Introduction
Triage is an essential component of providing unscheduled health services, particularly during disasters Reference Born, Briggs and Ciraulo1 and at mass gatherings where marked variability in demand is seen. Reference Bullock, Ranse and Hutton2 Triage allows efficient utilization of health care resources, which leads to better matching of demand for and supply of health care resources, including in mass-casualty settings. Reference Bazyar, Farrokhi and Khankeh3 Triage has been a standard part of delivering emergency medicine for decades, and is widely discussed in the disaster management literature. It is routine to consider mass gatherings as “planned emergencies,” where large demands on health care services, including by patients with significant illnesses, may be made. Reference Ranse, Hutton and Keene4
Triage scales used in emergency departments demonstrated reasonable validity in discriminating between well and unwell patients in a recent systematic review and meta-analysis, though wide variation was seen. Reference Zachariasse, Hagen, Seiger, Mackway-Jones, Veen and Moll5 In the Australian context, the Australasian Triage Scale (ATS) is used nearly universally in emergency departments, primarily by triage nurses. Australian triage nurses using the ATS have been shown to make the expected triage decision 61% of the time, while 18% of decisions were under-triaged and 21% were over-triaged. Reference Considine, LeVasseur and Villanueva6
Triage scales adapted from disaster triage have been evaluated in many settings, including mass gatherings. There is an observed high rate of over-triage, which may have implications for resource allocation. Reference Turris and Lund7 An Australian-specific tool delivered by first aid staff has been developed to address observed deficiencies in current practice, but its performance has not been evaluated. Reference Cannon, Roitman, Ranse and Morphet8 One of the key tasks of triage systems is to both identify patients who need urgent care at the event site, and to identify patients who need to be transported to hospital via ambulance. Reference Ranse, Hutton and Keene4 In general, a significant over-triage effect is seen, and non-traumatic injuries are commonly not accounted for. Reference Heller, Salvador, Frank, Schiffner, Kipke and Kleber9 The Simple Treatment and Rapid Triage (START) tool is preferred by some authors, on account of its bias towards over-triage and high sensitivity for critically unwell patients. Reference Kahn, Schultz, Miller and Anderson10 It is likely that significant publication bias exists in the current literature, limiting the ability of policy makers to make informed choices about the best way to conduct triage at mass gatherings. Reference Timbie, Ringel and Fox11
First aid staff members are often employed to conduct triage at mass gatherings, whether implicitly or explicitly. Recent advice from New South Wales Department of Health (Surry Hills, New South Wales, Australia) has suggested the use of nurses in the triage role, based on a concern that first aid staff members may have inadequate experience in performing triage. The performance of first aid staff members in achieving guideline-recommended triage has not been examined, and this study aimed to bridge this gap in the literature.
Methods
An audit was conducted of patients presenting for care at mass gatherings by a single organization supplying medical services in Victoria (Australia) from 2018-2019.
Database
The audit was conducted using a database of patient presentations owned by Event Medical Services Australia (Melbourne, Victoria, Australia). The database contains summary-level reports, and did not contain individually identifiable or re-identifiable patient data. The database and dictionary had not been previously referenced. The sources for raw data were the patient care records of the organization. The inclusion and exclusion criteria for the database are listed below. Data entry staff were trained by one of the investigators using a standardized template, who directly supervised the data entry work on an ongoing basis, and was available to answer questions when required. No data abstraction training was provided and the accuracy of abstraction was not measured.
There had not been previously published estimates of the accuracy of the data contained within the database. As such, a small sample audit of approximately five percent of records was conducted. This audit demonstrated a data accuracy rate of 98.4% for all entries. Where errors were discovered, they were corrected.
Ethical Approval
Ethical approval was provided by the Edith Cowan University (Joondalup, Western Australia, Australia) Human Research Ethics Committee in April 2019. The study was conducted in accordance with the Declaration of Helsinki.
Inclusion and Exclusion Criteria
The study included all patients presenting to the provider for care during the period of 2016-2018. Patients were included if a set of observations were taken. Patients were excluded if their presentation did not require a set of observations to be taken, for example if they requested a band aid for a blister.
Equipment
Measurement of variables was standardized over the study period. The physiological variables had been measured either with standard clinical approaches (heart rate measurement by taking the patient’s pulse; blood pressure using an aneroid syphgmomanometer), or using the Philips M3001A Multi-Measurement Server (Philips GMBH; Amsterdam, The Netherlands) for the heart rate, blood pressure, and oxygen saturation. Temperature had been measured using the Braun Thermoscan 6000 tympanic thermometer (B Brauna; Melsungen, Germany). The Glasgow Coma Scale (GCS) was measured by first aid, medical, paramedic, and nursing staff trained in the evaluation of the GCS. Statistical analysis was performed using SPSS Statistics v23 (IBM; Armonk, New York USA). The receiver operating characteristic (ROC) analysis was performed using easyROC (Hacettepe University; Ankara, Turkey). Reference Goksuluk, Korkmaz, Zararsiz and Karaagaoglu12
Primary Triage Strategy
The primary triage strategy refers to the triage system used by the first aid staff at the events. The organization specified the use of a modified version of the START algorithm. The basic algorithm specifies that if a patient is able to walk, they are triaged into the Green category. If the patient cannot walk, they are assessed for spontaneous breathing, including positioning the airway if needed. If they are not breathing spontaneously, they are categorized as Expectant, and if they are only breathing spontaneously after airway positioning, they are classified into the Red (Immediate) category. If patients have an open airway and are breathing spontaneously, the respiratory rate is assessed. If it is over 30 breaths per minute, the patient is also assigned to the Red (Immediate) category. If the respiratory rate is less than 30 breaths per minute, the perfusion status is assessed. If the radial pulse is absent, or the capillary refill time is greater than two seconds, the patient is assigned the triage category of Red (Immediate). If perfusion is assessed as normal, lastly, the mental status is assessed, and if the patient obeys commands, they are classified as Yellow (Delayed), or Red (Immediate) if they do not.
The organization recognized that in the mass-gathering context where medical and drug and alcohol problems are prevalent, the START system may have been insufficiently sensitive to some important problems that frequently presented, such as drug and alcohol presentations. Reference Turris and Lund7 As such, staff were instructed to include history elements in their triage decisions and to up-triage patients presenting with problems such as chest pain, asthma, and drug and alcohol problems where the patient’s clinical presentation required.
Secondary Triage Strategy
The secondary triage strategy refers to the triage decision made for the purpose of the research, which occurred some months to years after the event. The presentation was rated by one of the authors (ND) using an algorithm conceptually inspired by the Emergency Severity Index, 13 which was contextualized to the mass-gathering environment. The author was blinded to the triage decision made by the first aid staff member. In making these classifications, a Green (Walking) patient would be expected to have normal physiology other than mild elevation of heart rate or respiratory rate, which can be elevated for many reasons. A Yellow (Delayed) patient could have mildly abnormal physiology on one or more variables, and needed a GCS of 13 or greater and to able to follow commands. A Red (Immediate) patient would have significantly abnormal physiology in any or multiple variables. The classification system is shown in detail in Table 1. A comparison chart of the two systems is included as Figure 1.
Table 1. Secondary Triage Strategy

Abbreviations: GCS, Glasgow Coma Scale; HR, heart rate (beats per minute); RR, respiratory rate (breaths per minute); SBP, systolic blood pressure; SpO2, oxygen saturation.

Figure 1. Receiver Operating Characteristic Curve for the Two Triage Strategies.
The primary triage decisions were then compared to the physiology-based secondary system and classified as “expected” if the two systems agreed on the triage classification, “under-triaged” if the secondary system suggested a sicker patient than the primary decision suggested, and “over-triaged” if the secondary decision suggested a safer patient than the primary decision suggested.
Outcomes
The baseline characteristics recorded for each presentation included the patient’s age and type of event they presented at, classified as a music festival, sporting event, or community event.
The primary comparison outcome was whether the assigned primary triage category was considered expected when compared to the secondary triage decision, which was based on the available physiological data. This primary triage decision was decided by the first aid staff member, following the established guidelines within the organization.
The physiological variables considered for the secondary triage decision included heart rate, systolic blood pressure, respiratory rate, oxygen saturation, conscious state as measured using the GCS, and temperature.
The secondary outcomes included the rate of under-triage, which was adjudicated when the secondary triage decision was of a more urgent category than the primary triage decision, and the rate of over-triage, where the secondary triage decision was of a less urgent category than the primary decision.
The reasons for over-triage could not be elucidated from the data, and were likely related to history factors not captured by the data extraction. The physiological variable that drove the discrepancy between the primary and secondary triage decisions was, however, available when under-triage occurred, and under-triage was considered a more important problem than over-triage in the clinical context. As such, the physiological variable driving the discrepancy was recorded and presented.
Where more than one physiological variable was abnormal, the more severely abnormal was chosen as the driver, unless the GCS was abnormal, where it was preferentially selected. The rationale for this approach was that the inclusion of these variables could be used to improve the triage system into the future, and the authors considered the most obviously abnormal variable to be the most useful variable for potential inclusion.
Statistical Analysis
The primary outcome was presented descriptively, as were the secondary outcomes of under-and over-triage decisions.
The primary and secondary outcomes were pre-specified as acceptable if greater than or equal to 61% of decisions were expected, and fewer than or equal to 18% of decisions were under-triaged and fewer than or equal to 21% of decisions were over-triaged.
No prior assumptions were formed for the direction or reasons for mis-triage given the lack of prior data.
The performance of the two triage systems in identifying presentations requiring ambulance transport to hospital was assessed using the area under the ROC curve (AUROC). A pre-specified threshold of 0.7 was set, in line with commonly recommended thresholds. The sensitivity and specificity were reported. In comparing the two triage systems, the study used De Long, et al’s method and a pre-specified threshold for significance was set at P < .05. The Youden’s index method was used to determine the optimal cut-point for discrimination between presentations requiring transport and those that did not require transport. Reference Goksuluk, Korkmaz, Zararsiz and Karaagaoglu12
For each triage category, the sensitivity, specificity, and positive and negative likelihood ratios are reported.
Results
A total of 1,048 patients were included for screening, representing a sequential sample of the patients meeting the inclusion criteria. The median age was 21 years, and 980 presentations occurred at music festivals, with 68 at community events.
Complete triage data were available for 91% of presentations. No triage code was recorded for 96 presentations (9%); 945 presentations entered the analysis. No presentations were triaged as Expectant. A total of 728 presentations were primarily triaged as Green (Walking), while 186 were triaged as Yellow (Delayed), and 38 as Red (Immediate). The median physiology of each group is displayed in Table 2. A total of 48 patients were transported to hospital by ambulance.
Table 2. Median Physiology of the Presentations as Coded by the Primary Triage System

Abbreviations: GCS, Glasgow Coma Scale; HR, heart rate (beats per minute); RR, respiratory rate (breaths per minute); SBP, systolic blood pressure; SpO2, oxygen saturation.
For the primary outcome, the expected decision was made in 674 (71%) of presentations for which a triage code was available.
For the secondary outcomes, under-triage occurred in 118 (12%) of presentations and over-triage in 142 (15%) of presentations. The degree of mis-triage varied with the direction of mis-triage. In the under-triaged presentations, 97 (74%) were mis-triaged by a single category, while 34 (26%) were mis-triaged by two categories. In the over-triaged presentations, 126 (89%) were mis-triaged by a single category, while 16 (11%) were mis-triaged by two categories. Table 3 shows the full distribution of presentations across the various triage classifications.
Table 3. Distribution of Presentations by the Triage Classifications
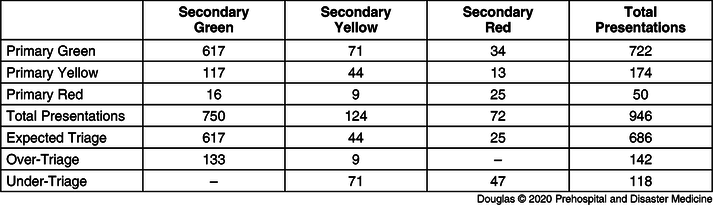
The performance of primary triage strategy varied by triage category. In the Green (Waking) initial triage category, 619 (85%) presentations were classified as expected. In the Yellow (Delayed) category, 44 (23%) were triaged as expected, and 13 (30%) in the Red (Immediate) category.
The physiological variable that could have revealed the need for a higher triage category was heart rate in 41 (32%) of presentations, respiratory rate in 28 (22%), GCS in 31 (24%), temperature in 27 (21%), and blood pressure in two (2%).
When examining the primary and secondary triage strategies for their ability to detect patients requiring transport to hospital, the primary triage strategy had an AUROC curve of 0.76, while the secondary triage strategy had an AUROC of 0.63. Comparing the two strategies using De Long, et al’s method, the AUROC curves were significantly different, with P = .0199. The full description of the performance of the triage systems are available in Table 4.
Table 4. Diagnostic Test Performance of the Primary Triage System Categories as Applied by First Aid Staff Members Compared to Physiology-Based Triage

Discussion
This study was the first to evaluate the performance of first aid staff members undertaking triage at Australian mass gatherings, and to examine the performance of a modified version of the START triage tool adapted for mass-gathering health care in a non-simulated context.
The performance of both the first aid staff members and the tool appeared comparable or superior to reported literature on the performance of emergency department triage nurses using the ATS. Reassuringly, the expected triage decision rate exceeded the pre-specified endpoint, and both the under- and over-triage rates were below the pre-specified cut offs. This is despite triage training in current first aid training courses being very limited, and many first aid staff members having only relatively limited clinical experience.
While the primary triage strategy demonstrated decreasing sensitivity with increasing severity, this is likely due to the presence of unmeasured information in the clinical history that reassured the first aid staff members. Reassuringly, the accuracy of the triage increased with severity, implying that very unwell patients were likely to be recognized by the primary triage system. The results of the reasons that patients were mis-triaged are not surprising given the current guidelines. Many of the parameters are not measured in the current system, and may be first measured when a patient is brought into the assessment area of the medical center. However, the fact that the measured physiology was different between the primary triage categories suggests that the first aid staff members were able to detect some differences between patients without formally using physiological markers. Some refinement of the triage system to better detect unwell patients may be possible using these results, particularly in incorporating rapid measurement of heart rate (for example using a pulse oximeter or hand measurement) and GCS (for example with screening questions). Further research should explore the performance against current gold standards, such as triage nurse assessment.
An interesting finding of the analysis was that the secondary, physiology-based, triage system had reduced discriminatory power to detect patients who subsequently required transport to hospital via ambulance. On this basis, it does not seem reasonable to change current practice to incorporate sophisticated measurement of vital signs early in the triage process.
This analysis supports the continuing, and even perhaps expanded, use of first aid staff using simple tools in triage roles at mass gatherings in Australia, in contrast to recent government advice.
Limitations
The study is limited by the fact it only examined the performance of a single company providing services at mass gatherings in Australia, which may limit its generalizability. This limitation is somewhat ameliorated by the large number of presentations enrolled in the study, and consequently, the number of different first aid staff members engaged in the role. There is an urgent need for industry-wide collaborative research among providers to understand the generalizability of these results.
The study’s discriminatory power in terms of ambulance transport to hospital is somewhat limited by the small number of transport events that occurred.
The study’s ability to inform drivers of the mis-triage events is limited by the inability to discover what drove the over-triage events. While these may be less risky for patients than under-triage events, they contribute significantly to waste in resource allocation. There is a need for research examining both under- and over-triage events that accesses history information to discover the causes of these events.
Conclusion
First aid trained staff performed at least as well as hospital emergency department nurses, if not better, at providing triage according to organizational guidelines at mass gatherings. The performance of the modified START triage system appeared superior to a physiology-based system at identifying patients that required ambulance transport to hospital. The data support the continued use of first aid staff members using simple triage tools in the triage role at Australian mass gatherings. Further work is required to assess the comparative effectiveness of triage by first aid staff to the current gold standard, which is triage by registered nurses.
Conflicts of interest
none







