Introduction
Rationale
Tonsillectomy is one of the most commonly performed ENT operations. The procedure was described as early as the first century.Reference Younis and Lazar1,Reference Lowe, van der Meulen, Cromwell, Lewsey, Copley and Browne2 For children, the two main indications for tonsillectomy are obstructive sleep apnoea and recurrent tonsillitis.Reference Barraclough and Anari3,Reference Greig4 The criteria of current guidelines assess the disease impact on function, child development and quality of life, in order to determine benefit from tonsillectomy.Reference Barraclough and Anari3,Reference Windfuhr5 Tonsillectomy may also be required following peritonsillar abscess.
A number of techniques may be used to remove the tonsils. However, there is currently no consensus on the ‘gold standard’, with each technique having its own advantages and disadvantages. Previous evidence showed that the most popular tonsillectomy technique is cold dissection.Reference Lowe, van der Meulen, Cromwell, Lewsey, Copley and Browne2 This involves separation of the tonsil and the associated capsule from the surrounding tissue with blunt and sharp dissection; bipolar diathermy is then used for haemostasis. The second most popular choice is bipolar diathermy, used for both haemostasis and dissection.Reference Lowe, van der Meulen, Cromwell, Lewsey, Copley and Browne2 Other techniques are also commonly used; these include coblation tonsillectomy, laser dissection, monopolar electrosurgery and use of the Harmonic® scalpel.Reference Lowe, van der Meulen, Cromwell, Lewsey, Copley and Browne2
There are a few risks and complications associated with tonsillectomy that a child's parent or legal guardian must be made aware of. Pain is often mentioned as a risk. Pain always occurs to some extent with tonsillectomy, but the level will vary between patients.Reference Husband and Davis6 The most common risks associated with this procedure are haemorrhage, infection and dental injury.Reference Greig4 Haemorrhage is occasionally a very serious and potentially life-threatening complication. Haemorrhage is classified depending on the time it occurs in relation to the operation.Reference Lowe, van der Meulen, Cromwell, Lewsey, Copley and Browne2 According to the National Prospective Tonsillectomy Audit, the rate of primary haemorrhage is around 1 in 170, and that of secondary haemorrhage is 1 in 33, with the lowest incidence of secondary haemorrhage occurring in procedures performed via cold dissection.Reference Lowe, van der Meulen, Cromwell, Lewsey, Copley and Browne2
Coblation tonsillectomy is a more recent technique that uses a conduction medium to produce a plasma field with radiofrequency energy, causing ablation, to dissect tissue. The major advantage of this technique is that the charge has sufficient energy to cause disintegration of tissues at lower temperatures compared to other electrosurgery techniques. This causes less thermal damage, which may contribute to less post-operative pain; however, it may contribute to an increased risk of haemorrhage when compared to cold dissection.Reference Blanchford and Lowe7
Objective
This study evaluated the peri-operative outcomes in paediatric tonsillectomy patients by comparing coblation and cold dissection techniques.
Materials and methods
Types of studies
All randomised studies reporting on the peri-operative outcomes of coblation tonsillectomy and cold dissection tonsillectomy techniques were identified. There was no language restriction. Only paediatric studies were considered for inclusion (Table 1). All animal studies were excluded. Articles that only assessed the use of coblation tonsillectomy or cold dissection tonsillectomy, or did not use both coblation tonsillectomy and cold dissection tonsillectomy, were excluded. Studies that included adult patients were also excluded.
Table 1. Inclusion criteria for systematic review

Types of participants
Articles that included paediatric patients (aged under 16 years), male or female, of any ethnic background, with no regional restriction, who underwent tonsillectomy by either coblation technique or cold dissection technique, were studied.
Hypotheses and outcome measures
The primary hypothesis was that there would be no significant difference between the peri-operative outcomes of coblation and cold dissection tonsillectomy techniques in paediatric patients. The primary outcome measure was pain; the secondary outcomes were haemorrhage rates and operative time. The results are presented using forest plots and risk ratios.
Information sources
The studies reviewed compared the two aforementioned tonsillectomy techniques. Searches were made using the Medline, Embase, and Cumulative Index to Nursing and Allied Health Literature (‘CINAHL’) databases, all available through the National Health Service National electronic Library for Health website, as well as the Cochrane Library and the PubMed search engine, both available online. The search included all articles dated up to December 2018. The last search was performed on 31 December 2018. There was no language restriction in place and articles in other languages were translated if required.
Searches
Text words were used in combination with Medical Subject Heading terms. The following search terms were used: ‘tonsillectomy’, ‘tonsil surgery’, ‘tonsillar surgery’, ‘tonsil removal’, ‘tonsils removal’, ‘tonsillar removal’, ‘tonsil surgical removal’, ‘tonsils surgical removal’, ‘tonsillar surgical removal’, ‘tonsil dissection’, ‘tonsils dissection’, ‘tonsillar dissection’, ‘tonsil resection’, ‘tonsils resection’ or ‘tonsillar resection’, together with ‘coblation’, ‘normal’, ‘standard’, ‘cold steel’, ‘cold knife’, ‘cautery’, ‘electrocautery’, ‘bipolar’, ‘radiofrequency’, ‘bipolar radiofrequency’, ‘ultrasound’, ‘ultrasonic’, ‘powered’, ‘intracapsular’, ‘powered intracapsular’, ‘harmonic’, ‘thermal’, ‘welding’, ‘thermal welding’, ‘laser’, ‘laser ablation’, ‘transoral laser ablation’, ‘transoral laser’, ‘tolr’, ‘transoral laser resection’ or ‘microdebrider’.
Articles relating to other tonsillectomy techniques, any other tonsil-related technique or procedure, irrelevant articles, reviews or meta-analyses, as evident from the titles and abstracts, were not included; however, any relevant articles referenced in these publications were obtained and the references of identified studies were searched to identify any further studies.
A flow chart of the literature search according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (‘PRISMA’) guidelines is shown in Figure 1.Reference Moher, Liberati and Tetzlaff8

Fig. 1. Preferred Reporting Items for Systematic Reviews and Meta-Analyses (‘PRISMA’) flow chart diagram, showing search results of included articles after exclusions.
Study selection and data collection process
Each article conforming to the inclusion criteria (Table 1) was examined. This review was performed independently. When more specific data or missing data were required, the authors of the manuscripts were contacted; however, no responses were received to these requests. Data were entered onto a worksheet ready for analysis.
Data items
Patient demographics and study characteristics were extracted from the studies. The study characteristics extracted were: year, country of origin and tonsillectomy technique. Patient demographics included: total number of patients, along with gender and age (mean age and range) where available. Two authors (MUA and ANW) independently collected the data, before it was compared. Any discrepancies in the collected data were to be reviewed by a different author; however, this did not occur.
Risk of bias and quality assessment
The methodological quality of the trials included for meta-analysis was formally assessed using the Cochrane risk of bias tool.Reference Higgins, Altman, Gotzsche, Juni, Moher and Oxman9,Reference Higgins, Thomas, Chandler, Cumpston, Li and Page10 Assessment was performed by two authors (MUA and ANW) independently.
Summary measures and data synthesis for summative and comparative meta-analyses
Statistical analyses were performed using Review Manager 5.3 computer software.11 The study was undertaken in accordance with reported guidance for outcome meta-analyses. In the case of a 0 event, where no events occurred for the specified parameter, 0.5 was added to each cell frequency by the statistical software, as reported by Higgins et al.Reference Higgins, Thomas, Chandler, Cumpston, Li and Page10 In the studies examined, the gold standard was set as cold dissection tonsillectomy.
The data collected for operative time and intra-operative blood loss outcomes were continuous data; therefore, the inverse variance statistical method was applied and the effect measure was presented as a standardised mean difference. The data collected for primary and secondary haemorrhage rates were event data and therefore discrete data; the Mantel–Haenszel statistical method was thus applied and the effect measure given as a risk ratio.
Heterogeneity between studies was assessed using Cochran's Q statistic, which is a type of chi-square test. There was clinical heterogeneity between the studies; therefore, all statistical tests were completed using the random effects model.
Publication bias
There is likely to be inherent publication bias, although this was not formally tested given the low number of studies.
Funding
There are no funding declarations related to this study.
Results
Study selection
A total of 4430 records were identified through database searching (Figure 1). The electronic databases searched (Medline, Cochrane, Embase) yielded 3999 citations, and 431 citations were identified through bibliographies and conference proceedings. After the removal of duplicates, 3957 unique records remained. Records were excluded if they were deemed irrelevant or unrelated to the comparison of coblation and cold dissection techniques in paediatric tonsillectomy. A total of 34 studies were then reviewed for eligibility, after which 24 were excluded. Of the 24 studies excluded, 3 of these studies may have been considered relevant, but could not be included as the data were inaccessible (being in Chinese) or the article was not available.Reference Wang, Dong, Liang, Fu, Jiang and Chen12–Reference Wang, Yang and Yang14
The remaining studies were used for quantitative analysis. The studies were chosen based on the inclusion criteria (Table 1). There were no data or studies from any unpublished or grey literature. A total of seven studies were included in the summative outcome for meta-analysis.Reference Elbadawey, Hegazy, Eltahan and Powell15–Reference Shapiro and Bhattacharyya21
Study types
All study characteristics are shown in Table 2. All seven studies were published in English. Four studies came from Asia, whilst two studies came from Europe and one study from the USA.
Table 2. Study characteristics

Participants
A total of 635 patients were included in this review of summative outcomes. Of these paediatric patients, 318 underwent coblation tonsillectomy and 317 underwent cold dissection tonsillectomy. The patient data for each treatment group are shown in Table 3. The analyses used are described in the section ‘Summary measures, and data synthesis for summative and comparative meta-analyses’ above.
Table 3. Characteristics of patients from selected studies

Quality assessment
The studies were assessed using the Cochrane risk of bias tool (Table 4).Reference Higgins, Altman, Gotzsche, Juni, Moher and Oxman9,Reference Higgins, Thomas, Chandler, Cumpston, Li and Page10
Table 4. Methodological qualities of studies according to Cochrane risk of bias toolReference Higgins, Altman, Gotzsche, Juni, Moher and Oxman9,Reference Higgins, Thomas, Chandler, Cumpston, Li and Page10

‘+’ = low risk of bias; ‘−’ = high risk of bias; ‘?’ = undetermined risk of bias
Quantitative synthesis of peak pain score
This outcome was recorded in the studies in two different ways, using either the visual analogue score or Wong-Baker Faces® score. The highest pain score given was the measurement used. Only data that were given as part of the Wong-Baker Faces pain score were assessed, as this has been validated in children.Reference Garra, Singer, Domingo and Thode22,Reference Garra, Singer, Taira, Chohan, Cardoz and Chisena23 The study authors reported the results in different ways. Wong-Baker should be reported as discrete data, but some authors attempted to use means for data. Given the lack of consistency in reporting and the low number of studies reporting this outcome, a statistical test was not attempted for this outcome and the data are not reported. However, from the two studies which reported the outcome, both showed that coblation resulted in less pain than cold dissection.Reference Elbadawey, Hegazy, Eltahan and Powell15,Reference Paramasivan, Arumugam and Kameswaran19 The issues surrounding this are discussed further in the section ‘Study limitations and heterogeneity’ below.
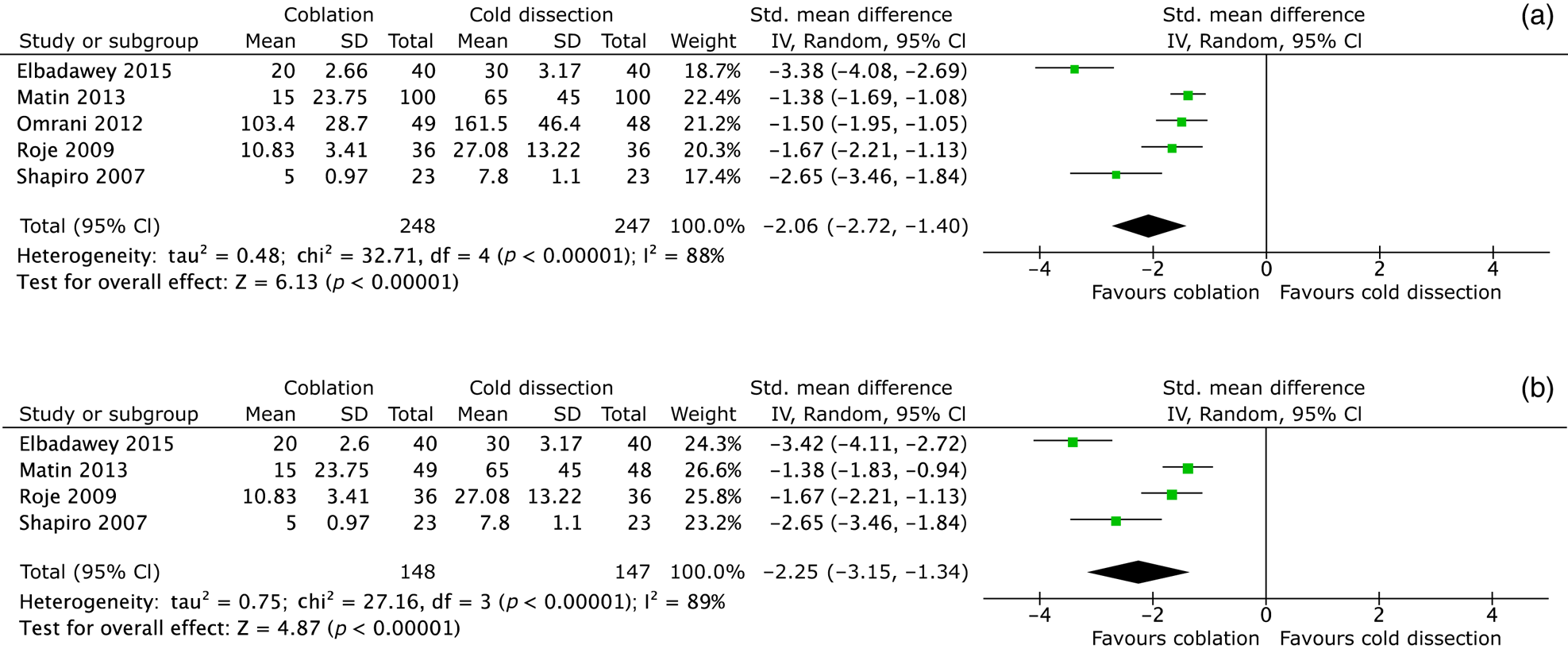
Quantitative synthesis of intra-operative blood loss
Five studies with 495 patients contributed data to the meta-analysis (Tables 5 and 6). Coblation showed a −2.06 (p < 0.00001; 95 per cent confidence interval (CI) = −2.72 to −1.40) standardised mean difference in intra-operative blood loss when compared to cold dissection tonsillectomy. This is shown in the forest plot in Figure 2a. There was evidence of significant heterogeneity between the studies (tau-square = 0.48, chi-square = 32.7, 4 degrees of freedom, p < 0.00001; I2 = 88). However, one study showed what appeared to be an anomalous result, very different to the other studies; therefore, a second analysis was conducted with this study removed.

Fig. 2. (a) Forest plot to demonstrate standardised mean difference of intra-operative blood loss between coblation and cold dissection tonsillectomy; and (b) modified forest plot to demonstrate standardised mean difference of intra-operative blood loss between coblation and cold dissection tonsillectomy after perceived anomaly removed. Std. = standard; SD = standard deviation; IV = inverse variance; CI = confidence interval; df = degrees of freedom
Table 5. Study results for coblation group

All results were given a quantitative continuous number except peak pain score, operative time and intra-operative haemorrhage. * Wong-Baker Faces score; data were omitted in light of the poor application of science and statistics for the pain score values reported. SD = standard deviation
Table 6. Study results for cold dissection group

All results were given a number except peak pain score, operative time and intra-operative haemorrhage. *Wong-Baker Faces score; data were omitted in light of the poor application of science and statistics for the pain score values reported. SD = standard deviation
Four studies with 295 patients contributed to the modified meta-analysis, as shown in Figure 2b. Coblation showed a −2.25 (p < 0.00001; 95 per cent CI = −3.15 to −1.34) standardised mean difference in this analysis; however, there was still significant evidence of heterogeneity (tau-square = 0.75, chi-square = 27.16, 3 degrees of freedom, p < 0.00001; I2 = 89).
Quantitative synthesis of operative time
Four studies with 423 patients contributed data to the meta-analysis (Tables 5 and 6). Coblation showed a −2.67 (p = 0.0001; 95 per cent CI = −4.03 to −1.31) standardised mean difference in operative time when compared to cold dissection tonsillectomy. This is shown in the forest plot in Figure 3. There was evidence of significant heterogeneity between the studies (tau-square = 1.81, chi-square = 75.52, 3 degrees of freedom, p < 0.00001; I2 = 96).

Fig. 3. Forest plot to demonstrate standardised mean difference of operative time between coblation and cold dissection tonsillectomy. Std. = standard; SD = standard deviation; IV = inverse variance; CI = confidence interval; df = degrees of freedom
Quantitative synthesis of primary haemorrhage
Seven studies with 635 patients contributed data to the meta-analysis, with 2 studies showing events of primary haemorrhage (Tables 5 and 6). Coblation showed a 0.66 (p = 0.65; 95 per cent CI = 0.11 to 3.99) relative risk for primary haemorrhage events when compared to cold dissection tonsillectomy. This is shown in the forest plot in Figure 4. There was no evidence of significant heterogeneity between the studies (tau-square = 0.00, chi-square = 0.15, 1 degree of freedom, p = 0.7; I2 = 0).

Fig. 4. Forest plot to demonstrate relative risk ratio of primary haemorrhage between coblation and cold dissection tonsillectomy. M–H = Mantel–Haenszel; CI = confidence interval; df = degrees of freedom
Quantitative synthesis of secondary haemorrhage
Seven studies with 635 patients contributed data to the meta-analysis, with 4 studies showing events of secondary haemorrhage (Tables 5 and 6). Coblation showed a 0.52 (p = 0.34; 95 per cent CI = 0.14 to 1.99) relative risk for primary haemorrhage events when compared to cold dissection tonsillectomy. This is shown in the forest plot in Figure 5. There was no evidence of significant heterogeneity between the studies (tau-square = 0.00, chi-square = 2.31, 3 degrees of freedom, p = 0.51; I2 = 0).

Fig. 5. Forest plot to demonstrate relative risk ratio of secondary haemorrhage between coblation and cold dissection tonsillectomy. M–H = Mantel–Haenszel; CI = confidence interval; df = degrees of freedom
Discussion
When this meta-analysis was conducted, there were two other meta-analyses that had previously compared coblation to multiple other techniques, both hot and cold, the latter being an update on the first.Reference Pynnonen, Brinkmeier, Thorne, Chong and Burton24,Reference Burton and Doree25 A similar systematic review was conducted by Metcalfe et al., in which a range of modalities were reviewed.Reference Metcalfe, Muzaffar, Daultrey and Coulson26 However, none of these studies were specific to only coblation and cold dissection tonsillectomy, or to paediatric patients.
• Coblation appears to cause less pain than cold dissection tonsillectomy
• Coblation involves a shorter operation with less intra-operative blood loss
• There is no statistical difference between coblation and cold dissection tonsillectomy in post-operative haemorrhage
• New population-based studies with better statistical power are required to determine the true statistical difference for post-operative haemorrhage
• Coblation offers an alternative to cold dissection, with some better outcomes
Main findings
There are always attempts to minimise the consequences of any surgical procedure. Paediatric and adult tonsillectomy are very different as there are different challenges regarding management decisions. Pain is an almost guaranteed consequence of tonsillectomy; the degree of pain will affect a child's ability to eat and the consequent timely discharge. A child's ability to eat is also a predictive factor for post-operative haemorrhage. In addition, a shorter operative time may reduce the patient's risk of chest infections and pneumonia whilst anaesthetised.
Summary and appraisal of evidence
This meta-analysis, which comprised data from seven studies, showed that coblation tonsillectomy may be a viable alternative to cold dissection tonsillectomy in paediatric patients.
There were inconsistencies in the way evidence was reported in the studies, especially when assessing the outcome of pain. This is discussed further in the section ‘Study limitations and heterogeneity’ below.
Of the studies included, one specific study seemed to give anomalous results for intra-operative blood loss, despite using the random effects model for meta-analysis. The test was repeated after removing data from the study by Omrani et al.Reference Omrani, Barati, Omidifar, Okhovvat and Hashemi18 However, the data still showed a significant reduction in intra-operative blood loss for coblation tonsillectomy when compared to cold dissection.
Study strengths
The findings are similar to those of other studies and evidence in the literature. Two other reviews have been carried out, by Pynnonen et al.Reference Pynnonen, Brinkmeier, Thorne, Chong and Burton24 and Metcalfe et al.,Reference Metcalfe, Muzaffar, Daultrey and Coulson26 with Pynnonen et al. updating a previous review completed by Burton et al.Reference Burton and Doree25 The reviews found coblation to have at least comparable outcomes, if not significantly better outcomes, when compared to the cold dissection technique. These studies included both paediatric and adult populations. The current findings support the existing evidence, but for paediatric patients.
Study limitations and heterogeneity
The first limitation of this study concerns the outcomes. Firstly, with regard to pain, whilst it may be possible to objectify a pain score, it is still always a subjective feeling. There are many factors associated with pain and its perception, which may affect how it is reported between people. In addition, pain was assessed in terms of the Wong-Baker Faces score, which is given in a range of discrete values (0–5); however, this was sometimes reported as a continuous value.Reference Garra, Singer, Domingo and Thode22,Reference Garra, Singer, Taira, Chohan, Cardoz and Chisena23 This outcome was reported in various different ways. The scale uses discrete values; however, the data presented were never consistent with the data type, and therefore no statistical analysis was performed. The authors of the studies in question were contacted for the data, but there was no response. The other issue is that reporting pain is dependent on the ability of the child to communicate this. Whilst an older child may be able to communicate this well, a younger child will not be able to communicate pain as effectively.
The second and biggest limitation concerns intra-operative blood loss. Coblation uses a conduction medium (saline) in order to cause tissue disintegration. Given the different flow rates and a difficulty in timing, it would be very difficult to determine the blood loss without any contribution from the conduction medium. Whilst a conduction medium may contribute to the blood volume, the true value may be less; this demonstrates the superiority in intra-operative blood loss with the coblation technique.
Another limitation of the original studies is related to power calculations. In order for any study results or conclusions to be applied to the general population, power calculations must be completed, to ensure sufficient numbers in the study sample. Power calculations were not evident in any of the studies included, and no calculations were made. Therefore, there is a possibility that the results of this meta-analysis may not be a true reflection of the population. However, as already mentioned, this analysis supports the findings of previous pooled analyses reported in the published literature.
Following on from the limitation concerning power calculations, the numbers of reported haemorrhage rates were low, particularly with regard to secondary haemorrhage rates. Given the low numbers, it may not be a true reflection of the population. The numbers may have resulted in study or publication bias. However, this does introduce an important question regarding attempts to assess haemorrhage rates. A large study is required to truly assess this.
In the study conducted by Matin et al., no standard deviations were reported; these values were therefore estimated using a basic method.Reference Matin, Chowdhury, Haque, Islam, Shamim and Muqeet16 It was assumed that the data were normally distributed, and thus 95 per cent of the data would be within 2 standard deviations of the mean. As a range was reported, the difference of the range was divided by four to estimate the standard deviations.
The lack of regional restrictions placed on the studies should not have limited the current study findings. Most of the studies used in this meta-analysis were conducted in different countries within Asia. This may demonstrate differences in techniques, experience and user ability.
The final limitation of note, which may have introduced bias into the study, was that of blinding. None of the studies specifically discussed methods of blinding; therefore, there is a possibility of bias in terms of patient selection.
Importance and implications for practice
The National Prospective Tonsillectomy Audit yielded valuable information, from a significant sample size.Reference Mitic, Tvinnereim, Lie and Saltyte17 That audit included over 20 000 paediatric patients and their outcomes. It is clear from the audit findings that most tonsillectomies (48 per cent) were conducted using the cold steel dissection technique, with less than 5 per cent of tonsillectomies carried out by coblation. The audit also revealed that coblation and other ‘hot’ techniques seemed to carry a higher risk for primary and secondary haemorrhages, reported to be 2.4–3.2 times higher compared to cold dissection techniques.Reference Lowe, van der Meulen, Cromwell, Lewsey, Copley and Browne2 However, the current study, with albeit fewer participants, shows coblation to be a viable alternative to cold dissection techniques.
There are two other implications that concern clinical practice. The first is the reduced pain, as demonstrated by the lower Wong-Baker Faces scores in individual studies.Reference Elbadawey, Hegazy, Eltahan and Powell15,Reference Paramasivan, Arumugam and Kameswaran19 Secondly, whilst there has always been evidence that post-operative haemorrhage incidence was greater in coblation tonsillectomy, the results from this study showed that there is no significant difference.
Implications for research and further studies
Further research is still required to provide better evidence, especially with regard to other techniques. It is important to measure each outcome between different studies. This will provide a greater understanding as to which technique is actually the better one. Secondly, a large multicentre trial that evaluates the difference in techniques, especially haemorrhage rates, is required to attain truly applicable evidence.
Conclusion
In children, tonsillectomy by coblation may offer better overall intra-operative and post-operative outcomes when compared to cold dissection tonsillectomy. Pain and haemorrhage are the biggest drawbacks of the procedure; coblation tonsillectomy appears to be less painful in the post-operative setting. The use of coblation tonsillectomy, especially within day-case procedures, should be considered in an attempt to allow quicker recovery and subsequent discharge.
Competing interests
None declared