undergoing surgical valvotomy versus balloon valvuloplasty in terms of height, weight, age at intervention, or individual echocardiographic parameters (Table 1).
Of the 68 patients, 60 (88%) maintained a successful biventricular circulation. Of the eight patients who failed biventricular palliation: three had subsequent univentricular palliation (at 12–19 days following initial intervention) – all of these patients had undergone preceding balloon valvuloplasty with failure of recovery of left ventricular function after the intervention, four died prior to discharge with biventricular circulation due to multiorgan dysfunction and brain haemorrhage (precluding univentricular repair or transplant), and one underwent heart transplant prior to discharge after failure of biventricular circulation as the patient was deemed too high risk for univentricular palliation.
Of the individual echocardiographic parameters, left ventricular outflow tract diameter (p = 0.027), aortic valve annulus size (p = 0.003), ascending aorta dimension (p = 0.018), and right ventricle long axis length (p = 0.03) were significantly different between the patients who maintained successful versus unsuccessful biventricular circulation after aortic valve intervention (Table 2). Median left ventricle outflow tract diameter (6.2 versus 5.2 mm), median aortic annulus diameter (6.3 versus 5.1 mm), and ascending aortic diameter (9 versus 7 mm) were significantly larger in patients undergoing successful biventricular palliation; in addition, there was a trend towards larger aortic sinus diameter (8 versus 7.3 mm; p = 0.06) being associated with successful biventricular palliation after initial intervention.
The five scoring systems were applied using their newborn echocardiogram to assess the predictive value retrospectively. Overall, none of the binary score predictions (using proposed cut-offs) were significantly associated with actual outcome (% of patients who achieved successful biventricular circulation). The results for each individual scores are included in Tables 4–8.
Table 4. Summary of % successful BiV repair among those with BiV/UniV predicted by the Rhodes score

BiV: biventricular; UniV: univentricular.
The Rhodes score was the least accurate, as it failed to predict outcome in the majority of patients. The Rhodes score recommended a biventricular approach in 2/68 patients, and 1 (50%) maintained successful biventricular circulation after aortic valve intervention. Of the remaining 66 patients who had a Rhodes score recommending a univentricular approach, 59 (89%) patients maintained successful biventricular circulation after aortic valve intervention (Table 4).
The CHSS 1 score recommended a biventricular approach in 39/68 patients, and 37 (94%) maintained successful biventricular repair after aortic valve intervention. Of the remaining 29 patients who had a CHSS 1 score recommending a univentricular approach, 23 (79%) patients maintained successful biventricular circulation after aortic valve intervention (Table 5).
Table 5. Summary of % successful BiV repair among those with BiV/UniV predicted by the CHSS-1 score

BiV: biventricular; UniV: univentricular.
The discriminant score recommended a biventricular approach in 14/68 patients, and all maintained successful biventricular repair after aortic valve intervention. Of the remaining 54 patients who had a discriminant score recommending a univentricular approach, 46 (85%) patients maintained successful biventricular circulation after aortic valve intervention (Table 6).
Table 6. Summary of % successful BiV repair among those with BiV/UniV predicted by the discriminant score

BiV: biventricular; UniV: univentricular.
The CHSS 2 score recommended a biventricular approach in 59/68 patients, and 54 (91%) maintained successful biventricular circulation after aortic valve intervention. Of the remaining nine patients who had a CHSS 2 score recommending a univentricular approach, six (66%) patients maintained successful biventricular circulation (Table 7).
Table 7. Summary of % successful BiV repair among those with BiV/UniV predicted by the CHSS-2 score

BiV: biventricular; UniV: univentricular.
The 2 V score recommended a biventricular approach in all 68 patients and 60 (88%) maintained successful biventricular circulation after aortic valve intervention. No patients were predicted to undergo univentricular repair by this score (Table 8).
Table 8. Summary of % successful BiV repair among those with BiV/UniV predicted by the 2 V score

BiV: biventricular; UniV: univentricular.
Figure 1 plots the success of each individual patient within each scoring system and helps illustrate the variability of each scoring system in accurately predicting outcome. The Rhodes score strongly favoured univentricular palliation for the majority of patients who had successful biventricular palliation. In contrast, the CHSS 2 and 2 V scores more accurately predicted the observed outcome for majority of the cases.

Figure 1. Distribution of scores. The boxes indicate patients correctly predicted in each scoring system. The vertical position of the dots does reflect the scores’ numeric values, so those closer to the dotted line (author recommended cutoff) are more borderline scores.
Discussion
This study examined the retrospective success of published echo-derived scoring systems to accurately predict successful biventricular circulation in a cohort of neonates with critical aortic stenosis. In summary, none of the binary score predictions of biventricular versus univentricular (using that score’s proposed cut-offs) were significantly associated with the observed outcome in this cohort. In particular, the Rhodes and Discriminant scores predicted the need for a univentricular approach in the majority who maintained biventricular circulation after neonatal aortic valve intervention. Only the CHSS 1 and 2 and 2 V scoring systems predicted successful biventricular repair in the majority who maintained biventricular circulation. Overall, a high percentage of those predicted to need univentricular palliation by any of the scoring systems had successful biventricular repair: 89.4% by Rhodes, 79.3% by CHSS 1, 85.2% by Discriminant, and 66.7% by CHSS 2 score.
The CHSS 2 and 2 V scores were more successful in accurately predicting biventricular palliation for a majority of our cohort. CHSS 2 score was the most accurate, and this is likely secondary to its reliance on left ventricle outflow tract dimension as opposed to aortic valve or root dimensions. Reference Hickey, Caldarone and Blackstone5 Larger absolute measures of the left ventricle outflow tract and aortic outflow diameters from the initial neonatal echocardiogram were associated with a successful biventricular approach. A small aortic valve z-score has been shown to be risk factor for failure of biventricular palliation, especially in very young children; Reference Colan, McElhinney, Crawford, Keane and Lock4 however, inclusion of minimum left ventricle outflow tract dimension allows identification of additional neonates with more diffuse left ventricle outflow tract hypoplasia who may respond poorly to aortic valve intervention alone. Reference Hickey, Caldarone and Blackstone5
The 2 V score Reference Mart and Eckhauser10 was created to predict success of biventricular circulation in neonates with left heart hypoplasia complex, but specifically excluded those with significant aortic stenosis. It is focused on ratios of mitral to aortic valve size and left ventricle to right ventricle size ratios and also included main pulmonary artery diameter in the equation. When applied to our cohort, it predicted biventricular palliation in all 68 patients, likely reflecting that left heart dimensions, and not the presence of critical aortic stenosis, are the most important discriminators of predicting successful biventricular circulation. In particular, the significant differences in left ventricle outflow tract diameter, aortic valve annulus, and ascending aorta diameter were found in our cohort, with patients who underwent successful biventricular palliation having larger absolute diameters. Past studies have shown that indexed left ventricle outflow tract diameter smaller than 16 mm/m2 (equivalent to 4 mm for a body surface area of 0.25 m2) confer disproportionately poor predicted survival after biventricular palliation. Reference Mart and Eckhauser10 Hypoplastic aortic annulus has also been previously shown to be associated with biventricular repair failure. Reference Cavigelli-Brunner, Bauersfeld and Pretre11 The difference in right ventricle length in our cohort is harder to explain and suggests that this may have a more challenging dimension to consistently estimate, especially given the expected trabecular appearance of the right ventricular endocardium.
Interestingly, there was no difference in the mitral valve dimension between groups in this study. In another recent study, patients with mitral valve measurement of <8 mm with abnormal subvalvar apparatus on intraoperative assessment benefited from single ventricle palliation. Reference Mery, Nieto and De Leon8 Average mitral valve annulus size in our study was greater than this prior study (10.7 mm), as we chose to include only those undergoing aortic valve intervention. We intentionally excluded those who also required neonatal mitral valve surgery, as we believe this is an important predictor of outcome. In our institutional approach to critical aortic stenosis, we focus on a combination of 2D echocardiographic measurements of left heart structures, particularly mitral valve, left ventricle outflow tract, aortic annulus, and ascending aorta diameters, but use the presence of an apex-forming left ventricle as a key determinant in expecting biventricular circulation.
In recent studies, cardiac MRI has been shown to be helpful in assessing adequacy of left heart for biventricular palliation. Reference Grosse-Wortmann, Yun and Al-Radi12,Reference Banka, Schaetzle, Komarlu, Emani, Geva and Powell13 Banka et al. showed that in borderline hypoplastic left heart patients, a larger left ventricular end diastolic volume, left ventricle-to-right ventricle stroke volume ratio, and mitral-to-tricuspid inflow ratio were associated with successful biventricular conversion. Reference Banka, Schaetzle, Komarlu, Emani, Geva and Powell13 Mery et al. described utilising intraoperative assessment of the mitral valve to determine size, quality of the subvalvar apparatus, and leaflet morphology, and in some instances aortic valve inspection, in determining adequacy of the left heart structures. Reference Mery, Nieto and De Leon8 We did not routinely perform cardiac MRI on this patient cohort, and consistent data on intraoperative assessment of left heart structures were not available. We believe that assessment of ventricular volumes by cardiac MRI and 3D echocardiography imaging of the mitral valve to assess size and morphology in conjunction with 2D echocardiographic assessment of individual left heart structures in terms size and morphology hold potential to additionally guide this complex decision.
This study is limited by its retrospective nature, small cohort of patients who did not receive biventricular repair and lack of a consistently applied model to prospectively make the decision about appropriateness of biventricular palliation for this cohort (based on local expert consensus).
Conclusion
In summary, previously published scoring systems based on echocardiographic markers do not predict outcome accurately and reliably in neonates with isolated critical aortic stenosis. However, CHSS 2 and 2 V were more likely successfully predict outcome when retrospectively compared to local expert opinion decision-making. Larger absolute measures of left ventricle outflow tract and aortic outflow diameters were significantly associated with successful biventricular circulation, and so adequacy of these structures is likely critical components in the assessment of adequacy of left heart structures suitable for biventricular circulation in critical aortic stenosis.
Acknowledgements
None.
Financial Support
This research received no specific grant from any funding agency, commercial, or not-for-profit sectors.
Conflicts of Interest
None.
Ethical Standards
The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national guidelines on human experimentation (please name) and with the Helsinki Declaration of 1975, as revised in 2008, and has been approved by the institutional committees of Medical College of Wisconsin.












