Introduction
Benign paroxysmal positional vertigo (BPPV) is the most common cause of vertigo of vestibular origin.Reference Nedzelski, Barber and McIlmoyl1–Reference Lee and Kim4
Although its aetiology is not clear, there is broad consensus concerning its physiopathological mechanism and treatment. Although some authors support a neural mechanism (i.e. neuronal degeneration reducing utricular and saccular inhibition of the semicircular canals),Reference Gacek5 it is generally accepted that symptoms are due to the displacement of otoconial fragments from the utricle to the semicircular canals. They either adhere to the cupola,Reference Schuknecht6 thus increasing its relative density, or float freely inside the canal,Reference Hall, Ruby and McClure7 causing movement of the endolymph. Changes in the position of the head cause deflections in the semicircular canal's cupola, which give rise to the nystagmus and vertigo reported by patients.
Proposed treatment methods are based on these two physiopathological theories (known as cupulolithiasis and canalithiasis, respectively), and attempt to relocate the otoconial fragments and associated crystals within the utricle. Treatment techniques comprise particle repositioning manoeuvres based on either liberation (in the case of cupulolithiasis) or repositioning (for canalithiasis). The prototypes of these manoeuvres, applied to BPPV of the posterior semicircular canal (the most commonly affected semicircular canal) are the Semont manoeuvre for cupulolithiasisReference Semont, Freyss and Vitte8 and the Epley manoeuvreReference Epley9 (with subsequent amendments) for canalithiasis.
Most authors report excellent outcomes with both manoeuvres, at least with regards to immediate control of vertigo.Reference Steenerson, Cronin and Marbach3, Reference Herdman, Tusa, Zee, Proctor and Mattox10–Reference von Brevern, Seelig, Radtke, Tiel-Wilck, Neuhauser and Lempert14 However, recurrence appears to be relatively common,Reference Nunez, Cass and Furman12, Reference Sakaida, Takeuchi, Ishinaga, Adachi and Majima15, Reference Brandt, Huppert, Hecht, Karch and Strupp16 and is estimated to occur in approximately 50 per cent of cases followed up in the medium and long term.
The choice of the Semont or Epley manoeuvre basically depends on each author's personal experience. In an attempt to compare the efficacy of these two manoeuvres and that of the Brandt–Daroff exercises,Reference Brandt and Daroff17 a few years ago our research group conducted a randomised, comparative, prospective study in a group of 106 patients diagnosed with BPPV of the posterior semicircular canal.Reference Soto Varela, Bartual Magro, Santos Pérez, Vélez Regueiro, Lechuga García and Pérez-Carro Ríos18 We found similar efficacy for a single Semont or Epley manoeuvre, both of which were better than Brandt–Daroff exercises. We also found a lower recurrence rate in patients cured with a Semont manoeuvre, compared with an Epley manoeuvre. Furthermore, repetition of the Semont manoeuvre was ineffective, while repetition of the Epley manoeuvre increased the percentage of cured patients. These findings gave rise to a BPPV treatment protocol combining the two manoeuvres and the Brandt–Daroff exercises. This ‘Santiago protocol’ is shown in Figure 1.
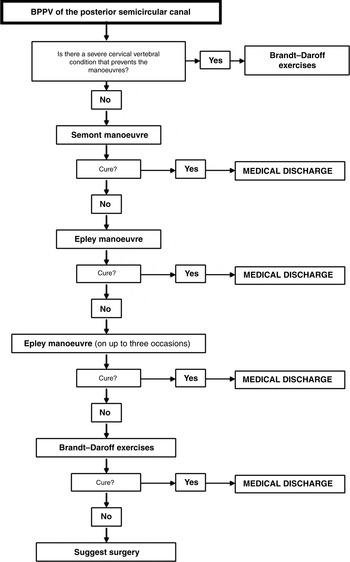
Fig. 1 Santiago protocol for treatment of benign paroxysmal positional vertigo (BPPV) of the posterior semicircular canal.
We have used this treatment regimen for patients diagnosed with BPPV of the posterior semicircular canal since April 2000.
The primary objective of the current study was to validate the efficacy of this protocol by evaluating results for short-term control of symptoms. Secondary objectives were to analyse the medium and long-term evolution of studied cases, to estimate the incidence of recurrence, and to identify factors favouring recurrence.
Materials and methods
Material
The study included all the patients consecutively diagnosed with unilateral BPPV of the posterior semicircular canal in the ENT department of Hospital Clínico Universitario de Santiago de Compostela, between April 2000 and March 2009, to ensure post-diagnosis follow up of at least one year.
All the participants consented to take part, in accordance with the Declaration of Helsinki.
The inclusion criteria specified a positive Dix–Hallpike test, with nystagmus typical of a posterior semicircular canal disorder, rotating (clockwise in the left ear and anti-clockwise in the right) with an upwards component. Nystagmus was observed with Frenzel glasses; in doubtful cases, videonystagmography was used to confirm the direction of the nystagmus.
In order to homogenise the study group as much as possible, the following exclusion criteria were applied: a negative Dix–Hallpike test (i.e. no nystagmus, even if anamnesis was consistent with BPPV); involvement of the superior and/or lateral semicircular canals (either individually or associated with the posterior canal); and bilateral involvement of the posterior semicircular canal.
Method
The protocol shown in Figure 1Reference Soto Varela, Bartual Magro, Santos Pérez, Vélez Regueiro, Lechuga García and Pérez-Carro Ríos18 was used to treat 412 patients who met the inclusion criteria. One patient had a cervical vertebral condition which made the Semont manoeuvre unadvisable. Thus, this manoeuvre was performed on 411 study patients, as follows.
Once the affected ear had been identified by the Dix–Hallpike test, the patient was seated on a gurney and their head turned 45° towards the unaffected side. They were laid down suddenly on the affected side, and kept in that position for four minutes. The patient was then suddenly turned 180° to lie on the unaffected side, while maintaining the position of the head relative to the trunk, and kept in this new position for another four minutes. Finally, the patient was asked to slowly rise, and was advised not to lie on the affected side for a week.
The patient was reviewed one week after the Semont manoeuvre and the Dix–Hallpike test was repeated.
If the test was negative and the patient was asymptomatic, they were discharged with no positional constraints. However, they were asked to return if the symptoms reappeared, and were also asked to provide a telephone number and e-mail address to enable direct contact by one of the study authors.
If the Dix–Hallpike test was still positive, the Epley manoeuvre was applied as follows.
The patient was seated on a gurney and their head turned 45° towards the affected side. Maintaining this angle, they were laid down suddenly on the side towards which their head was turned, so that their head hung at a 20° angle over the edge of the gurney. Their head (alone) was slowly turned 90° to the other (healthy) side. Their entire body was then turned until they were lying on their side, maintaining the same angle of the head relative to the body. The patient was then slowly raised to the initial position, looking forward. Finally, their head was turned 20° towards the front.
Each position was maintained until nystagmus ceased; if it did not appear in a position, that position was maintained for one minute. The cycle of positions described above was repeated until there was no nystagmus, or no improvement in two successive cycles. The patient was advised not to lie on the affected side for a week. We did not use a mastoid vibrator during this manoeuvre.
The patient was consulted one week later. If the Dix–Hallpike test was negative, they were discharged with the same instructions as above regarding symptom reappearance, after telephone or e-mail contact details had been recorded. If the Dix–Hallpike test was positive, the Epley manoeuvre was repeated.
If the Dix–Hallpike test was still positive after three Epley manoeuvre sessions (one per week), the patient was told to perform Brandt–Daroff exercises as follows: (1) sit on a gurney (or bed) and turn the head 45° towards one side; (2) lie on the opposite side and remain in that position for 30 seconds; (3) return to the initial position and turn the head to the opposite side; and (4) lie on the opposite side. The patient developes Brandt and Daroff exercises not only for a week, but until the exercises do not cause vertigo.
The patient was reviewed monthly until the symptoms disappeared or the Dix–Hallpike test was negative. If the symptoms persisted after six months, surgical treatment was suggested.
In case of recurrence after a cure (i.e. compatible symptoms and a positive Dix–Hallpike test), the treatment protocol was instigated again from the beginning (in the case of posterior semicircular canal recurrence). Recurrences in the horizontal semicircular canal were treated with Lempert manoeuvres, and those in the anterior semicircular canal with Epley and/or Yacovino manoeuvres.
Statistical analysis
The following data were analysed: sex, age at diagnosis, duration of symptoms, aetiology of BPPV, applied treatment, evolution (cure, improvement or stabilisation) and follow-up period. We also monitored recurrences (confirmed by Dix–Hallpike testing), analysing the time from cure of initial episode, the affected canal and the treatment response.
Data were entered into a database created especially for the purpose. Statistical analysis of results was performed with the Statistical Package for the Social Sciences version 15.0 for Windows software program. Fisher's exact test was used to analyse the relationship between aetiology and response to treatment and number of manoeuvres required for a cure. The same test was also used to establish the relationship between sex, affected side and number of manoeuvres initially required and recurrence, and the patients’ final status. The chi-square test was used to relate aetiology to the presence of recurrence (or not) and final status. The Mann–Whitney test was used to analyse the impact of age and duration of symptoms on recurrence and final status. Finally, the Kaplan–Meier method was used to estimate permanence without recurrence, and the Wilcoxon test to compare recurrence-free permanence curves. Statistical tests were classified as significant when the p value was below 0.05.
Results and analysis
Four hundred and nineteen patients met the study's inclusion criteria. Seven patients were excluded for not attending the visit scheduled to assess the efficacy of the manoeuvre. Therefore, the final study group comprised 412 patients (144 men and 268 women, a proportion of 1:1.86), with a mean age of 58 years (median: 59; mode: 62; range: 14–93). The distribution of patient age is shown in Figure 2. Diagnosis was more common between the sixth and eighth decades of life (273 patients, 66.5 per cent). The right ear was affected in 222 patients (54 per cent) and the left in 190 (46 per cent).

Fig. 2 Patient age distribution.
With regards to duration of symptoms, the mean at diagnosis was 11.6 months (median: two months; mode: one month), with a maximum of 30 years (referring to the first episode compatible with a diagnosis of BPPV, although with asymptomatic periods prior to diagnosis and an evolution of at least one week).
No aetiological factors were identified in 62 per cent of the patients. In the rest, the most common aetiological factors were ipsilateral vestibular neuronitis (7 per cent), head trauma (7 per cent), diagnosed ipsilateral Ménière's disease (6 per cent), hospitalisation for severe systemic disease (5 per cent) and chronic ipsilateral middle-ear disorder (4 per cent). Less commonly, patients had other factors recognised in the literature as causes of BPPV in another canal (2.1 per cent), or concomitant sudden hypoacusia syndrome (1.5 per cent), or recent otological and/or dental surgery (1 per cent). Notably, 1.5 per cent of patients had unilateral Ménière's disease in the contralateral ear.
Application of the Santiago protocol resolved symptoms (i.e. led to no subjective sensation of vertigo and a negative Dix–Hallpike test) in 404 patients (98.1 per cent), improved symptoms in another five (1.2 per cent) and had no effect in three (0.7 per cent). Of the 404 ‘cures’, one Semont manoeuvre was sufficient in 334 (81.2 per cent), with a subsequent Epley manoeuvre required in 40 (9.7 per cent), two Epley manoeuvres in 15 (3.6 per cent) and three Epley manoeuvres in five (1.2 per cent). In nine patients (2.2 per cent), one Semont and three Epley manoeuvres were not sufficient, although these patients were cured with Brandt–Daroff exercises. Finally, in one patient (0.2 per cent) these exercises were indicated in the first instance, as severe vertebral problems contraindicated use of the Semont and Epley manoeuvres. The number and percentage of patients cured with each manoeuvre are shown in Figure 3.

Fig. 3 Patients cured of unilateral benign paroxysmal positional vertigo of the posterior semicircular canal, using different treatment options within the Santiago protocol. B-D = Brandt–Daroff exercises; S = Semont manoeuvre; E = Epley manoeuvre
The condition's aetiology had no impact on its resolution. Eight patients did not achieve full resolution. The cause was unknown in five of them (62.5 per cent, similar to the figure for the entire group). Trauma was not an aetiological factor in any of them. Patients with known aetiology did not have a poorer prognosis than those in whom the origin was not identified (Fisher's exact test, p = 0.357).
Aetiology also had no impact on the number of manoeuvres required. The need for only one Semont or at less one Epley manoeuvre was not related to the idiopathic or known origin of the disorder (Fisher's exact test, p = 0.239).
Mean patient follow up was 59.7 months, with a maximum of 123.6 months and a minimum of one year. We found recurrence of symptoms in 90 patients (21.8 per cent of the total). The mean time from initial diagnosis to recurrence was 15.31 months. Figure 4 shows the estimated evolution of recurrences (Kaplan–Meier estimation), considering that follow up was interrupted in 23 cases by death from other causes. More than half the recurrences occurred in the first year after resolution of symptoms (14 per cent); after this time, the recurrence rate per year was much lower, with an estimated cumulative recurrence of 27 per cent after 10 years.

Fig. 4 Recurrence in patients with unilateral benign paroxysmal positional vertigo of the posterior semicircular canal. Estimated Kaplan–Meier cumulative percentage for recurrence: 14 per cent at one year, 18 per cent after two years, 19 per cent after three years, 23 per cent after five years and 27 per cent after 10 years.
Recurrence was predominantly in the posterior semicircular canal of the initially affected ear (62 cases, 69 per cent of the total). However, there were also recurrences in the other two canals of that ear, or in a canal of the contralateral ear (even bilaterally in one case). Table I shows the distribution of recurrences by canal.
Table I Recurrence cases: affected semicircular canal

Data represent patient numbers. SCC = semicircular canal; ipsilat = ipsilateral; contralat = contralateral; bilat = bilateral
We analysed each study factor to determine whether it influenced the likelihood of recurrence. No influence was found for sex (Fisher's exact test, p = 0.157), affected side (Fisher's exact test, p = 0.072), age (Mann–Whitney test, p = 0.192) or duration of symptoms (Mann–Whitney test, p = 0.418). With regards to aetiology, there was recurrence in 23 per cent of idiopathic cases, 27 per cent of post-trauma cases, 43 per cent of cases associated with Ménière's disease in the same ear, 19 per cent of cases secondary to vestibular neuronitis and 25 per cent of cases of other origins. However, these differences were not statistically significant (chi-square test, p = 0.272). Figure 5 shows the estimated percentage of recurrences (Kaplan–Meier estimation), comparing the cases of unknown origin with the rest. Although a larger number of recurrences could be expected in the medium term in cases of known origin compared with idiopathic cases, the differences were not statistically significant (Wilcoxon test, p = 0.208). Similar results were obtained when we compared patients with and without a traumatic origin (Figure 6), using a Kaplan–Meier estimation (Wilcoxon test, p = 0.847).

Fig. 5 Recurrence in patients with unilateral benign paroxysmal positional vertigo of the posterior semicircular canal, by idiopathic vs non-idiopathic aetiology (Kaplan–Meier estimation). Wilcoxon test: p = 0.208.

Fig. 6 Recurrence in patients with unilateral benign paroxysmal positional vertigo of the posterior semicircular canal, by traumatic vs non-traumatic aetiology (Kaplan–Meier estimation). Wilcoxon test: p = 0.847
Recurrence appeared to be less likely in patients for whom a single initial manoeuvre was sufficient to resolve symptoms (20.4 per cent), compared with those for whom several manoeuvres were required (27.1 per cent); however, this difference was not statistically significant (Fisher's exact test, p = 0.150). Use of the Kaplan–Meier estimation led to a similar result: recurrences were again less common in patients for whom a single Semont manoeuvre was sufficient, compared with those for whom several manoeuvres were required (Figure 7), but, again, this difference was not statistically significant (Wilcoxon test, p = 0.191).

Fig. 7 Recurrence in patients with unilateral benign paroxysmal positional vertigo of the posterior semicircular canal, according to the type and number of manoeuvres required to initially resolve symptoms (Kaplan–Meier estimation). Wilcoxon test: p = 0.191.
Recurrences in the posterior semicircular canal were treated with the same protocol. Recurrences in the horizontal semicircular canal were treated with the Lempert manoeuvre, while those in the anterior canal were treated with the Epley and (in the most recent cases) Yacovino manoeuvres.
After treatment and at the end of follow up, the final status of the patients was ‘cure’ (i.e. no symptoms) in 387 (93.9 per cent), ‘improvement’ in eight (1.9 per cent) and ‘persistence of symptoms’ in 17 (4.1 per cent). Patients’ final status (i.e. cure or not) was not influenced by sex (Fisher's exact test, p = 0.135), affected side (Fisher's exact test, p = 0.577), age (Mann–Whitney test, p = 0.993) or aetiology (i.e. known versus idiopathic; Fisher's exact test, p = 0.228). At the end of the follow-up period, 95 per cent of the idiopathic cases were asymptomatic, as were 95 per cent of the post-traumatic cases, 95 per cent of cases secondary to vestibular neuronitis, 86 per cent of cases associated with Ménière's disease in the same ear, and 93 per cent of cases of other origin (chi-square test, p = 0.520).
The association between the number of manoeuvres required to resolve symptoms and the patient's final status was of equivocal statistical significance (Fisher's exact test, p = 0.053); 96 per cent of patients in whom a single Semont manoeuvre was initially sufficient continued to be asymptomatic at the end of the follow-up period, while the percentage fell to 90 per cent when more manoeuvres were necessary. Recurrence substantially affected final status: only 76 per cent of patients suffering a recurrence were asymptomatic at the end of the follow-up treatment, compared with 100 per cent (obviously) of those with no recurrence (Fisher's exact test, p < 0.001).
Discussion
Particle repositioning manoeuvres are highly effective in resolving the symptoms of patients with BPPV. Specifically, when the posterior semicircular canal is affected, excellent results have been reported for both the Semont and Epley manoeuvres (and the latter's modifications).Reference Steenerson, Cronin and Marbach3, Reference Herdman, Tusa, Zee, Proctor and Mattox10, Reference Cohen and Jerabek11 Therefore, the combined use of the two manoeuvres should resolve symptoms in almost all patients. However, long-term follow up shows that recurrence is relatively commonReference Nunez, Cass and Furman12, Reference Sakaida, Takeuchi, Ishinaga, Adachi and Majima15, Reference Brandt, Huppert, Hecht, Karch and Strupp16 and, in some patients, repeated.19
Our sample's demographic characteristics (i.e. sex, age and affected side) were consistent with the literature: BPPV was more common in women,Reference Baloh, Honrubia and Jacobson20, Reference von Brevern, Radtke, Lezius, Feldmann, Ziese and Lempert21 largely affected people from 60 to 90 years of age,Reference Baloh, Honrubia and Jacobson20 and predominantly affected the right ear.Reference von Brevern, Seelig, Neuhauser and Lempert22 Also consistent with other publications was the fact that its origin was unknown in most of our patients;Reference Lee and Kim4 in the remainder, trauma, ipsilateral vestibular neuronitis and ipsilateral Ménière's disease were the most common causes.
The association between Ménière's disease and BPPV has been described and studied;Reference Gross, Ress, Viirre, Nelson and Harris23–Reference Rossi Izquierdo, Soto Varela, Santos Pérez and Labella Caballero26 however, in our study Ménière's disease was present in the contralateral ear in 1.5 per cent of patients (a much higher incidence than that expected in the general population). This could be because these patients were already being seen for their Ménière's disease and so had easier access to specialist care; in the general population, many cases of BPPV are not seen by specialists, either because they are self-limiting or because they are resolved by general practitioners. However, if we assume a possible physiopathological relationship between hydrops and BPPV (with increased endolymph pressure facilitating otoconial detachment from the utricular macula),Reference Gross, Ress, Viirre, Nelson and Harris23, Reference Perez, Martin, Zubieta, Romero and Garcia-Tapia24 these patients could have bilateral Ménière's disease with subclinical symptoms in one of the ears (in which the BPPV appears).
In our study, a single Semont manoeuvre resolved symptoms in a significant number of patients (81.2 per cent); this is similar to reported results (73 per cent) in a different group,Reference Soto Varela, Bartual Magro, Santos Pérez, Vélez Regueiro, Lechuga García and Pérez-Carro Ríos18 and is within the reported effectiveness range for a single manoeuvre (i.e. from 52 per centReference Norre and Beckers27 to 90 per centReference Herdman, Tusa, Zee, Proctor and Mattox10). Application of our Santiago protocol, with up to three Epley manoeuvres plus Brandt–Daroff exercises if necessary, resolved symptoms in almost all patients (98.1 per cent). We therefore believe that the combined use of the two manoeuvres and these exercises, according to the above protocol, can cure symptoms and result in a negative Dix–Hallpike test in practically all patients with unilateral BPPV of the posterior semicircular canal.
However, when analysing the efficacy of BPPV treatment manoeuvres, one must consider the significant number of patients with spontaneous remission (we have previously observed spontaneous resolution in 47 per cent of patients suspected of BPPV; the same percentage has been reported at one-month follow up).Reference Blakley28 However, in our current study, the treatment effect was assessed just one week after the manoeuvre, in patients who had suffered symptoms for more than 11 months on average. We therefore believe that the number of spontaneous remissions in such a short time (one week) was probably minimal in our study population.
Unlike other publications which have reported a poorer prognosis in cases of traumatic origin compared with idiopathic cases,Reference Del Río and Arriaga29, Reference Ahn, Jeon, Kim, Park, Hur and Kim30 we found no significant difference (in terms of symptom resolution or the number of manoeuvres required): our patients with a history of trauma responded to the manoeuvres similarly to patients with other aetiologies.
Over the follow-up period, recurrence appeared in just over one-quarter of our patients. This figure is close to that given by some authorsReference Steenerson, Cronin and Marbach3, 19, Reference Del Río and Arriaga29, Reference Rashad31 but much lower than that reported by others; some have predicted recurrence rates of up to 50 per cent over long-term follow-up periods.Reference Nunez, Cass and Furman12, Reference Brandt, Huppert, Hecht, Karch and Strupp16 The timing of recurrence is especially important: symptoms are most likely to return in the first year of follow up (in our study, this was true for 14 per cent of the total number of patients and approximately half of total recurrences). Although recurrence is possible after this time, it is much less likely. Some authors have reported that 80 per cent of total recurrences occur in the first year of follow up.Reference Brandt, Huppert, Hecht, Karch and Strupp16 This would justify close monitoring in the first 12 months, after which it would probably be unnecessary.
Recurrences usually affect the initially involved side, but not always. Indeed, in our study symptoms appeared in the contralateral ear in 22.2 per cent of all cases. Rather than recurrences involving a repetition of the same process, it would appear that some people are more predisposed to BPPV (possibly due to a favourable systemic factor) or have easier access to specialist care after an initial episode.
In this study, we were unable to find a factor that predicted whether a patient with unilateral BPPV of the posterior semicircular canal would suffer a recurrence. Unlike other studies, in our series a history of traumaReference Gordon, Levite, Joffe and Gadoth32, Reference Kansu, Avci, Yilmaz and Ozluoglu33 did not favour recurrence. However, the literature is not consistent in this respect, as some papers have reported a lower rate of recurrence in post-traumaticReference Ahn, Jeon, Kim, Park, Hur and Kim30 than in idiopathic cases, while other authors, like ourselves, have found no relationship between previous trauma and recurrence.Reference Suarez, Alonso, Arocena, Suarez and Geisinger34 Similarly, some authors have stated that recurrence is more common in patients younger than 40 years,Reference Rashad31 but this was not the case in our patients, as age had no impact on its likelihood. It has also been reported that the rate of recurrence is greater in patients who have suffered vertigo for less than three years;Reference Rashad31 however, duration of symptoms had no effect on recurrence in our series. Although not statistically significant, recurrence does seem more common in patients with ipsilateral Ménière's diseaseReference Del Río and Arriaga29, Reference Kansu, Avci, Yilmaz and Ozluoglu33, Reference Tanimoto, Doi, Nishikawa and Nibu35 (this is not unexpected: if increased endolymph pressure facilitates otoconial detachment, there is no reason why this should not occur on more than one occasion), and in those patients who require more than one manoeuvre to initially resolve their symptoms.
• Unilateral benign paroxysmal positional vertigo of the posterior semicircular canal was treated with combined Semont and Epley manoeuvres and Brandt–Daroff exercises
• Symptoms resolved and the Dix–Hallpike test became negative in 98 per cent of patients
• Traumatic (vs idiopathic) aetiology did not predict poor treatment response
• Recurrence was 27 per cent over 10 years, mostly in the first year
• Recurrence was more frequent with ipsilateral Ménière's disease, and in patients needing more than one manoeuvre to resolve symptoms
• The only clear predictor of poorer prognosis was recurrence
Although most cases respond to treatment, not all do. In our series, 93.9 per cent of patients were cured at the end of the follow-up period, less than the 98.1 per cent who initially responded to treatment. Recurrence is the only factor that clearly influences final status. However, two further factors appear to indicate a poorer prognosis (although lacking clear statistical significance): ipsilateral Ménière's disease and the need for more than one manoeuvre to initially resolve symptoms.
In conclusion, in unilateral benign paroxysmal positional vertigo of the posterior semicircular canal, the above treatment protocol cured 98 per cent of patients and more than half of recurrences occurred in the first year.










