Inappropriate antimicrobial use has been described as the most important preventable cause of drug resistance (Reference Costelloe, Metcalfe, Lovering, Mant and Hay1). Consequently, antimicrobial stewardship programs (ASPs) were implemented in several countries, aiming to provide prescribers with up-to-date and pragmatic therapeutic recommendations for prudent antibiotic prescribing (Reference Lee, Cho, Jeong and Lee2). These recommendations have been integrated into computer prescriber order entry and electronic patient record (EPR), as contextual recommendation or as clinical decision support system (CDSS) (Reference Forrest, Van Schooneveld TC, Schulz, Duong and Postelnick3;Reference Baysari, Lehnbom, Li, Hargreaves, Day and Westbrook4). Most CDSSs include automatic data processing for clinical decision making in antimicrobial treatment, and some of them integrate alerts to optimize antimicrobial dosing, or antimicrobial de-escalation after empiric treatment, aimed for treatment monitoring (Reference Agwu, Lee and Jain5). Nevertheless, recent literature shows that the benefits of these systems are limited (Reference Baysari, Lehnbom, Li, Hargreaves, Day and Westbrook4) and even disappointing because they fail to take into account clinicians’ needs and workflows, leading to poor engagement (Reference Rawson, Moore and Hernandez6). Very few interventions report predeployment analysis of clinicians’ decision-making process to justify CDSS intervention design (Reference Rawson, Moore and Hernandez6).
In sum, clinicians have to deal with three main difficulties. First, it is difficult to know if the proposed recommendation embedded into a CDSS fits the singular clinical situation of a patient (Reference Westphal, Jehl, Javelot and Nonnenmacher7) and if the algorithm takes into account all the relevant variables of the situation. Second, the starting or end time of the treatment, depending on the severity of the disease and related to the possibility to wait for a documentation strategy, is difficult to determine. Third, the automatic alerts for prescriptions could be excessive, nonpractical, and nonactionable because they cause numerous false-positive alerts, which requires more attention to evaluate each alert before deciding to make a prescription (Reference Forrest, Van Schooneveld TC, Schulz, Duong and Postelnick3). Moreover, the time required to respond to an alert for de-escalating therapy is not always the time needed by clinicians to reach a medical decision. Thus, alerts cannot replace good clinical judgment (Reference Forrest, Van Schooneveld TC, Schulz, Duong and Postelnick3).
Historically, in many hospitals, clinicians informally used to ask for the counsel of an infectious diseases specialist (IDS), which may be informal. Because this activity is time costly for the infectious disease department (IDD), telephone counseling was developed and implemented. Thus, clinical situations for the patients during a consultation can be appraised by telephone or by the IDS moving to the patients’ bedside for complex situations (Reference Yinnon8). Generally, it was argued that telephone counseling might be less effective than formal consultation and IDS consultation to patients’ bedside (Reference Forsblom, Ruotsalainen, Ollgren and Järvinen9), but it is not clear whether the reason to move to the bedside is to access the patient's record or to allow physical examination of the patient.
Moreover, informal information sharing by telephone could contain exchange of inaccurate or insufficient information between physicians and the IDS, driving to inappropriate antibiotic prescription (Reference Yinnon8). Thus, telephone counseling may be related to insufficient availability of relevant and accurate information. Furthermore, the insufficient traceability of information related to the IDS counsel may lead to the misunderstanding of the reasons for medical decision making (for example to modify antimicrobial prescription) by the physicians the next day.
This study has two aims. The first aim is to present the tele-expertise system, designed to improve the availability of information needed for understanding of the clinical situation and consequently for medical decision, and to improve the traceability of the information provided by the IDS to prescribers facilitating the monitoring and the re-assessment of patients. The second aim is to assess the diffusion of the system and its perceived utility by medical managers. This system combines telephone counseling and specific forms that are an integrative part of the EPR to record the analysis of the clinical situation, indications, and precisions related to treatment modes and monitoring.
We will, first, present the design of the tele-expertise system in a French university hospital. Second, we will present the method used to assess its diffusion and its perceived utility. Third, the results will be discussed and compared with the literature on antimicrobial stewardship and use of CDSS.
DESIGN AND IMPLEMENTATION OF AN ENABLING TELE-EXPERTISE SYSTEM: THE CASE OF THE UNIVERSITY HOSPITAL OF MONTPELLIER
In 2012, the University Hospital of Montpellier (France) shifted its method of clinical documentation (e.g., patient charts and flowsheets, medication order) from a paper-based system to an EPR. The hospital center is in the south of France and features approximately 2,000 beds in seventy-four different departments. Overall, the hospital staff consisting of 6,000 caregivers, 1,400 doctors (physicians, anesthetists, and surgeons), and 500 residents provides treatment to more than 235,000 inpatients and 540,000 outpatients annually. The new EPR system, which is an information technology (IT)-based enterprise-wide healthcare solution was designed to support all aspects of patient care, covering medical and paramedical notes and reports, physician order entry and treatment plans, laboratory management system, operating room management system, billing, and follow-up procedures. This “off-the-shelf” EPR was implemented in 9 months with a task force of one physician, one pharmacist, three manager nurses, and 100 full-time technicians recruited for the customization during 1 year. The EPR allows customization and configuration of patients’ records through setting of new forms, queries, and personalized views.
Aware of these opportunities, an IDS decided to formalize the counseling activity and customize the EPR for his team. His aim is to facilitate the IDS’ daily practice of providing counsel to clinicians from every department and to increase the traceability of the activity of the IDD. For this, in collaboration with the other IDS, a form was designed and deployed for the IDS initial assessment, for the re-assessment and for the decisions made during the team consultation meeting of all the IDS, the pharmacist, the microbiologist, and the infection control team. The global process is described in Figure 1.
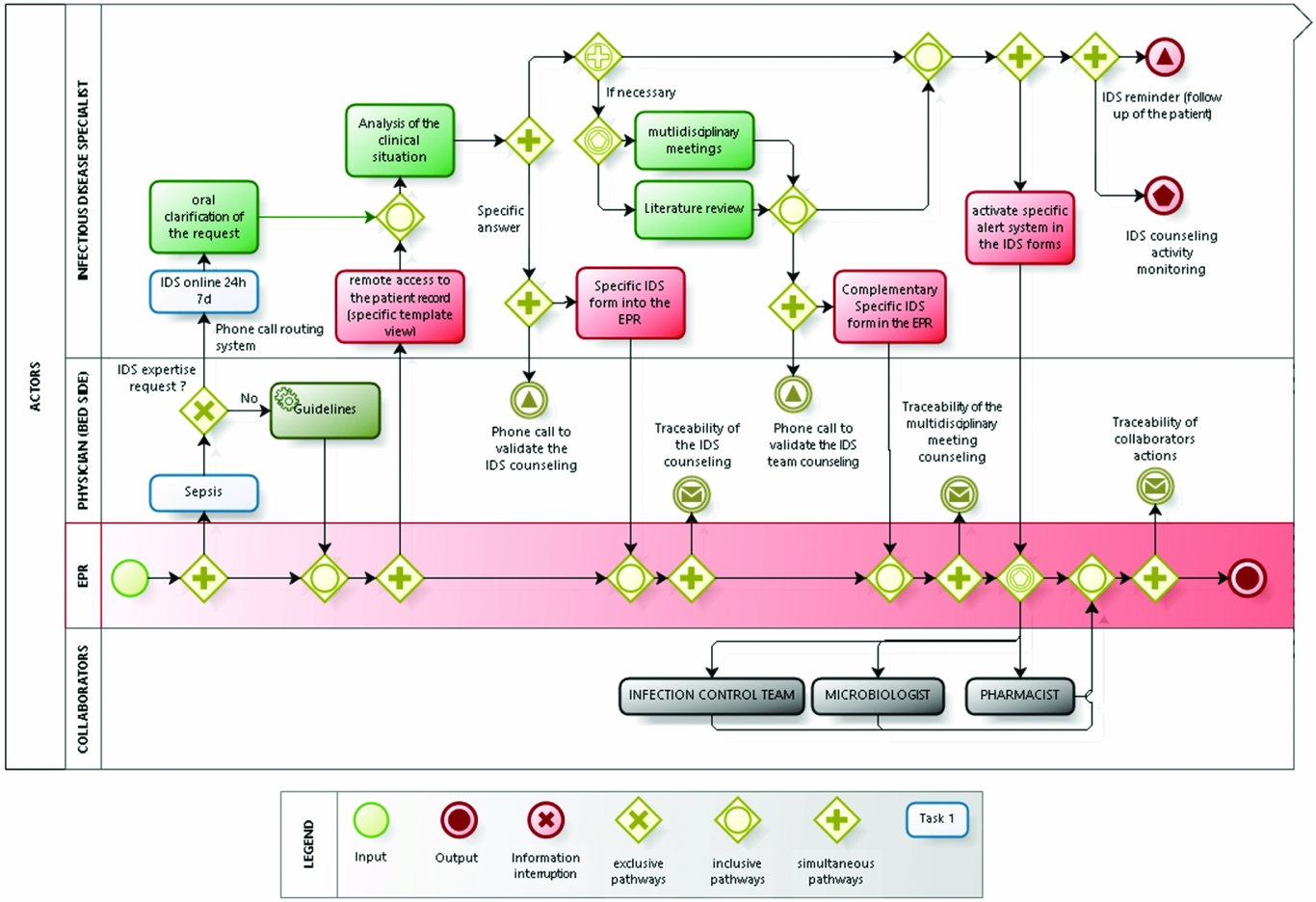
Figure 1. The tele-expertise process.
When a clinician needs more specific information than provided by standard recommendations embedded into the EPR, he or she may contact the IDS on a unique telephone number 24 hours a day, 7 days a week. A Web-based telephone call routing system is used to switch the telephone line to the IDS on call, which may change daily according to availability schedule. The requesting clinician briefly explains the medical situation and the degree of emergency and the IDS may ask for additional clarifications on the request. The call is then followed by a remote access by the IDS to the full patient's record (including laboratory results, radiology, medical and nurses’ notes), with a specific template view (inflammation biomarkers graphs, table of microbiological results, past antimicrobial use). The information recorded includes the IDS’ previous advices, allowing follow-up care.
These advices focus mainly on the diagnosis of infectious diseases or on the therapeutic use of the appropriate antimicrobial strategy, but they may also be related to the infection control issues, unexplained fever, accidental exposure to biological fluid or rabies exposure. The IDS may choose to respond make an answer alone and may justify his or her response by providing hypertext links to scientific articles. For complex cases, the clinician may decide that the response require a decision made by the team consultation meeting of the all IDS, the pharmacist, the microbiologist, and infection control team.
The IDS's response is recorded in a specific IDS form into the EPR and available in real time for all the clinicians. To enable clinicians to make medical decisions, IDS do not make any prescription, they only provide and record argued counsels.
Originally, the specific IDS form was designed to record the medical reasoning and the diagnosis or therapeutic proposal, the identification details of the IDS and of the patient with a timestamp. Later, the users’ remarks and all input errors were taken into account. Consequently, all unused or ambiguous fields were removed.
The information framing is based on: (a) ergonomics choices, as tabs that designate the steps of the counseling, combo boxes, checkbox, under form for the use of the typical instructions associated with dosages and monitoring of each suggested drug; (b) standardized requirements and mandatory elements, as remote or bedside assessment, allergies related to anti-infective drug, and monitoring decisions; (c) indexing of each situation by combining the clinical category of infection, the pathogens classes (bacteria, viruses, etc.), and the disease context (i.e., immunosuppression, cancer, pregnancy, etc.).
The most important elements, as the analysis of the clinical situation, its history and therapeutic proposal, are described in narrative text. The size has been defined to fit the work practices of each IDS. An input help has been added. Requests have been computerized to allow monitoring of use. Furthermore, media fields have been inserted to associate an image in the form (e.g., biological result curves or patient photos) or scientific papers concerning the clinical situation. Additionally, binary radio buttons were set up linked with the automated mailing at defined time intervals (e.g., the IDS may ask for a specific pharmaceutical monitoring).
The form evolved iteratively during the first year of use of the system. After, the rate of change of the form has slowed considerably with updates on the new instructions associated with treatment proposals and new ways to alert collaborators (Infection Control [IC] staff, microbiologists, pharmacists) for specific queries and to provide automatic instructions associated with the proposed antibiotic treatment. Especially, in the summer of 2015 a new feature was designed: every time the IDS completed the checkbox “alert the IC team,” a secured mail with essential clinical data is sent to the IC department. This applies to all major health-care associated infections and community-acquired infections with an epidemic potential (e.g., measles or tuberculosis).
Regular automatic queries provide real-time anonymous data from IDS activity, as the number of telephone calls, the regimental number, the prescriber's department, the infection class, the time passed since the first evaluation, and the antimicrobial suggestion.
In this context, an observational prospective study was conducted to assess the diffusion of the tele-expertise system and the perceived utility for the medical managers of most demanding departments.
RESEARCH SETTING
An observational prospective study was conducted in the period between August 1, 2012, and August 31, 2016, as follows: (a) The diffusion of the system was assessed based on the number of calls for tele-expertise council, the number of recorded tele-expertise notifications, and the reasons of call. (b) The assessment of the prescribers’ adherence to the tele-expertise system was made for a 1-year period between February 1, 2013, and January 31, 2014, more than 6 months after the implementation of the system. All the patient records including a notification from the IDS were reviewed and analyzed by an independent IDS. Collected data from EPR included clinical and biological data at baseline, and the modifications of the treatment made by physicians asking for a counsel during the 5 next days after the request. Moreover, the follow-up of the information from the counseling of the patients’ records after the discharge were also checked. Adherence to the therapeutic and diagnostic proposals was assessed for a particular clinical situation and not for each notification, largely due to the frequent reassessment because several notifications could concern the same tele-expertise. (c) The assessment of the perceived utility was made by six semi-structured interviews, which were transcribed and coded by thematic analysis. Our interviews were done with the managers of the most demanding medical departments.
RESULTS
Global Assessment between August 1, 2012, and August 31, 2016
During 48 months, 6,994 tele-expertise forms were completed and inserted into the EPR, relating to 4,173 inpatients. They include 4,228 initial assessments, 2,116 reassessments, and 650 ISD team meetings. The activity of IDS grew over 4 years from forty to over 330 tele-expertise (August 2016) acts per month. At the end of 2013, the IDS team decided to reschedule the medical planning to ensure a senior physician available every time for this activity. In 2016, the resources dedicated to tele-expertise were upgraded to a team of one different resident and one different senior IDS every day. Over the period of 12 months (from August 2015 to August 2016), 193 patients’ medical cases (13.6 percent of the initial assessments) were automatically reported to the IC team. This generated more than 120 investigations into patients’ files for in-depth analysis of causes (in case of major HAIs such as surgical site infections or catheter-related blood stream infections), leading to readjustment of healthcare practices (e.g., updating of surgical antibiotic prophylaxis) or implementation of specific precautions (e.g., contact tracing around a case of highly transmissible infection). Moreover, this internal signaling system increased by 300 percent the number of HAI notified to the IC team, who had until then relied solely on laboratory-based surveillance for multi-drug resistant organisms and very occasional clinical notifications for surgical site infections.
In-depth Analysis of 1-Year Activity
During the interval between February 1, 2013, and the January 30, 2014, a total of 1,386 tele-expertise forms for asking for IDS counseling were completed for 870 inpatients. Among them, 63 percent of requests were related to an initial assessment, 25 percent of a re-assessment, and 12 percent of a second consultation meeting assessment. Moreover, 87 percent of the answers were made without physician face-to-face discussion and clinical evaluation at the inpatient bedside.
During this period, an average of 116 counseling actions were reported per month, which is much lower than the total number of calls (an average of 160 calls per month). The explanation may consist in the voluntary information form embedded into the EPR. Only 12 percent of counseling was requested for diagnostic purposes while 86 percent for therapeutic advices. Antibiotic treatment was already underway in 71 percent of cases and 65 percent of cases were focused on modifying the ongoing strategy. Concerning the topic, expertise was related to bone and joint infections (27 percent), skin and soft tissue infections (18 percent), surgical infections, bacteremia (8 percent), and urinary infections (9 percent). The most demanding departments are orthopedic surgery (17 percent), ear/nose/throat (8 percent), internal medicine (8 percent), endocrinology (8 percent), cardiology (7 percent), and neurosurgery (7 percent). The other advices (45 percent) were asked by forty different departments (less than 5 percent for each). The information counseling was noticeable in the inpatient discharge letter in 43 percent of the cases. One request out of four was discussed during the IDS team consultation meeting.
Adherence was assessed for 927 clinical situations, taking into account that several tele-expertise actions may occur for the same inpatient counseling. For the diagnosis (n = 111), 79 percent counseling suggestions (95 percent confidence interval [CI],76.4–81.6 percent) were fully followed, 11 percent not followed, 6 percent partially followed, and 4 percent not evaluable.
For strictly therapeutic requests (n = 797), 87 percent of answers (95 percent CI, 84.8–89.2 percent) were followed, 5 percent partially followed, 5 percent not followed, and 3 percent nonassessable. The suggestions from the IDS consultation meeting were followed in 82 percent, partially followed in 7 percent of cases.
The reasons why the counseling was not followed (12 for the diagnosis and 40 for therapeutics) included for 80 percent the fact that the clinical situations have evolved just after the counseling and the bedside “clinicians knew what to do and didn't feel the need for a reassessment” (e.g., the severity of the clinical situation of the patient has dramatically increased and the team limited the therapeutics).
This means there were clear medical opinion conflicts for only 10 of the 927 situations. The nonassessable situation concerned rare cases of information transmission rupture, that is, error in recording the IDS advice and doubt about the fact that the team were able to read the IDS notification.
Medical managers of the departments who ask most frequently for IDS advice (representing 55 percent of the demand) considered the proposal was totally relevant and adapted in most cases, even if bedside evaluation occurred in less than 13 percent of the assessments (6 percent of first assessments and 7 percent of re-assessments).
Table 1 summarizes the main medical managers’ opinions.
Table 1. Main Medical Managers’ Opinions

DISCUSSION
This tele-expertise system was designed in the context of the French national care pathway alert for antibiotics (2011–16), which promotes counseling networks in which the role of experts in antibiotics use is emphasized. The counseling activity of IDS for other physicians is common in most hospitals. However, this requires a considerable expenditure of time by IDS (Reference Pulcini, Botelho-Nevers, Dyar and Harbarth10) because of the disparity among the necessary information sources (clinical examination, consultation and care data, laboratory results, drug prescription). Our data not only indicate that this activity is important, but also indicates an increase during the whole period of our study.
Various studies have shown that the infectious diseases services lead to the reduction of inappropriate antibiotic therapy and a decrease in antibiotics use (Reference Cisneros, Neth and Gil-Navarro11) while decreasing mortality rate (Reference Westphal, Jehl, Javelot and Nonnenmacher7). However, our objective was not to evaluate the clinical impact on patients or even the use of antibiotics, but to evaluate the adhesion of the system itself by the hospital physicians.
We were interested in the capabilities of the system to manage a large volume of patients without losing the quality of the evaluation. In addition, we wanted to confirm the IDS was able to take into account each specific clinical case and to promote the collaboration between IDS and other specialists. Most information systems are originally conceived as means of providing patient-specific information for individual patient care; however, in many situations like in ours, these systems played a more collaborative role than originally anticipated by their designers (Reference Kaplan12). In our case, the tele-expertise system designed in the EPR to support real-time antimicrobial use and the different views provided by the patient record, allowed each group to see the information in the context that made the most sense to them. The principle of different views combined with the underlying exchange of the same information helped support the collaboration between different caregivers, as elaborated by Reddy et al. (Reference Reddy, Dourish and Pratt13).
Our study outlines that prescribers’ adherence to the IDS counseling is high even if counseling is assisted by telephone and EPR use. This result is in contrast with other studies leading to the conclusion that telephone counseling or informal consultation may be less effective than formal consultation (Reference Forsblom, Ruotsalainen, Ollgren and Järvinen9;Reference Fox, Siegel and Weinstein14). This gap may be explained by the original way to link telephone and EPR use in a clinical tele-expertise decision system. For each step, the use of the EPR has been re-designed during the use, taking into account the remarks of the IDS related to the most relevant information to enable gain in time in their visualization and search (personalized view, information gathering, graphic, etc.), in terms of data record (forms, automatic queries) and in terms of collaboration to other health professionals in the hospital (pharmacy and infection control team). This tele-expertise system is based on the autonomy of the health professionals involved, meaning the IDS team (who has the autonomy to modify the EPR forms for IDS counseling, the system of call routing, and the monitoring of the activity) and for clinicians who may or not to ask for counseling and to follow the proposals made by IDS.
Moreover, the traceability of counseling into the EPR system makes available all the IDS suggestions and prescribers’ decisions to the clinical staff (including pharmacists, microbiologists and hygienist), thereby improving the coordination and continuity of care (e.g., inpatients’ transfer). This is a positive effect of using the system of tele-expertise, which is, however, difficult to assess according to cost-benefits analysis or inpatient mortality rate.
The system designed and implemented in the University Hospital of Montpellier shows that the data traceability and the telephone communication between the IDS and the prescribers may be sufficient to support the medical decision for a large number of clinical situations of antimicrobial prescription. This is a crucial element in a limited medical resources context where antimicrobial stewardship has to manage a high volume of antibiotic prescriptions wherein a large number of clinical situations do not match the guidelines. The challenge is to change the administrators and providers focus from the “antibiotic policy and guidelines” to a “quality of care initiative” (Reference Westphal, Jehl, Javelot and Nonnenmacher7).
The interviews conducted with the managers of the most demanding departments are in line with these arguments, especially when clinical guidelines are not applicable for our case. One of the main topics, as the manager of the Neurosurgery department stated, is to determine when the problem is too complex and requires bedside consultation. The real question is, thus, to find out when the remote access of the information does not allow the appropriate analysis. This could be due to the fact that the relevant information is not available in the EPR or that there could be misinterpretation of the facts between the IDS and the bedside’ clinician.
It is very important to consider that remote access and bedside consult are sometimes interchangeable whereas at other times this cannot be the case. Consequently, to discriminate among clinical situations is the next step for the system improvement. In our case, according to the actors, lots of IDS counseling for inpatients were followed by an IDS consult after discharge, as a close follow-up. Unfortunately, accurate data remained out of the scope of our study.
The main limitation of this study is seen in its observational nature that does not provide explanation for the prescribers’ adherence using the tele-expertise system compared with a control group. Moreover, we were not able to compare the tele-expertise system before and after the implementation period, because the counseling activities before were informal and decentralized.
CONCLUSION
While several studies show the benefits of CDSS for the care (Reference McGregor, Weekes and Forrest15), we were interested in the design and diffusion of a tailored tele-expertise system linking telephone calls and information recorded and stored in the EPR to improve the quality of collaboration between IDS and other specialists.
We showed that the tele-expertise system is an original way to design IT supported antimicrobial stewardship intervention based on the remote access to relevant information by the IDS and on the traceability of the medical counseling by the other clinicians. The diffusion of the system and the adherence to the counsel was assessed by a prospective observational study, showing the increasing number of calls and tele-expertise notifications during a 4-year period. The adherence was high, despite the fact that the IDS moved to the bedside was only in 6 percent of the cases. The system was able to provide efficient help for medical decision making in antimicrobial prescription in real time and to manage a high volume of clinical situations that, from the bedside clinician point of view, do not match the established guidelines.
CONFLICTS OF INTEREST
The authors have no relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript.




