Introduction
At the time of writing, the World Health Organization (WHO; Geneva, Switzerland) Strategic Advisory Group has very recently endorsed the sign-off of a minimum data set (MDS) for daily reporting for emergency medical teams (EMTs) in sudden onset disasters (SODs). 1 This was developed by deriving candidate items from multiple international sources of medical records and reporting systems which were then distilled and refined by expert consensus in a WHO MDS working group.Reference Kubo 2 This work is not being done in isolation as it complements the WHO agenda for standardization of EMT practice. 3
There is wide disparity in the use of medical record keeping systems across EMTs and in different SODs.Reference Kubo 2 , Reference Jafar, Norton, Lecky and Redmond 4 The MDS is intended to formalize data-gathering to allow Ministries of Health (MoHs) and EMT co-ordination cells (EMTCCs) to receive guaranteed daily data from EMTs in support of their response planning. However, the MDS data items need to be collected accurately to be useful.
Following on from work done as part of the WHO MDS working group, the UK EMT medical record (note that UK-Med [Manchester, UK] provides the medical arm of UK EMT) has been redeveloped to ensure that, as a minimum, there is a single record sheet for all patients that encompasses the MDS requirements. This single sheet, although being developed in conjunction with a more comprehensive record process (which exists both in paper and electronic format), is in many ways the most important recording item. Its importance lies in the fact that it should be this sheet, which, regardless of working conditions, access to electricity, and patient volume, is always filled in and made available to patients, the national MoH, and the EMT themselves.
The UK EMT single sheet (Figure 1) was developed between September 2016 and December 2016 in collaboration with a commercial company, L2S2 (Cambridge, UK) who is working with the UK EMT to develop an electronic patient record that works synergistically with a paper-based system. Members of the UK EMT developed the content of the form based on the WHO MDS and the basic essentials of a functional medical record. This was derived from examples of other single-sheet records, combined with clinical and field experience. The intended use of this single sheet is completion for each patient, regardless of whether or not they are inpatients or outpatients. The sheet will accompany the patient from initial contact through to conclusion of that contact. At the basic level, this sheet will be paper-based; however, as deployment conditions permit, each sheet will be scanned with some data being auto-recognized and collated and other data requiring manual collation.
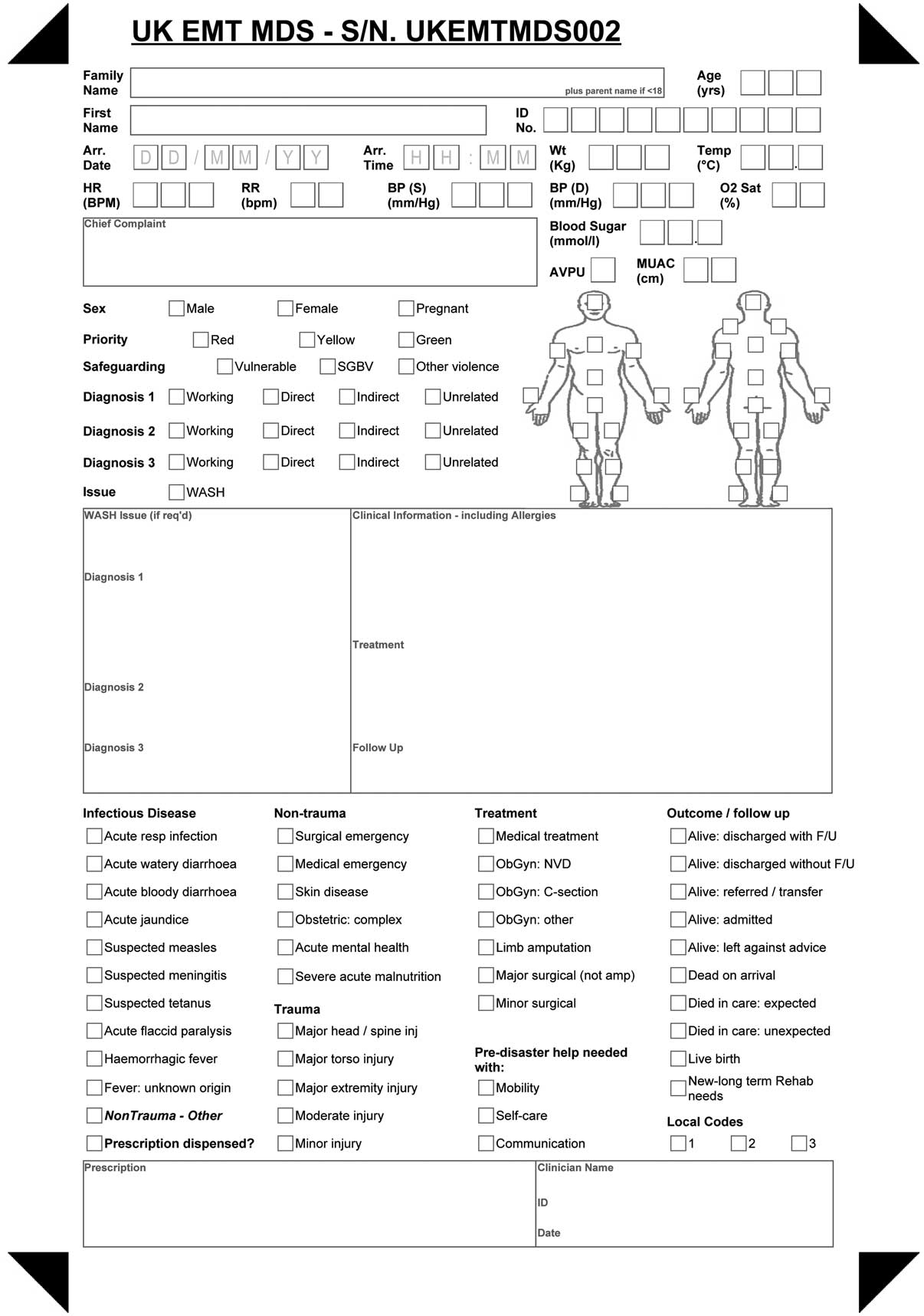
Figure 1 Single Minimum Data Set Compliant Sheet Used During the Pilot Exercise. Abbreviations: EMT, emergency medical team; MDS, minimum data set.
In order to advance the UK EMT record, with a focus on this single sheet, it was important to understand how the prototype could be used in practice, what fields might not be filled in naturally, and whether the flow of the form worked. This is crucial in securing the accuracy and quality of the record itself, and the data subsequently extracted. An operational review was therefore conducted to gain insight into the use of this medical record in practice to allow assessment of its utility and the need for any modification prior to deployment of the team.
Methods
The UK EMT single sheet (Figure 1) was printed as a triplicate, carbonless copy system so that one sheet each will be available to the patient, the MoH/EMTCC, and the EMT.
During a deployment training course, the 33 participants were required to camp and carry out activities as if living and working within a real field hospital. They attended a range of training activities matched to their proposed work in a field hospital deployment. The session on medical records was not labeled as such on the program, thereby avoiding any pre-meeting preparation bias.
The 33 participants were: 15 nurses; seven allied health professionals (encompassing radiography, physiotherapy, and public health); six paramedics; and five doctors; and they all were taught across two identical sessions.
The session was introduced as a simulation exercise wherein faculty members were provided with a scenario and told to act as patients. The participants were provided with a pen and the single medical record sheet and told they had only five minutes to see the patient as if they were a new presentation to the field hospital. They were told that anything else they wished to know, which went beyond talking to the patients, such as vital signs and examination findings, could be asked of the faculty and, if available in the scenario crib sheet, would be provided.
The setting for the consultation was a disused farm building and therefore participants had to make do with any available limited seating. Once the five minutes had finished, all paperwork was collected. At this point, it was explained to the participants that the exercise had been intended to see how they would interact with an unfamiliar medical record. It was explained that the purpose of such an exercise was to get a sense of which areas of the record would be focused upon in a stressful situation and which areas might be neglected.
The importance of medical record keeping in this context was discussed, as well as how it links with the WHO MDS for daily reporting. The latter part of the session explored the electronic record being developed in conjunction with the paper record. During this time, the medical records that had been filled in were briefly reviewed and some obvious areas, which were not completed by many delegates, were highlighted. At the end of the session, the initial findings were fed back to the group, highlighting in particular those frequently missed areas in the record. These missed areas were linked to their importance to the patient and coordination of the overall disaster response at an MoH level. Feedback was requested pertaining to the form design and content to see if the delegates could identify any significant omissions or barriers to accurate completion. All those participating were advised that this operational review exercise would be used to inform the development of the UK EMT record and may contribute to publication of this development process.
Finally, the single sheets were reviewed in more detail and any name/signature information blacked out on all sheets. There were 42 variables on the form which were analyzed for completeness/accuracy and then entered into a database. Specific issues of flow within the form were scrutinized to identify the pattern in which the delegates appeared to use the form. This was done by reviewing each form and focusing on those areas of the form that were filled in with information which belonged elsewhere. This was done to see if there was a pattern indicating that certain information ought to be captured at a specific point in the form. The candidates’ feedback on use of the record is also presented, as well as reasons for not completing sections.
As this was an operational review of practice and involved no participant identifiable information, the UK-Med medical advisory team exempted it from ethical review with reference number ukmed2017/001.
Results
A total of 32 out of 33 possible records were handed in for review; Table 1 shows the frequency with which each item from the single sheet was completed (Figure 1).
Table 1 Of the 32 Forms Completed, the Number of Times Each Item was Filled In

Abbreviations: AVPU, Alert/Voice/Pain/Unresponsive; MUAC, mid-upper arm circumference; WASH, water, sanitation, and hygiene.
Those variables which were completed “very often” (at least three-quarters of the time) were:
∙ Age;
∙ Sex;
∙ Family name;
∙ First name;
∙ Oxygen saturations;
∙ Blood pressure;
∙ Heart rate;
∙ Clinical information;
∙ Temperature;
∙ Respiratory rate; and
∙ Chief complaint.
However, it was noted that the information in areas of the form such as “diagnosis” did not necessarily represent what was intended to be there. This space and the “chief complaint” space were often used for clinical detail rather than diagnosis. This suggested that the flow of the record may not be as logical or intuitive as it could be.
Those variables which were filled in especially badly (less than one-half of the time) were:
∙ ID number;
∙ Diagnosis;
∙ Diagnosis codes;
∙ Weight;
∙ Treatment codes;
∙ Whether diagnosis is related to the disaster or not;
∙ Outcome/follow-up codes;
∙ Follow-up;
∙ Clinician name/ID/date;
∙ Prescription;
∙ Water, Sanitation, and Hygiene (WASH) issue and details;
∙ Disability screen;
∙ Mid-upper arm circumference (MUAC); and
∙ Safeguarding.
The delegates themselves raised specific issues, such as:
∙ Absence of negatives such as “not pregnant” or “no safeguarding issues” boxes may mean these issues may be assumed, erroneously, to have been considered, and the lack of a filled box equated to a negative answer when in fact it has simply been ignored;
∙ The MUAC requires three boxes with a decimal point rather than two, for a useful reading;
∙ “Allergies” needs to be highlighted and isolated to ensure it is clear and filled in;
∙ Pre-existing disability belongs closer to the demographic data area of the sheet;
∙ Some adjustment of coding order is needed to make all categories sit in a more logical place; and
∙ Prescription information needs to be in one place to ensure it is filled in accurately.
The delegates also discussed the form more broadly and generally felt that with some familiarity it would be speedy enough to complete. They did comment that the flow of the form did not feel as logical as it could; however, many reflected that this was not dissimilar to much of the paperwork they fill in as part of their day-to-day practice.
There were several technical/training issues which were also highlighted by this exercise:
∙ The bottom of the three carbonless sheets had clear information in only two of 32 records;
∙ Extra text was included on the form in just under one-half of records (when used in conjunction with the electronic system, this extra text would not necessarily be captured); and
∙ In around one-third of records, numerical values were filled in from left to right rather than right to left.
All of this feedback was used to remodel some areas of the form, as shown in Figure 2.

Figure 2 Redeveloped Single Sheet. Note: SATIS is an additional system which allows some information to be printed as a label for the first few details. Abbreviation: EMT, emergency medical team.
Discussion
The results demonstrate that the domains of coding, prescription, signature, follow-up, diagnosis, and ID number were filled in in less than 50% of cases. These areas are therefore crucial to emphasize prior to deployment so that team members understand their importance. However, the layout of the form does not appear to flow easily, which has been addressed by altering the layout to reflect how delegates actually completed the form. It is clear from many of the forms that most participants associate a left to right format with the direction of flow. They therefore superimposed their own flow of the consultation (which by convention is likely based in some way around a content guide embedded within a Calgary-Cambridge model)Reference Kurtz, Silverman, Benson and Draper 5 upon the form. That is to say, they wrote their notes in the places they thought they ought to be rather than where the form indicated they should be. This made it very clear that the flow needed to be modified to closely as possible reflect the natural process of a consultation which moves from introduction, through information gathering, and then to explanation and planning.Reference Kurtz, Silverman, Benson and Draper 5
It was noted that MUAC was not filled in at all, but this was appropriate as this value would, in the main, only be looked at for the under-five-years group where it is used as a proxy for malnutrition.Reference Mogeni, Twahir and Bandika 6 Similarly, it would be for this purpose that weight would be important rather than being a requirement in adult patients. With regard to WASH issues, it was already decided before the course that this is better recorded as an overview than for each individual patient. Therefore, it was already intended for this item to be removed from the single sheet.
It was observed that many delegates were using either their knee, the floor, a chair, or a wall to lean on when filling in the record. This may explain why there was such poor penetration down to the third sheet of carbonless paper. This is a key finding as it cannot be assumed that the paper record will be filled in leaning on a desk/table in a field hospital. The carbonless system currently in use therefore needed review. This is to ensure that at a very basic level, if only paper recording is available, there are three legible copies of the medical record: one for the patient, one for the MoH, and one for the team. To remedy this, the same scenario was run again at a subsequent course some time later, this time using the specific ball point pens deemed most suitable to penetrate each sheet and using a clipboard-box for each delegate. Although this improved the penetration, it was still not regarded as acceptable. Therefore, a different triplicate system is being tested while the option of a duplicate system wherein the MoH or the EMT only receive an electronic scanned copy or paper photocopy on conclusion of the deployment is being considered.
Some delegates were noted to fill in the form at the end of the consultation and frequently they stated they had “run out of time” when handing it in and this resulted in forms that were less complete. This indicates that all staff need to be encouraged to “document as they go” to avoid details being missed due to time constraints.
Looking at Figure 3, it is evident that some delegates were filling in numerical values from left to right instead of right to left. In this example, if the information was to be read by a computer, it may erroneously pick up a figure of 970 for systolic blood pressure (instead of 97) and a figure of 830 for diastolic blood pressure (instead of 83). Therefore, it must be ensured that the technology can accommodate digits written in left to right instead of right to left and interpret them correctly, or at least flag them as an error. If this is not addressed, then inaccurate data will be drawn into the electronic system.

Figure 3 Image of Inaccurate Filling of Numerical Boxes Left to Right Instead of Right to Left.
This exercise served a number of purposes: it allowed participants to simulate their use of records; it allowed the team to see how a record might be used unprompted and under stress; it highlighted deficiencies in the record; it allowed participants to contribute to the refinement of the record they will ultimately use; and it reinforced the importance of the record keeping process in line with WHO standards. 3 Having participants involved in the redevelopment of the record utilizes some aspects of user-involvement in research, which has been used much more formally in the form of participatory design in other areas of health care, such as developing technology for major incidents and developing telemedicine systems.Reference Kristensen, Kyng and Palen 7 , Reference Li, Wilson, Stapleton and Cregan 8 The benefits of this approach on a wider scale include:
∙ Improved quality due to better reflection of user requirements;
∙ Avoidance of features which will go unused;
∙ Improved acceptance of what is being proposed;
∙ Better understanding and thus more effective use; and
∙ Increased involvement in decision making.Reference Kujala 9
These benefits are very important in ensuring the medical record’s appropriate and efficient use in order to provide the most useful outputs for patients and the MoH/EMTCC.
Limitations
The exercise had its limitations. Some of the delegates were not patient-facing in their usual roles, and therefore a medical record was quite a new process for them. Similarly, the delegates had varying levels (if any) of experience of working in SODs; therefore, certain aspects of the form might not yet resonate with them. The sample is relatively small and the conditions were not those of a strictly controlled study. The simulation was not wholly realistic in its setting or participants, as there was no full field hospital and the “patient” was very evidently a healthy faculty member, possibly known to the delegate. That said, the conditions were reflective of a stressful environment (a disused farm building, barely above freezing, with little by way of furniture). Arguably, five minutes is too short a time for a consultation, however this was done in an attempt to simulate a potential scenario of high throughput to highlight how the record might function under such pressure.
All feedback and analysis of the forms was reviewed and informed a redevelopment of the form (Figure 2) in preparation for subsequent deployment courses, larger simulation exercises, and ultimately deployment. The final test of how the medical record truly works will be during the first deployment. However, this pilot has allowed the team to iron out some issues so that its first use in a deployment is more likely to produce more reliable data than it would have done without such testing. Following deployment, more broadly applicable conclusions will be available from the much larger volume of data using the redesigned form and subsequent layout changes can be made.
Conclusion
Using training opportunities prior to deployment to SODs can be a useful way to pre-test and improve working practices in the field. This particular pilot of a single-sheet triplicate medical record during an EMT deployment simulation led to significant modifications which hopefully will improve data capture and function. It also had an added advantage of training participants in the process of medical record keeping, which is an area of disaster medicine well known to be poorly prioritized.
Acknowledgement
The authors acknowledge the work of L2S2’s Philip Gaffney and James Belcher.






