Echocardiography skills are a key component to the development of a skilled paediatric cardiologist. To become a consummate paediatric cardiologist, trainees must also develop skills in other sub-disciplines including clinical care, catheterisation, electrophysiology, and adult CHD.Reference Graham and Beekman 1 Given the competing time demands to acquire clinical competence in these areas during fellowship training, strategies to increase efficiency of their training are of interest.
Simulation training has become widespread in many aspects of medical education, and simulation is beneficial in a range of other procedural-based specialities.Reference Knudson and Sisley 2 , Reference Ferlitsch, Glauninger and Gupper 3 Benefits such as eliminating patient risk are evident, but exposure for trainees to rare but critical clinical scenarios can also improve skills acquisition. The incorporation of a realistic echocardiographic simulator may augment the training of paediatric cardiology fellows in this manner as a supplement to their traditional echocardiography training.
A simulator-based transthoracic echocardiography trainer for CHD has been demonstrated to be effective in the training of paediatric residents.Reference Wagner, Razek and Grafe 4 We evaluated the effectiveness of a simulator-based echocardiography training session among paediatric cardiology fellows for the diagnosis of CHD.
Materials and methods
Simulator training setting
The EchoCom echocardiography simulator (EchoCom GmbH, Leipzig, Germany) projects two-dimensional echocardiographic images on a computer screen in a manner based on how the operator locates, angles, and positions the dummy ultrasound probe on the chest of a neonatal manikin. Adjacent to the two-dimensional echocardiographic projection is a visual description of the scan plane on a virtual heart. Figure 1 shows a screenshot of the simulator screen. Eleven paediatric cardiology fellows underwent a 4-hour hands-on simulator-based training session led by an echocardiography attending physician (J.D.D., P.A.F.). The simulation training sessions were conducted individually midway (between December and February) through their first (n=5), second (n=5), and third (n=1) year of fellowship training. None of the paediatric cardiology fellows had prior exposure to the use of an echocardiography simulator before or during their fellowship training. The session included real-time scanning with a review of probe positions, image optimisation, anatomic details of multiple forms of CHD, and normal anatomy. The particular diagnoses selected to review in the session were chosen based on the most common forms of CHD, which fellows were expected to encounter during their training. In addition to normal anatomy, individual cases of tetralogy of Fallot, d-transposition of the great arteries, ventricular septal defect, atrioventricular canal defects, hypoplastic left heart syndrome, and tricuspid atresia were reviewed. Other than the echocardiography simulator, no other teaching tools were used in the training session.
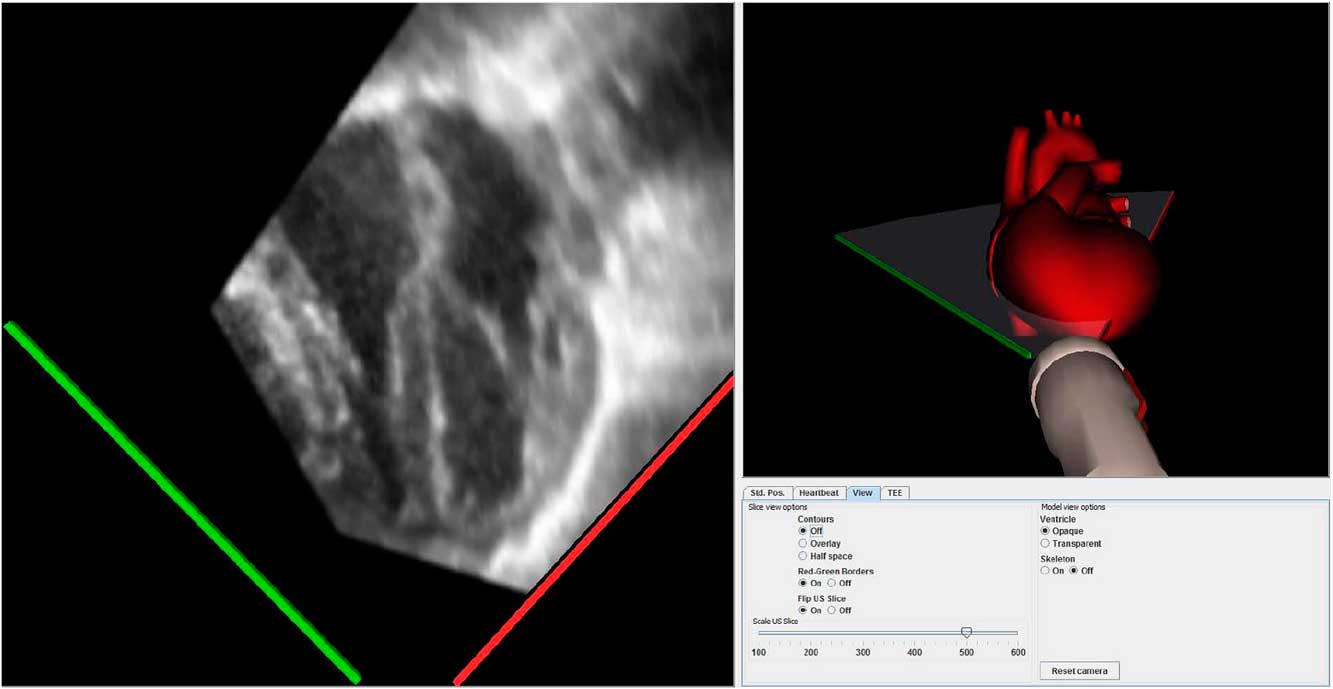
Figure 1 Screenshot of the echocardiography simulator showing two-dimensional image (left) and corresponding scan plane with probe position on simulated heart (right).
Assessment
Knowledge of CHD was evaluated by participants’ score on a 26-point multiple-choice test administered before and after the training session. All trainees completed the assessments immediately before and after the simulation session. The same questions were used in the pre- and post-training knowledge assessments to reduce the risk of bias from different questions being used of potentially different difficulty and the answers were not provided to the trainees after the pre-training assessment. Questions on the knowledge-based assessment focussed on anatomic views, probe positioning, and movement, and included echocardiographic images asking the trainee to identify anatomic details of normal and abnormal cardiac anatomy. Echocardiographic performance was evaluated by presenting each trainee with five different cases of CHD before and after the training session while assessing diagnostic accuracy. For both the pre- and post-performance evaluation of diagnostic accuracy, the trainee was asked for a diagnosis in an open-ended manner and was not provided with multiple choices to select from. The set of cases used in the pre-assessment and post-assessment were different but of similar difficulty and not seen previously by the trainee (including during the training session). The diagnoses used in each assessment included a case of tetralogy of Fallot, d-transposition of the great arteries, complete atrioventricular canal, single ventricle, and a normal heart. The particular cases used in the pre-assessment and post-assessment were the same for all trainees. All trainees completed an evaluation at the conclusion of the simulation session.
Analysis
The Wilcoxon rank-sum test was used to compare pre-simulator training scores with post-simulator scores of echocardiographic performance and knowledge of CHD. All statistical tests were two-sided and p<0.05 was considered statistically significant. All analyses were performed in SAS Version 9.4 (SAS Institute Inc., Cary, North Carolina, United States of America).
Results
There was improvement in knowledge of CHD and echocardiographic performance following the simulation-based training session. Median score on the knowledge-based multiple-choice test increased from 20 (range 14–25) to 24 (range 17–25) (p=0.0078). Median diagnostic accuracy on the echocardiographic performance assessment increased from 80% (range 20–100%) to 100% (range 80–100%) (p=0.0078). Detailed graphical presentation of multiple-choice testing and echocardiographic performance are shown in Figure 2. A total of 100% (n=11) of the trainees reported that the simulator improved both their knowledge of and ability to diagnose CHD. In all, 82% (n=9) reported that the simulator improved their technical skills to perform a transthoracic echocardiogram.

Figure 2 Knowledge and echocardiographic performance assessment. Pre- and post-simulation: ( a ) knowledge-based examination test scores; and ( b ) echocardiographic performance results showing an improvement in examination score and diagnostic accuracy following simulation training.
Discussion
This report demonstrates the feasibility and short-term effectiveness of a simulator-based echocardiography training module for paediatric cardiology fellows in our training programme here at Weill Cornell Medical College. The simulator used has been shown to be a realistic representation of cardiac anatomy and a robust assessment tool for the diagnosis of CHD.Reference Weidenback, Razek and Wild 5 Our report is unique in its assessment of echocardiography simulation training focused solely on paediatric cardiology trainees.
Importantly, we evaluated the effectiveness of the simulator for trainees who are concurrently receiving traditional echocardiography training and found that there is still an improvement in their knowledge and echocardiography skills in CHD. Therefore, the use of an echocardiography simulator has the potential to augment training for fellows who are receiving standard training via the traditional apprenticeship model. In addition, educators will also have the opportunity for on-demand case training to assess trainees’ knowledge while providing real-time feedback to facilitate skills acquisition.
Condensed training programmes, often described in the form of a “boot camp”, are more commonly being incorporated into the training of paediatric cardiology fellowship programmes to better prepare individuals for the technical and procedural components of their training. Maskatia et alReference Maskatia, Altman, Morris and Cabrera 6 have reported the use of an echocardiography boot camp to advance participants’ skills in paediatric cardiovascular imaging education. Subsequent studies have evaluated the experience of paediatric cardiology fellows participating in an educational boot camp, which incorporated simulation modules into their curriculum.Reference Ceresnak, Axelrod, Motonaga, Johnson and Krawczeski 7 – Reference Ceresnak, Axelrod, Sacks, Motonaga, Johnson and Krawczeski 9 Interestingly, the simulation-based activities were among those rated most highly by fellows in one evaluation.Reference Allan, Tannous and DeWitt 8 Our study provides a favourable in-depth analysis of the effectiveness of echocardiography simulation training, which may warrant more widespread inclusion in the regular imaging education and boot-camp portion of fellowship training.
Simulation-based training has been shown to improve the performance of adult cardiology fellows in interventional and electrophysiology procedures.Reference DePonti, Marazzi, Ghiringhelli, Salerno-Uriarte, Calkins and Cheng 10 – Reference Voelker, Petri and Tonissen 12 The effectiveness of these training methods demonstrates that realistic simulator-based training modalities have the potential to improve education and patient care. With demonstration of effectiveness of the simulator used in our training module, simulation training appears ready for more widespread use in the echocardiographic training for CHD in a manner similar to other aspects of cardiology training. Curricula development for the incorporation of simulators into clinical training programmes has the potential to accelerate the acquisition of these skills in a setting more comfortable for trainees and risk-free for patients. Simulation training in the standard 3 years of traditional paediatric fellowship may strengthen imaging skills among all trainees and also become particularly useful in providing additional imaging opportunities for those not seeking advanced imaging training as a 4th-year experience.
Future areas of study should include assessment of echocardiographic images obtained on live patients after undergoing simulation training. Technologic improvements in simulation are inevitable, including those for echocardiography. Future improvements, such as addition of color Doppler, would make the simulator experience even more realistic, thereby making the skills learned through simulation more likely to translate into better clinical care.
Our report demonstrates that simulator training is an effective addition to training for paediatric cardiology fellows in CHD at our centre. While future studies should evaluate a longer-term experience of paediatric cardiology fellows’ experience with simulation training and its impact on clinical care, simulator education appears feasible and ready for incorporation into their training.
Acknowledgements
The authors appreciate the contributions of Kevin Ching, Linda M. Gerber, and Hoda T. Hammad to this project.
Financial Support
This research received no specific grant from any funding agency, commercial, or not-for-profit sectors.
Conflicts of Interest
None.





