Introduction
Normal balance function relies on sensory information from the visual, auditory, peripheral vestibular and somatosensory systems.Reference Kanegaonkar, Amin and Clarke1 This sensory information is integrated and interpreted within the central nervous system to maintain gaze and postural control, and provide information on self and environmental movement.Reference Corcoran and Jones2 Central interpretation requires comparing relayed sensory information with preformed templates within the central nervous system. The absence of a suitable template, or a mismatch between the template and sensory information, results in dizziness, vertigo or unsteadiness.
Assessment of the dizzy patient requires taking a thorough medical history and performing a clinical examination. The Fukuda (or Unterberger) stepping test is commonly performed as part of a full neuro-otological battery.Reference Grommes and Conway3 They both require patients to march on the spot with their eyes closed. Significant rotation or translation is deemed to signify underlying peripheral vestibular hypofunction.Reference Unterberger4 However, previous studies have suggested a maximal sensitivity and specificity of 70 percent and 50 percent, respectively, in a standard clinical setting.Reference Honakar and Shepard5
This study therefore aimed to assess possible environmental factors that may influence the reliability of the Fukuda stepping test and to explore methods to improve the sensitivity of (or ‘sharpen’) this clinical test.
Materials and methods
Normal healthy individuals under the age of 45 years and free of musculoskeletal, neurological or visual pathology were invited to participate in this study. Those with current symptoms or a history of dizziness or vertigo were excluded. All participants underwent pure tone audiography to confirm bilateral hearing thresholds of less than 20 dB HL at 0.25, 0.5, 1, 2, 4 and 8 kHz. Informed verbal consent was obtained from all participants.
Each participant was asked to march on the spot with their eyes closed and arms outstretched. After 50 steps, the extent of their rotation and displacement was recorded and participants returned to their starting point (see Figure 1). Each participant was tested in both a standard clinic room and a soundproofed anechoic room under the following randomised conditions: standing on the floor, standing on foam, with or without industrial ear defenders, and in the presence or absence of a sound-localising source (the ‘Mobile Metronome’ smartphone application set to 120 beats per minute and placed at the 0° azimuth).
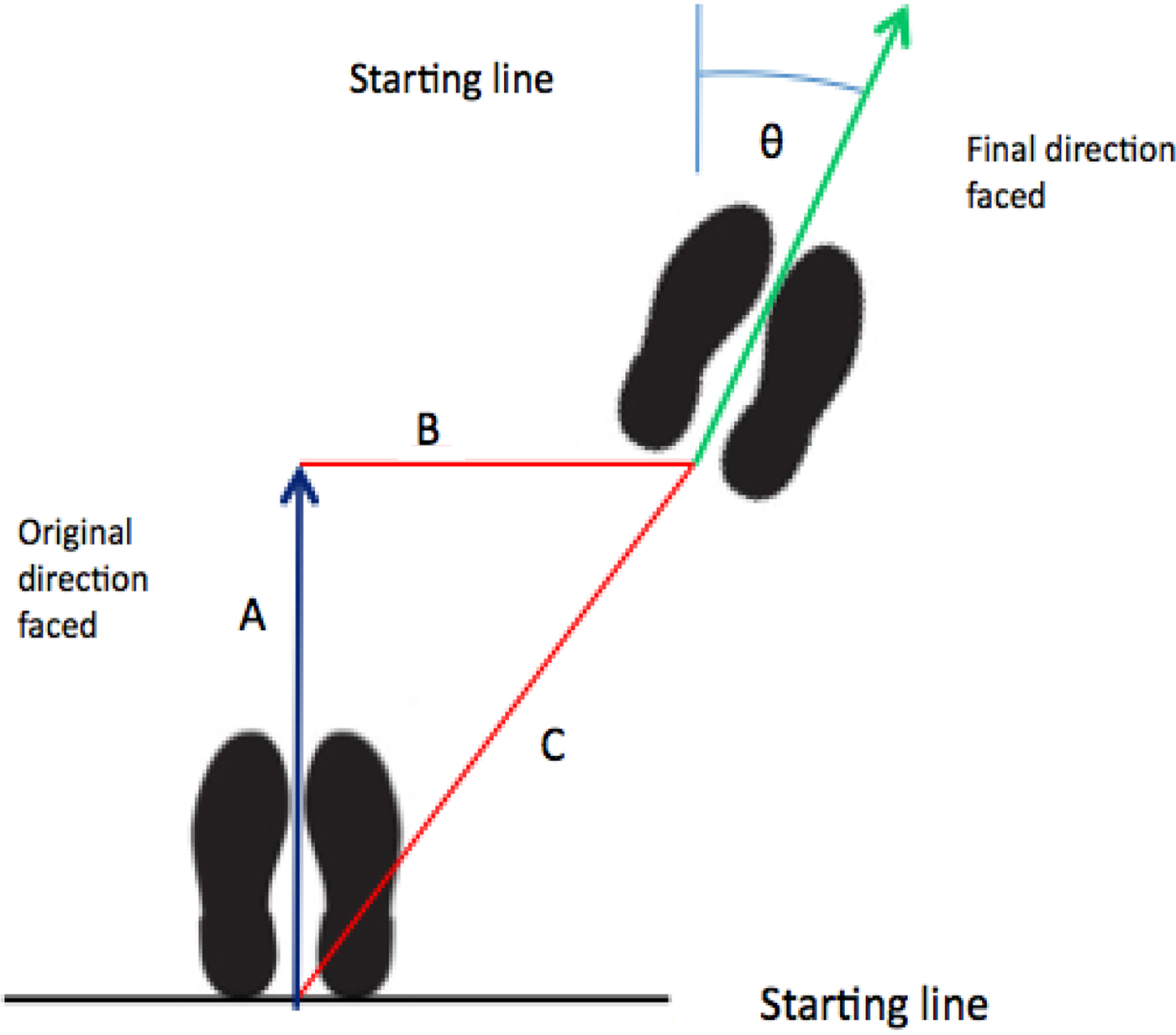
Fig. 1 The Fukuda stepping test was performed and extent of rotation and displacement calculated using a plumb-line held at the subject's fingertips, a rule and protractor. A = the amount of forward displacement; B = the amount of lateral displacement; C = the total amount of displacement; Θ = the final amount of rotation from the original direction faced
Data was entered into an Excel™ spreadsheet, and environments and conditions were compared using a paired t-test. A p-value of less than 0.05 was taken to indicate statistical significance.
Results
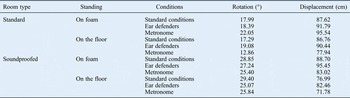
Forty-four patients with a mean age of 26.0 years (range 20–43 years) were eligible for inclusion in this study (22 males and 22 females). Comparisons of the effects of different environmental variables are shown in Tables I and II (p-values), with standard deviations shown in Table III.
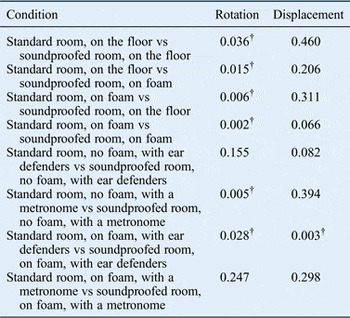
Table I Comparisons of the effects of varying conditions on rotation and displacement in standard and anechoic rooms

*p-values; †p > 0.05.
Table III Two standard deviations for rotation and displacement

Rotation
In a standard room, participants provided with a metronome showed a significant reduction in rotation compared with those without (p = 0.012). In a soundproofed room, participants standing on foam and provided with a metronome showed a significant reduction in rotation compared with those without (p = 0.016).
When both rooms were compared, there was a general trend towards increased rotation in the soundproofed room under all test conditions. Significant differences in the degree of rotation of participants were observed under the following conditions: a standard room on the floor versus a soundproofed room on the floor (p = 0.036); a standard room on the floor versus a soundproofed room on foam (p = 0.015); a standard room on the floor with a metronome versus a soundproofed room on the floor with a metronome (p = 0.005); and a standard room on foam with ear defenders versus a soundproofed room on foam with ear defenders (p = 0.028) (Table II).
Displacement
Displacement, i.e. the distance moved by participants from their starting point, was less consistently influenced by environment and by the conditions applied during testing. For participants standing on the floor in the standard room, there was significantly less rotation for those with ear defenders compared with those without (p = 0.022), and for those with a metronome compared with those without (p = 0.027). For participants standing on foam in the soundproofed room, there was significantly less rotation for those with a metronome compared with those without (p = 0.019).
A comparison of the effects of different rooms on the rotation of participants standing on foam with ear defenders revealed significantly less rotation for those in the soundproofed room (p = 0.003; Table II).
Discussion
Assessment and subsequent treatment of the dizzy patient requires a full clinical evaluation supported, where necessary, by audiovestibular testing and imaging.Reference Grommes and Conway3 The Fukuda stepping test forms part of the formal clinical assessment, with rotation in a particular direction suggesting a peripheral vestibular deficit on the ipsilateral side.Reference Unterberger4 No single clinical test should be taken in isolation, but should instead be performed in conjunction with appropriate additional tests. However, the Fukuda stepping test is commonly performed alone; it is anecdotally reported to be the only test of peripheral vestibular function known to primary care physicians.
Previous studies have suggested that postural control and sway may be influenced by a variety of factors including tactile sensations, mental tasks and, more recently, auditory information.Reference Kanegaonkar, Amin and Clarke1, Reference Tremblay, Mireault, Dessureault, Manning and Sveistrup6, Reference Predo, Stoffregen and Duarte7 Our study supports the concept that auditory cues influence spatial awareness and hence influence the extent of rotation observed during this clinical test. The extent of both rotation and displacement was greater in a soundproofed room compared with in a standard room, but was significantly lower when participants were concomitantly exposed to a sound-localising source (in this study, a metronome).
The results of this study have a number of clinical implications. The first is the need for standardisation of the Fukuda stepping test. This should include the use of an environment devoid of auditory cues which may act as a sound-localising source. In clinical practice, this may require removing a clock, fan or telephone, and performing this test in silence. Our results also suggest that variations in the extent of rotation were greater in a soundproofed room than in a standard clinic room, and also on foam rather than on the floor. Hence, these conditions deserve further investigation as they may be used to ‘sharpen’ the test and hence ‘unmask’ a peripheral vestibular deficit. Additional studies are required to validate these environmental effects and generate appropriate normal values for rotation. Moreover, our literature review suggests a need for standardising the Fukuda stepping test regarding the number of steps performed. This has varied in previous reports, and is occasionally substituted by a time interval (e.g. 30 seconds).Reference Fukuda8–Reference Morrison and Harris10
A valid criticism of this study is the small number of individuals recruited. We hope to recruit a larger cohort of normal participants in the future to strengthen the normative values generated. This may establish a valuable normal range and provide a threshold value of rotation to suggest the presence of a peripheral vestibular deficit. Another limitation is that the participants did not undergo formal vestibular testing, although they were carefully screened and those with a history of dizziness or vertigo were excluded. A further limitation was the exclusion of patients with a documented peripheral vestibular deficit; further research is needed to investigate the effects of modifying the Fukuda stepping test for these patients.
The method used to accurately record the extent of participant rotation during this study proved to be time-consuming, but paralleled those of previous studies.Reference Fukuda8, Reference Hickey, Ford, Buckley and Fitzgerald O'Connor11 This method is, however, seldom used clinically. A recent unpublished study performed in our department suggests considerable inter-observer variation when the extent of rotation is only estimated (not measured), which may affect the reliability of the test.Reference Whittaker, Mathew, Kanani and Kanegaonkar12 We recently explored this possibility by developing a smartphone application (‘D + R Balance’) that records both the extent of rotation and sway.
• The Fukuda stepping test is commonly used to assess peripheral vestibular function
• Its maximal sensitivity and specificity are 70 per cent and 50 per cent, respectively
• Measuring both rotation and displacement may be clinically useful
• The test may be ‘sharpened’ by marching on foam or in a soundproofed room
The direction of rotation was not recorded because our cohort consisted of normal healthy individuals. Although one might expect a patient with a peripheral vestibular deficit to rotate towards the side of loss, this is not always the case; previous studies have suggested the specificity of this test to be in the region of 50 per cent.Reference Honakar and Shepard5, Reference Jacobson and Shepard13 Additional research into assessing patients by exploring the environmental variables described in this study is required. These variables may also influence the direction of rotation, although this may be influenced by a number of factors. Some previous studies have suggested a link between the direction of rotation and the handedness of participants, with participants rotating in the opposite direction to that of their dominant hand or foot. However, other studies found no conclusive link between handedness and the direction of rotation in the Fukuda stepping test.Reference Kuipers-Upmeijer and Oosterhuis14
Conclusion
This study suggests that a variety of factors influence the degree of rotation seen in Fukuda stepping testing in normal participants, and that measuring both rotation and displacement may be clinically useful, as both are similarly affected by alterations to Fukuda stepping test conditions.
The test may be ‘sharpened’ by marching on foam or by being performed in a soundproofed room. The presence of a localising environmental sound may influence the extent of rotation and hence potentially mask an underlying unilateral peripheral vestibular deficit. These variables may merit further evaluation in both normal individuals and patients with peripheral vestibular hypofunction to assess their effect on the sensitivity of this common clinical examination.