Introduction
It has been suggested that theoretically the improvement in long-term psychodynamic psychotherapy (LPP) should continue several years after the end of therapy (Gabbard et al. Reference Gabbard, Gunderson and Fonagy2002; Perry & Bond, Reference Perry and Bond2009). Likewise, long-term therapy has been considered to have benefits in fostering long-term improvement beyond symptom remission, thus reducing vulnerability to new disorder episodes (Shedler, Reference Shedler2010). Practically no convincing empirical evidence exists, however (Leichsenring et al. Reference Leichsenring, Abbass, Luyten, Hilsenroth and Rabung2013). So far a few randomized studies have shown additional improvement during approximately a 1-year follow-up after the end of a course of psychodynamic therapy lasting up to about 40 sessions (Hoglend et al. Reference Hoglend, Bogwald, Amlo, Marble, Ulberg, Cosgrove Sjaastad, Sorbye, Heyerdahl and Johansson2008; Town et al. Reference Town, Diener, Abbass, Leichsenring, Driessen and Rabung2012; Leichsenring et al. Reference Leichsenring, Salzer, Beutel, Herpertz, Hiller, Hoyer, Huesing, Joraschky, Nolting, Poehlmann, Ritter, Stangier, Strauss, Tefikow, Teismann, Willutzki, Wiltink and Leibing2014). Results from long-term courses of therapy that markedly exceed 50 sessions and a duration of 1 year and followed for several years are nevertheless absent.
The Helsinki Psychotherapy Study (HPS) is so far the only trial to compare the effectiveness of individual short-term (6-month) and long-term (3-year) therapy among patients suffering from some depressive or anxiety disorder (Knekt & Lindfors, Reference Knekt and Lindfors2004) during a longer follow-up. So far the effectiveness of short-term solution-focused therapy (SFT), short-term psychodynamic therapy (SPP) and LPP on psychiatric symptoms and work ability (Knekt et al. Reference Knekt, Lindfors, Sares-Jäske, Virtala and Härkänen2013), social functioning (Knekt et al. Reference Knekt, Heinonen, Härkäpää, Järvikoski, Virtala, Rissanen and Lindfors2015), psychological functioning (Lindfors et al. Reference Lindfors, Knekt, Heinonen, Härkänen and Virtala2015) and need for treatment (Knekt et al. Reference Knekt, Lindfors, Renlund, Sares-Jäske, Laaksonen and Virtala2011) has been studied during a 5-year follow-up from the start of therapy. The improvement generally continued after end of the long-term therapy but was also maintained or improved after short-term therapies. Thus the differences in the outcomes between short- and long-term therapies were surprisingly small. Besides the suggestion that part of the effects in the short-term therapy groups may be due to auxiliary treatment, one explanation may be that the follow-up was not long enough to reveal the later improvement caused by the long-term therapy. Thus we need to further test the potential of LPP – based on its greater dosage, length and and specific techniques focused on enhancing mental capacities beyond termination of therapy – in promoting a truly long-term, sustained effect, in comparison with shorter therapies.
The present follow-up stage of the HPS is aimed at giving comparative information concerning the persistence and improvement of the effects of the short- and long-term psychotherapies during a 10-year follow-up from the start of therapy. We hypothesized that LPP would generally be more effective than the short-term therapies and that the short-term therapies would not differ in effectiveness.
Method
Population and study design
Out-patients from psychiatric services in the Helsinki region, 20–46 years of age, and having long-standing (>1 year) depressive or anxiety disorder causing work dysfunction were considered eligible for the HPS (Knekt et al. Reference Knekt, Lindfors, Härkänen, Välikoski, Virtala, Laaksonen, Marttunen, Kaipainen and Renlund2008). Patients with psychotic disorder, severe personality disorder, adjustment disorder, bipolar disorder or substance abuse were excluded. A total of 459 eligible patients were referred to the study between June 1994 and June 2000 (Fig. 1). Of these, 133 did not participate. In a randomized design, the remaining 326 patients were assigned to one of three treatment groups: SFT (n = 97), SPP (n = 101) and LPP (n = 128).
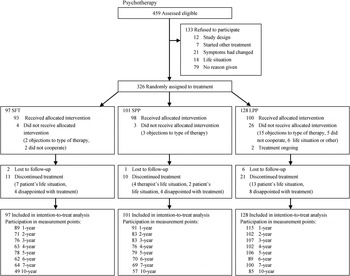
Fig. 1. Flowchart of study. SFT, Solution-focused therapy; SPP, short-term psychodynamic psychotherapy; LPP, long-term psychodynamic psychotherapy.
The study population mainly consisted of women (76%) and the mean age of the patients was 32 (s.d. = 7) years. At baseline 81.6% of the patients suffered from mood disorder, two-thirds from major depressive disorder, and 43.6% from anxiety disorder. A total of 18.1% had personality disorder and 42.9% of the patients had psychiatric co-morbidity (Knekt & Lindfors, Reference Knekt and Lindfors2004).
Patient withdrawal
Of the participants, four who were allocated to SFT, three to SPP and 26 to LPP did not receive the treatment. The main reason for not starting the treatment was the type of therapy allocated. Of the patients starting the assigned therapy, 11 assigned to SFT, 10 to SPP and 21 to LPP discontinued the treatment prematurely. The major reasons for discontinuing the study were the patients’ life situation (e.g. pregnancy, moving to another city or work-related factors) or disappointment with the treatment.
Therapies and therapists
SFT (de Shazer et al. Reference de Shazer, Berg, Lipchik, Nunnally, Molnar, Gingerich and Weiner-Davis1986) included 12 therapy sessions and SPP (Malan, Reference Malan1976) 20 therapy sessions, with both therapies lasting about half a year. The long-term therapy (Gabbard, Reference Gabbard2004) was open-ended, psychodynamic psychotherapy, lasting about 3 years with about 240 sessions. Only SFT, which uses goal- and resource-oriented strategies to facilitate behaviour change by constructing new solutions to the presenting problems, was manualized. The psychodynamic therapies, which in contrast explore developmental issues and have a transference-focused orientation, were conducted in accordance with clinical practice, where the therapists might modify their interventions according to the patient's needs within the respective framework. All the therapists had received standard training and were experienced: The mean duration of work experience was 9 years in the short-term and over 15 years in the long-term therapies. The therapists who provided SFT had received a qualification in SFT provided by a local institute. All the therapists giving psychodynamic psychotherapy (LPP and SPP) had received standard training in psychoanalytically oriented psychotherapy, approved by one of the psychoanalytic or psychodynamic training institutes in Finland. Those giving SPP received an additional 1–2 years training for it. None of the therapists offering psychodynamic psychotherapy had any experience of SFT and vice versa. Therapist characteristics are presented in more detail in Heinonen (Reference Heinonen2014).
Assessments
Psychiatric diagnoses on Axis I (American Psychiatric Association, 1994) were assessed at baseline using a semi-structured interview (Knekt & Lindfors, Reference Knekt and Lindfors2004). The descriptive statistics of the patients were assessed at baseline using questionnaires and interviews.
The outcome measures, covering different measures of psychiatric symptoms, work ability, personality functioning, social functioning, need for psychiatric treatment (auxiliary treatment) and remission were administered prior to the start of treatment and at 13 pre-chosen time points (i.e. at 3, 9, 12, 18, 24, 36, 48, 60, 72, 84, 96, 108 and 120 months) during a 10-year follow-up from start of treatment. In this study we mainly report on the results from the 6th to the 10th year.
The assessment of psychiatric symptoms, work ability, personality functioning and social functioning were based on self-report questionnaires. Psychiatric symptoms were assessed using the Symptom Check List (SCL-90) (Derogatis et al. Reference Derogatis, Lipman and Covi1973). Work ability was assessed using the work subscale (SAS-work) of the Social Adjustment Scale (SAS-SR) (Weissman & Bothwell, Reference Weissman and Bothwell1976) and the question on current employment status was collected by a single item included in a follow-up questionnaire developed in the project. Personality functioning was measured by the self-concept questionnaire of the Structural Analysis of Social Behavior (affiliation and autonomy scales) (Benjamin, Reference Benjamin1996), by the Defense Style Questionnaire (immature, mature) (Andrews et al. Reference Andrews, Pollock and Stewart1989) and the Inventory of Interpersonal Problems (Horowitz et al. Reference Horowitz, Alden, Wiggins and Pincus2000). Social functioning was measured with the SAS-SR (Weissman & Bothwell, Reference Weissman and Bothwell1976) and sense of coherence with the Sense of Coherence Scale (Antonovsky, Reference Antonovsky1993).
Information on the use of psychiatric treatment, i.e. psychotropic medication (antidepressant, anxiolytic, neuroleptic and psychiatric combination medication), additional psychotherapy (individual short-term or long-term, group, couple or family or other) and hospitalization for psychiatric reasons, was continuously assessed during the 10-year follow-up using questionnaires, telephone interviews and nationwide public health registers for all patients randomized (Knekt et al. Reference Knekt, Lindfors, Renlund, Sares-Jäske, Laaksonen and Virtala2011). Remission from psychiatric symptoms (measured by the SCL) in every single point of follow-up was defined using two criteria of symptom change: (1) a 50% reduction of symptoms in comparison with the baseline level; or (2) a measurement value lower than the remission level [i.e. SCL for anxiety symptoms (SCL-90-ANX) < 0.9, SCL for depressive symptoms (SCL-90-DEP) < 0.9 and SCL for general psychiatric symptoms (SCL-90-GSI) < 0.9] (Holi et al. Reference Holi, Marttunen and Aalberg2003), and simultaneously a lack of considerable auxiliary treatment (use of psychotropic medication for at least 6 months, psychotherapy for at least 20 sessions or hospitalization due to psychiatric reason) at the measurement point.
Drop-out from assessments
Of the patients randomized, the participation rate in the assessments was high during the earlier part of the follow-up, being 81% in the 5-year follow-up point, and varying only slightly between therapies (SFT 80, SPP 78, LPP 83%) (Fig. 1). From the sixth follow-up year onwards, the rate decreased, however. The rate was still good in the LPP group (78%) at the 7-year follow-up but only satisfactory in the SFT (66%) and the SPP (68%) groups. At the end of the 10-year follow-up 191 patients participated and the participation rate was only 58% (SFT 51, SPP 56 and LPP 66%).
The assumption of ignorable dropouts (i.e. that dropout does not bias statistical inferences) was studied using information from a nationwide register on the use of psychotropic medication during the entire follow-up separately for those participating and for those who had dropped out. We found that at the 10-year follow-up, participants in the SPP and SFT groups had a suggestively higher prevalence of psychotropic medication use (61 and 49%, respectively) than the non-participants (48 and 33%, respectively). This difference was statistically significant for the short-term groups combined (p = 0.02) (data not shown), indicating that the short-term psychotherapy participants needed more medication than the non-participants from these therapies. Thus the assumption of ignorable drop-out possibly may bias the results of these treatment groups. For this reason we also carried out an imputation using the use of psychotropic medication as an imputation factor.
Reference population
The Health 2011 Survey is based on a representative sample of the adult Finnish population. The sample consists of 7964 individuals, aged 30 years or more. A total of 5806 participated in a health examination of the survey, including assessment by means of the SCL-25 questionnaire (Koskinen et al. Reference Koskinen, Lundqvist and Ristiluoma2012). Of these participants, 447 were from the Helsinki area and were aged 30–56 years. This subsample was used as the reference population in the present study with the aim to see how close the patient sample comes to the normal population 10 years after start of therapy. The SCL-25 scale varied from 0 to 3, and values >0.75 were regarded as elevated, giving 5 and 11% elevated values for the anxiety and depression symptoms, respectively.
Statistical analyses
The effectiveness of the three therapies was studied in a design with repeated measurements of the outcome variables primarily as ‘intention-to-treat’ (ITT) analyses including all the 326 patients randomized (Härkänen et al. Reference Härkänen, Knekt, Virtala and Lindfors2005, Reference Härkänen, Arjas, Laaksonen, Lindfors, Haukka and Knekt2013; Knekt et al. Reference Knekt, Lindfors, Härkänen, Välikoski, Virtala, Laaksonen, Marttunen, Kaipainen and Renlund2008). Complementary ‘as-treated’ (AT) analyses were performed taking into account violation of the treatment standards. The primary analyses were based on the assumption of ignorable dropouts of assessments at the measurement points, and in secondary analyses, missing values were replaced by multiple imputation (Rubin, Reference Rubin1987). Since no notable differences were seen between the original and imputed models (data not shown), the results from the original models are reported.
Linear mixed models were used for continuous outcome variables (Verbeke & Molenberghs, Reference Verbeke and Molenberghs1997) and logistic regression models for binary responses (Liang & Zeger, Reference Liang and Zeger1986). Two effect size measures were calculated for the different time points: model-adjusted mean differences using predictive margins (Lee, Reference Lee1981; Graubard & Korn, Reference Graubard and Korn1999) and relative risks. The delta method was used for calculating confidence intervals (Migon & Gamerman, Reference Migon and Gamerman1999). Statistical significance was tested using the Wald test.
The basic ITT model included the main effects of follow-up time, treatment group, the difference between theoretical and realized date of measurement, and first-order interaction of time and treatment group. A completed model further adjusted for the baseline level of each outcome measure. The single outcome variables from the domains of psychiatric symptoms, work ability, psychological functioning, social functioning, need for psychiatric treatment and remission were analysed in separate models. The complementary AT analyses were performed by further including variables describing compliance as baseline variables (waiting time from randomization to initiation of treatment and withdrawal before start of treatment) and as time-dependent covariates (discontinuation of the study treatment and use of auxiliary treatment during follow-up) as main effects in the ITT models.
The statistical analyses were performed using SAS software 9.3 (SAS Institute Inc., 2011).
Results
Symptoms, work ability, personality and social functioning
Psychiatric symptoms, work ability, and personality and social functioning measures at baseline and at the 6-, 7- and 10-year follow-ups from the ITT analyses are presented in Table 1. A statistically significant change from baseline to the end of the follow-up was seen in all measures and in all therapy groups.
Table 1. Effectiveness of short- and long-term psychotherapy on psychiatric symptoms, work ability, and psychological and social functioning during a 10-year follow-up

SFT, Solution-focused therapy; SPP, short-term psychodynamic psychotherapy; LPP, long-term psychodynamic psychotherapy; s.e., standard error; SCL-90-GSI, Symptom Check List for general psychiatric symptoms; SCL-90-DEP, Symptom Check List for depressive symptoms; SCL-90-ANX, Symptom Check List for anxiety symptoms; SAS-SR, Social Adjustment Scale; DSQ, Defense Style Questionnaire; SASB, Structural Analysis of Social Behavior; IIP, Inventory of Interpersonal Problems; SOC, Sense of Coherence Scale.
a The intention-to-treat model.
* A statistically significant change occurred between two consecutive follow-up points (p < 0.05).
† Differed statistically significantly from the LPP group in a model further adjusted for baseline of respective outcome variable (p < 0.05).
The change in the three psychiatric symptom measures varied from 38.1% to 43.7%, from 53.2% to 57.0%, and from 42.7% to 49.2% for the SPP, LPP and SFT groups, respectively. A significant reduction from the 6-year to the 7-year follow-up point was seen in LPP. General psychiatric symptoms (SCL-90-GSI) and depressive symptoms (SCL-90-DEP) were significantly more effectively reduced in the LPP group than in the SPP group at the end of the follow-up. A similar greater reduction in general psychiatric symptoms and anxiety symptoms (SCL-90-GSI and -ANX) was seen in the AT analyses in comparison with the SFT group (online Supplementary Appendix S1.1).
Work ability (SAS-work) was at the 10-year follow-up significantly more improved in the LPP than in the SPP group in the ITT analyses and also more improved than SFT in the AT analyses (online Supplementary Appendix S1.2). Employment percentage was not significantly improved during the follow-up in any therapy group and, accordingly, no differences between the groups were seen.
No significant differences between the therapy groups benefiting from LPP in comparison with short-term therapy were seen for personality or social functioning in the ITT analyses, though SAS-SR was more improved at the end of the follow-up in LPP than in SPP or SFT in the AT analyses (online Supplementary Appendices S1.3–S1.4).
Population comparison of symptoms
Comparisons of clinically elevated anxiety symptoms and depressive symptoms of the patients aged 20–46 years at baseline and 10 years later with those of a representative sample of individuals aged 30–56 years in the Helsinki area showed that at baseline 87% of the patients suffered from depressive and 55% from anxiety symptoms. After 10 years the corresponding values were 42 and 20%. Since these post-treatment prevalences of depressive and anxiety symptoms in the study population were 4-fold in comparison with those of the reference population (11 and 5%) (p < 0.001), the treatments given by the HPS, in combination with the auxiliary treatment taken by the patients themselves, completely reduced symptoms in only a proportion of the treatment-receiving cohort.
Need for psychiatric treatment (auxiliary treatment)
Prevalence of auxiliary treatment during the follow-up
At baseline, one of five patients used psychotropic medication, whereas, due to the exclusion criteria, none of the patients used psychotherapy or were hospitalized (data not shown). During the treatment period and later during the entire follow-up the use of auxiliary treatment (mainly psychotropic medication and auxiliary therapy) was considerable, varying for the total sample by year from 40.7 to 48.5%. More auxiliary treatment was used in the short-term therapy groups than in the LPP group from the third year to the end of the follow-up, with relative risks varying from 1.28 to 2.00 (Fig. 2 a). During the first years of follow-up the short-term groups used more auxiliary therapy whereas the differences between the treatment groups were smaller at the end of follow-up (Fig. 2 b). Use of psychotropic medication rose during the follow-up in the short-term groups, during the first half in SPP and later in SFT being at the same level at the end of follow-up (Fig. 2 c).
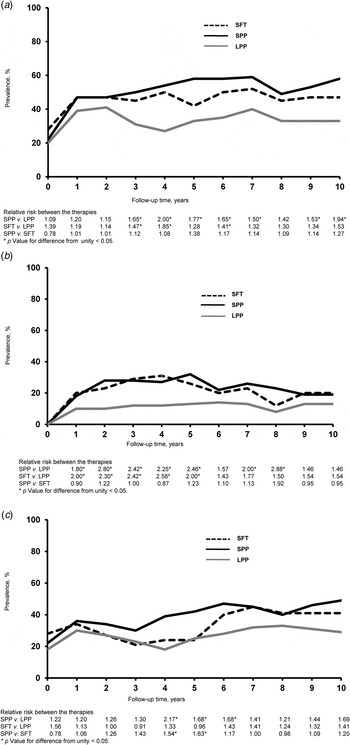
Fig. 2. (a) Prevalence of auxiliary psychiatric treatment during follow-up. (b) Prevalence of auxiliary psychotherapy during follow-up. (c) Prevalence of psychotropic medication during follow-up. SFT, Solution-focused therapy; SPP, short-term psychodynamic psychotherapy; LPP, long-term psychodynamic psychotherapy.
Need for treatment and use of auxiliary treatment at end of follow-up
At the 10-year follow-up, 44% of the 191 participants used some auxiliary treatment. Although these patients showed considerably fewer symptoms than at baseline, they suffered statistically significantly from more psychiatric symptoms (30–46%) than those not using auxiliary treatment. No significant differences between treatment groups were seen. Of these patients, 59% used medication only, 24% used both medication and psychotherapy, and 13% psychotherapy only (Table 2). The prevalence of auxiliary treatment use differed significantly between the treatment groups (p = 0.01), being 58% in the SPP group, 47% in the SFT group and 33% in the LPP group. The higher prevalence of auxiliary treatment in the SPP group was mainly due to the higher prevalence of psychiatric medication use, which was 41, 49 and 29% in the SFT, SPP and LPP groups, respectively.
Table 2. Patients using auxiliary treatment 10 years after start of therapy by treatment profile

Data are given as percentage of patients (number of patients).
SFT, Solution-focused therapy; SPP, short-term psychodynamic psychotherapy; LPP, long-term psychodynamic psychotherapy.
a Distribution by type of treatment.
b p Value for difference between therapy groups.
Cumulative use of therapy at the end of follow-up
Study of the cumulative auxiliary use of therapy during the entire follow-up showed 35% more therapy users in the short-term groups (p = 0.04) (Table 3). The median number of sessions was more than three-fold in individuals from these groups in comparison with those of the LPP group (p < 0.001). These differences were mainly due to the individual therapies (short- and long-term). The additional long-term therapies lasted for a much shorter time in the long-term therapy group; the median length was 192, 142 and 60 sessions in the SFT, SPP and LPP groups, respectively. In the total study sample of 326 patients the overall mean number of auxiliary therapy sessions were 86 (s.d. = 159, maximum = 613) in SFT, 93 (s.d. = 172, maximum = 1055) in SPP and 21 (s.d. = 48, maximum = 276) in LPP.
Table 3. Cumulative prevalence and number of sessions of auxiliary therapy during the 10-year follow-up

SFT, Solution-focused therapy; SPP, short-term psychodynamic psychotherapy; LPP, long-term psychodynamic psychotherapy; N, number of patients at risk (N = 296) after exclusion of those with missing data (N = 30); n, number of patients receiving therapy (n = 147), based on which the mean (median) sessions are estimated after exclusion of those with missing data (n = 3).
a p Value for difference between therapy groups.
b A number of patients used several forms of different auxiliary therapy.
Remission
Remission showed similar, but stronger, associations than changes in the psychiatric symptoms (Table 4, online Supplementary Appendix S2). A statistically significant rate of remission occurred during the 10-year follow-up in comparison with the baseline values for all three indicators in all therapy groups with the exception of remission from anxiety in the SPP group. Remission was more effectively reached for all three measures in the LPP group than in the SPP group at the 7- or 10-year follow-up. The remission rates at the 10-year follow-up point for SCL-90-GSI were 0.55, 0.45 and 0.62 in the SFT, SPP and LPP groups, respectively. The individuals in remission (52%) showed a mean SCL-90-GSI value of 0.37 for all therapy groups combined (Table 5). A study of individuals with extended remission (22%), i.e. patients otherwise satisfying the SCL-90-GSI remission criteria but receiving auxiliary treatment, showed a similar mean SCL-90-GSI value of 0.44. Combining these two groups showed a prevalence of global remission, with or without the use of auxiliary treatment, of 69, 67 and 81% for SFT, SPP and LPP, respectively. The remaining 26% of individuals still suffered from psychiatric symptoms, with a mean SCL-90-GSI of 1.47.
Table 4. Remission (%) by therapy group and year of follow-up

SFT, Solution-focused therapy; SPP, short-term psychodynamic psychotherapy; LPP, long-term psychodynamic psychotherapy; s.e., standard error; SCL-90-GSI, Symptom Check List for general psychiatric symptoms; SCL-90-DEP, Symptom Check List for depressive symptoms; SCL-90-ANX, Symptom Check List for anxiety symptoms.
a The remission variables were based on respective symptom variables, SCL-90-GSI, SCL-90-DEP and SCL-90-ANX, and use of considerable auxiliary treatment.
b The intention-to-treat model.
* Statistically significantly lesser improvement than in the LPP group, based on a model further adjusted for baseline of respective outcome variable (p < 0.05).
Table 5. Crude means of symptom measures by global remission and considerable auxiliary treatment at the 10-year follow-up point

SCL-90-GSI, Symptom Check List for general psychiatric symptoms; SCL-90-ANX, Symptom Check List for anxiety symptoms; SCL-90-DEP, Symptom Check List for depressive symptoms; s.d., standard deviation; SFT, solution-focused therapy; SPP, short-term psychodynamic psychotherapy; LPP, long-term psychodynamic psychotherapy.
a Global remission was defined as a 50% reduction of symptoms in comparison with the baseline level or a measurement value lower than the remission level (i.e. SCL-90-ANX < 0.9, SCL-DEP < 0.9 and SCL-GSI < 0.9, respectively).
b Use of psychotropic medication for at least 6 months, psychotherapy for at least 20 sessions or hospitalization due to psychiatric reason.
Discussion
Overall considerations
The treatments given by the HPS in combination with spontaneous use of psychotropic medication or auxiliary therapy significantly reduced symptoms and improved psychological functions and social functioning, which are effects that lasted for the entire 10-year follow-up. The treatments were nevertheless insufficient for many participants of the present study. At 10 years after the start of treatment only about 55% of the individuals were in remission and 40% of the individuals still used some form of psychiatric treatment. Furthermore, the prevalence of patients with elevated psychiatric symptom values was 4-fold in comparison with those of the total population. These findings suggest that the treatments given during this long period were not particularly effective in providing long-term benefits for most of the patients. Although the findings are in line with those of studies on depressive and complex anxiety disorder that were based on a follow-up of several years after termination of therapy (Perry & Bond, Reference Perry and Bond2009; Huber et al. Reference Huber, Zimmermann, Henrich and Klug2012), and in line with population-based studies on the long-term course of depression and anxiety in the general population (Rhebergen et al. Reference Rhebergen, Batelaan, de Graaf, Nolen, Spijker, Beekman and Penninx2011; Steinert et al. Reference Steinert, Hofmann, Kruse and Leichsenring2014), they may be considered unsatisfactory. One possible reason may be the fact that the disorders were relatively chronic at the start of treatment, given the inclusion criteria used, which selected for long-standing depressive or anxiety disorders with realized work dysfunction.
The fact that among patients using auxiliary treatment at the 10-year follow-up about 85% preferred medication and less than 15% solely auxiliary psychotherapy seems to reflect the fact that medication is more readily available and used in health care in an attempt to regulate mood and anxiety symptoms. It may also be a sign of persistent distress despite the use of psychotherapy (Bond & Perry, Reference Bond and Perry2006), and thus reflect dissatisfaction with the psychotherapy given. Alternatively, it may be a sign of a lower level of psychological suffering due to less complicated intrapsychic or interpersonal problems and/or symptoms and thus a lack of interest for time- and money-consuming therapies.
We found a lack of global remission for 19% of the patients receiving LPP and for 31% and 33% for those receiving SFT and SPP, respectively. Thus, in the event that all the 198 individuals allocated to the short-term therapy groups would have received LPP, it seems about 25 of those not remitted would have achieved remission. To be able to optimally allocate patients to therapy in the future, more suitability studies detecting patient factors predicting the outcome of short-term v. long-term psychotherapy before start of therapy (Laaksonen et al. Reference Laaksonen, Knekt and Lindfors2013) are needed. Thus, with the help of information on such patient factors in choice of therapy, the risk of referring the patient either to an insuffiently short treatment or to an unnecessarily long therapy could be reduced. Furthermore, to minimize complications for the patients, effectiveness studies should therefore more often be of naturalistic design, and trials allocating subjects to potentially inappropriate treatments should be avoided.
LPP gave a better outcome
We found significant, extended, symptom reduction in LPP 4 years after end of therapy, while at the end of the follow-up, depressive symptoms were slightly more reduced, work ability slightly more improved, and the remission rate somewhat higher in patients in the LPP than in the SPP group. Moreover, the prevalence of auxiliary treatment – both use of therapy and psychotropic medication – was much higher in the short-term therapy groups through the follow-up, suggesting LPP gives a better outcome. It has been suggested that changes in personality structure and functioning are specific treatment targets in LPP (Shedler, Reference Shedler2010). Recent meta-analyses on LPP across different types of patient groups have, depending on the inclusion criteria of the selected studies, either shown no specific effects of LPP on personality functioning or somewhat greater effects than for shorter therapies (Smit et al. Reference Smit, Huibers, Ioannidis, van Dyck, van Tilburg and Arntz2012; Leichsenring et al. Reference Leichsenring, Abbass, Luyten, Hilsenroth and Rabung2013). Accordingly, we found LPP to be more effective than the short-term therapies in this outcome domain during a 5-year follow-up from the start of therapy (Lindfors et al. Reference Lindfors, Knekt, Heinonen, Härkänen and Virtala2015). However, no benefits in the effectiveness prevailed throughout the 10-year follow-up in comparison with short-term therapies in any of the measures. Thus, although unknown aspects of personality-related changes may be involved in the attainment of more improved work ability and symptomatic status, these results suggest that the long-term benefits of LPP are not specifically indicated by greater effects in personality functioning. In fact, a single finding suggested that there was more increase in autonomy in SFT than in LPP at the final 10-year follow-up, although this was not supported by the AT analyses.
The patients in the short-term therapy groups started new therapies more often than those in the LPP group. At the end of the follow-up, the median cumulative number of auxiliary therapy sessions over the follow-up was 3-fold and the therapy was more often long-term in the short-term therapy groups in comparison with the LPP group. These extra therapies may have been taken because the short-term therapies have been experienced as unsatisfactory. It is also possible that the short-term therapy, although insufficient in providing recovery, did adequately function as a preparatory treatment for developing the patients’ better understanding of their problems, and may have built motivation and trust in a psychotherapeutic process, and accordingly paving the way to continued treatment. The relatively low number of auxiliary therapy sessions through the follow-up suggests that no considerable need for therapy persisted after the end of the long-term study therapy. The auxiliary therapies in the long-term group were much shorter, possibly because they mostly completed the study therapy given. Alternatively, this may be due to the fact that the community (Social Insurance Institution, 2012) requires for its support a waiting period of 5 years between two long-term therapies. One apparent contributory reason for this need for therapy in the short-term therapy groups may be that the randomization of patients hindered selection of patients based on their suitability for short-term therapy (Laaksonen et al. Reference Laaksonen, Lindfors, Knekt and Aalberg2012).
Also the fact that the prevalence of psychotropic medication was doubled during the follow-up in the short-term therapy groups, being two-fold at the end of follow-up in comparison with that of the LPP group, suggests that the short-term therapies have been less effective. Of these reasons our conclusion is that those randomized to the long-term therapy group overall had a better prognosis than those allocated to the short-term therapies.
No major differences in effectiveness between the two short-term therapies
Although the effects in the outcome measures or the use of auxiliary therapy between the two short-term therapies did not differ, the use of psychotropic medication in the SPP group was considerably higher during the first 5 years of follow-up than in the SFT group. Later, no differences were seen, suggesting that the possible intervention effect lasted for a longer time in the SFT group. We hypothesize that this difference may reflect the stronger reality orientation of SFT v. SPP. Further, the psychologically more demanding and interpretative technique of SPP may not have been sufficiently worked through in the short 20 session time-frame for some patients.
What is an optimal length of therapy?
As stated, mainly small differences were seen in the outcome measures between short-term therapy and LPP. Thus, on average, about 100–120 sessions (12 in SFT and 20 in SPP plus 85–95 auxiliary sessions) plus excess use of psychotropic medication gave an effectiveness almost comparable with that of 240–260 sessions of LPP. Our speculative suggestion is thus that for some patients, the dosage and length of the LPP could be reduced or replaced by shorter types of therapies, prescribing an additional maintenance or continuation type of therapy of low intensity and duration (Vittengl et al. Reference Vittengl, Clark and Jarrett2009), or a combination treatment, thus giving better cost-effectiveness. In line with that speculation, a recent study based on the register data of the Finnish Social Insurance Institution indicated that at present approximately only one-third of long-term therapies subsidized by the Finnish Social Insurance Institution have a duration of up to the maximum of 3 years (Tuulio-Henriksson et al. Reference Tuulio-Henriksson, Heino, Toikka and Autti-Rämö2014); however, it is not known how well this reflects patients’ true treatment needs or the match between patient characteristics and treatment length. On the other hand, our finding that patients in both short-term therapy groups on average needed about 85–95 auxiliary sessions suggests that the number of study sessions (12 in SFT and 20 in SPP) was unsatisfactory for some patients. Moreover, the fact that the majority of the patients receiving short-term therapy and needing auxiliary individual therapy continued with long-term therapy suggests that short-term therapy was experienced as unsatisfactory. These results also highlight the need to closely monitor patient progress and to flexibly respond to individual treatment needs.
Methodological considerations
Advantages of this randomized clinical trial that compares the effectiveness of short- and long-term psychotherapy are the exceptionally long follow-up, with 15 repeated measurements of the outcome variables during a 10-year follow-up. The inclusion of information about the use of auxiliary treatment during the entire follow-up is of importance as it gave the possibility to evaluate the net remission from psychiatric symptoms.
An unavoidable general weakness in the study is that measuring efficacy (the pure effects of the therapies) is not possible for ethical reasons; the lack of manuals for the psychodynamic therapies used, the lack of a control group, and the lack of blindness of assessments were further limitations (Knekt et al. Reference Knekt, Lindfors, Sares-Jäske, Virtala and Härkänen2013). Moreover, the effect of short-term therapies may have been underestimated for two reasons. First, the participation rate was relatively low (about 60%) at the final measurement point, accompanied by a significant drop-out rate. Since the participants belonging to the short-term therapy group appeared to need more treatment than those not participating in the measurement, the therapy effect may be underestimated in those groups. However, the imputed results did not support that suggestion. Furthermore, the differences between the therapies in favour of the long-term therapy lasted for a longer period, covering a period where drop-outs were less significant. Second, due to the randomization, the suitability of the therapies studied was not taken into account when allocating the therapies. The effects in the short-term therapy groups may therefore have been underestimated, as the expected sufficiency of the short-term therapy, based on the patients’ ego strength, self-observing capacity, and nature of problems, was not acknowledged (Laaksonen et al. Reference Laaksonen, Lindfors, Knekt and Aalberg2012). However, motivation, curiosity towards their inner life, and other psychological characteristics, considered beneficial for a lengthy, intensive process in LPP (Wilczek et al. Reference Wilczek, Weinryb, Gustavsson, Barber, Schubert and Asberg1997) may also have been less than optimal in the patients randomized to it.
Summary
This study suggests that LPP is more effective than short-term therapy, although none of the therapies alone guarantees remission. The incomplete effect of the therapies can be compensated by additive therapy and/or use of psychotropic medication, suggesting especially short-term therapy to be an unsatisfactory form of treatment for some of the patients. The fact that short-term therapy in combination with auxiliary treatment gives as nearly a good result as full long-term therapy suggests that the length of long-term therapy could be shorter than the 3-year therapy or the overall dosage could be lower than the approximately 240 sessions given for some patients. In conclusion, to obtain deeper insights into whether to use long- or short-term psychotherapy or some other treatment, suitability factors for the optimal use of short- and long-term psychotherapy should be detected and the effectiveness of therapies of different lengths should be studied in association with those factors identified. Thus a considerable amount of scientific work is still needed in this important area.
Supplementary material
For supplementary material accompanying this paper visit http://dx.doi.org/10.1017/S0033291715002718.
Acknowledgements
The present study was financially supported by the Academy of Finland (grant no. 138876).
Declaration of Interest
None.









