Introduction
Meditation has been extensively practiced in many civilizations for thousands of years as a means of transcending the common state of consciousness for well-being and religious purposes (Braboszcz et al. Reference Braboszcz, Hahusseau, Delorme and Carlstedt2010). In the recent times, meditation is used as a generic term to refer to a wide range of practices for self-regulation of emotion and attention (Gunaratana, Reference Gunaratana2002). It is very difficult to define meditation as it can both be a traditional and clinical entity. Encompassing both parts, Cardoso et al. (Reference Cardoso, de Souza, Camano and Leite2004) developed an operational definition of meditation as any practice that (a) utilizes a specific and clearly defined technique, (b) involves muscle relaxation somewhere during the process, (c) involves logic relaxation (i.e. not ‘to intend’ to analyze the possible psychophysical effects, not ‘to intend’ to judge the possible results, not ‘to intend’ to create any type of expectation regarding the process), (d) a self-induced state, and (e) the use of a self-focus skill or ‘anchor’ for attention (Cardoso et al. Reference Cardoso, de Souza, Camano and Leite2004). This can be done either by focusing on the flow of psychic content, rather than on the content itself, or by concentrating on a single stimulus like a mantra or the breath. The former is widely known as mindfulness-based meditation, whereas the latter is called transcendental meditation (Hussain & Bhushan, Reference Hussain and Bhushan2010). However, a meta-analysis of a large sample of studies has divided the meditation into five broad categories of practices, that is, Mantra Meditation, Mindfulness Meditation, Yoga, Tai Chi, and Qigong (Ospina et al. Reference Ospina, Bond, Karkhaneh, Buscemi, Dryden, Barnes, Carlson, Dusek and Shannahoff-Khalsa2008).
There is a significant role of meditation in the treatment of chronic illnesses like chronic pain, insomnia, and hypertension. Mindfulness meditation has been successfully integrated with psychotherapy, for example, Dialectical Behavior Therapy. It is also regarded as beneficial in various psychiatric illnesses like anxiety disorders, mood disorders, sleep disorders, Attention-Deficit/Hyperactivity Disorder, substance use disorders, and suicidality (McGee, Reference McGee2008). However, meditation has also been linked to psychosis (Baena Mures et al. Reference Baena Mures, Niell Galmes, Lázaro Pascual and Gonzalez2016; García-Albea et al. Reference García-Albea, González-Vives, Tejeira, López-Ibor and López-Ibor2012; Lim & Lin, Reference Lim and Lin1996; Lu & Pierre, Reference Lu and Pierre2007). Morita gave the first description of psychotic symptoms related to meditation in 1915, reporting that it occurred mainly in superstitious people with low educational levels and was a culture-specific disorder (Nakaya & Ohmori, Reference Nakaya and Ohmori2010). Linden et al. (Reference Linden, Harris, Whitaker and Healy2010) reviewed all case notes of patients admitted to the North Wales Hospital between 1902 and 1907 (around Welsh religious revival of 1904–1905) and found a significant increase in admissions for brief polymorphic psychoses in the revival years, but the number of first admissions for other psychiatric disorders did not change (Linden et al. Reference Linden, Harris, Whitaker and Healy2010).
There is ample literature on the benefits of meditation, including mindfulness-based practices. However, evidence is limited on the potential harms, especially when it is practiced in a clinical setting as opposed to contemplative practice. While it is important to study the harmful effects of pharmacotherapy and psychotherapy, similarly it is worth investigating the risks associated with meditative practices also. There are few reasons to explore the risks associated with meditative practice. Clinicians have a duty to follow the ethical principle of non-maleficence. If we have the knowledge of the possible harm due to meditation, then it could help improve its effectiveness. Meditation in contemplative tradition as well as in clinical settings has been described to be associated with some psychological problems like depressive symptoms, anxiety symptoms, dissociative symptoms, psychotic symptoms, and suicidal ideation (Baer et al. Reference Baer, Crane, Miller and Kuyken2019).
It has been suggested that there is an association between psychosis and meditation, but the empirical evidence is sparse as it is very difficult to investigate it in cross-sectional samples and requires longitudinal observation. In this review, we aim to explore the possibility of an association between occurrence of psychosis and meditation.
Methodology
The guidelines for systematic and structured search were employed for the literature search (Moher et al. Reference Moher, Liberati, Tetzlaff and Altman2009). Major medical, health, and psychological literature databases including PubMed, Cochrane Database for Systematic Reviews, Scopus, EMBASE, CINAHL, and PsycINFO were used, and the search was made from the inception till 31 May 2018. The keywords used for the systematic search were: ‘Psychosis’ AND ‘Meditation’, ‘Psychotic Symptoms’ AND ‘Meditation’, ‘Schizophrenia’ AND ‘Meditation.’ All studies (cross-sectional, case-control, and cohort) conducted in any population consisting of any age group that reported the relationship between psychosis and meditation were considered eligible for the present review. Exclusion criteria included reviews, opinions, and editorials, although their reference lists were searched for any studies not retrieved by the electronic search. Additionally, any non-English language studies were excluded. After completing the electronic database search, titles and abstracts of the identified articles were assessed for their suitability to be included in the review. Additional searches were also conducted in other ‘grey’ literature databases such as Google Scholar. After assessing the titles and abstracts, the full text of the articles deemed suitable was retrieved for further examination of the contents of the studies to determine their final inclusion in the review. Furthermore, the reference lists of the selected articles were also examined for additional suitable publications that might have been overlooked in the previous search. Data extraction was carried out under the following headings (as applicable): type and duration of meditation, risk factors, type and duration of psychosis, associated affective symptoms, sample size, and study design. Two authors (PS and AM) independently carried out data extraction. Results were compared, and any discrepancies were resolved by mutual consensus. Supplemental Table 1 contains a detailed description of all the articles in this review.
Results
The initial search led to 856 studies from all the databases, and the flow chart of the search strategy is summarized in Fig. 1.
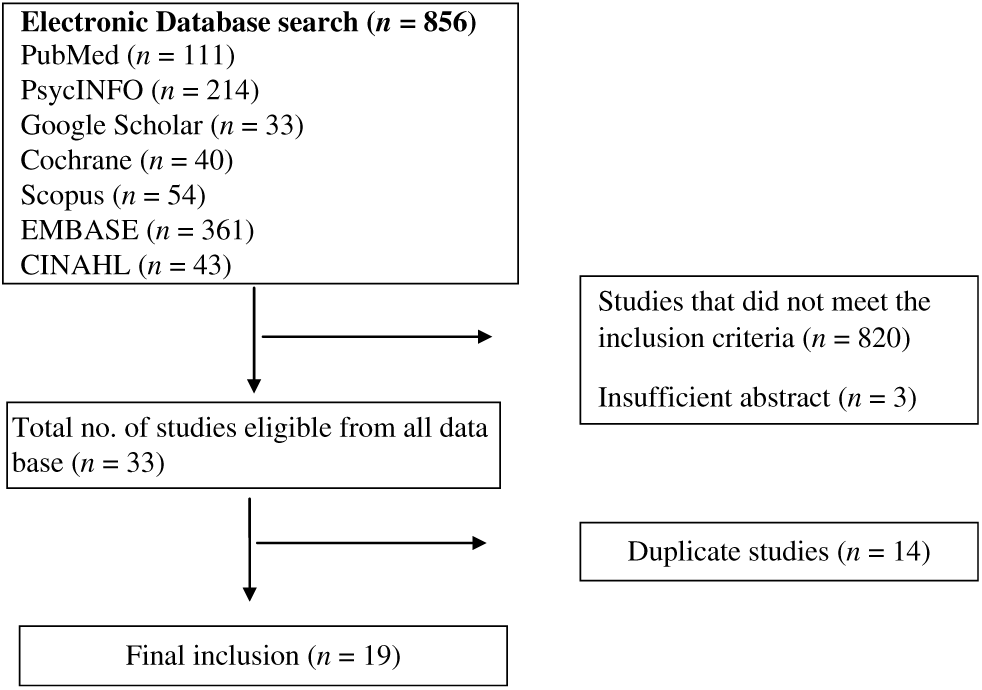
Fig. 1. Flow chart showing search strategy.
All the studies included in this review were either case reports or case series (maximum of three cases) as shown in Supplemental Table 1. The total number of cases from all the studies was 28. The minimum age of the patients described was 18 years, and maximum age was 57 years, with a mean age of 31.13 years (s.d. = 9.63). There was an equal distribution of males and females (14 each). The cases included in this review had performed meditation in a non-clinical setting and were brought to the clinical attention after occurrence of behavioral problems. All the cases were retrospectively reported by the respective authors. Hence, some caution is necessary while interpreting the association between practice of meditation and onset of psychosis. Different types of meditation were described among studies. However, none of the studies described the method of meditation. The types of meditation described were Transcendent, Mindfulness, Buddhist Meditation like Qigong, Zen, Theraveda, and others like Bikram Yoga, Pranic Healing, and Hindustan Type Meditation. The studies also mentioned non-specific meditations like walking meditation, chanting sutras, diffuse meditation, and camps. Different cases were described performing different durations of meditation ranging from few days to several years. Fourteen out of twenty-eight cases had certain precipitating factors like insomnia, lack of food intake, history of mental illness, stress, and psychoactive substance use. The diagnoses included acute psychosis in 14 cases, schizophrenia in 7 cases, mania with psychotic symptoms in 3 cases, and schizoaffective disorder in 1 case. Two cases had psychosis with depersonalization as a core feature characterized by autoscopic hallucination. It is notable that six cases had affective symptoms. However, in one of the cases, no diagnosis was mentioned. The duration of psychosis ranged from a very brief episode for seconds to longer duration of years. Nine out of twenty-eight cases had previous history of psychiatric illness. The cases included in the review had very heterogeneous presentations, such as transient psychotic symptoms, an affective disorder with psychotic symptoms, schizophrenic symptoms, and symptoms of schizoaffective disorder.
Discussion
Throughout the literature, we could find only a handful of cases where intense meditation was followed by psychotic symptoms, that is, temporal correlation between meditation and onset of symptoms suggesting some degree of association (Kiene et al. Reference Kiene, Hamre and Kienle2013). Meditation leads to complex neurochemical changes in the brain (Rubia, Reference Rubia2009). There is an increased level of neurochemicals like dopamine, serotonin (5-hydroxytryptamine or 5-HT), melatonin, acetylcholine, glutamate, N-acetylaspartylglutamic acid (NAAG), gamma-aminobutyric acid, dimethyltryptamine (DMT) and a decrease of noradrenaline, cortisol, and corticotropin-releasing hormone at the central level (Mohandas, Reference Mohandas2008). It also leads to increased cerebral blood flow in the specific brain areas like frontal lobe, pre-frontal cortex (PFC), thalamus, hippocampus, hypothalamus, and cingulate gyrus (Newberg & Iversen, Reference Newberg and Iversen2003; Monti & Beitman, Reference Monti and Beitman2010; Deepeshwar et al. Reference Deepeshwar, Vinchurkar, Visweswaraiah and Nagendra2015). The altered states of consciousness seen during certain meditation practices are principally due to transient PFC deregulation (Dietrich, Reference Dietrich2003). Similar findings are seen in the patients with schizophrenia regarding synaptic connectivity and neuronal thickness of PFC (Lewis & Lieberman, Reference Lewis and Lieberman2000). A variety of schizophrenia-like effects are associated with these complex neurochemical changes. Different hypotheses have been laid on how meditation could induce psychotic states. Some of the mechanisms proposed in relation to increased 5-HT2 receptor activation, increased 5-methoxyDMT, increased NAAG, and increased dopamine. The mechanisms include the 5-HT inhibition of Lateral Geniculate Body, the hallucinogenic effects of DMT, the dissociative hallucinogenic effects of NAAG, and the action of increased dopamine in the temporal lobe (Mohandas, Reference Mohandas2008).
It has been suggested that meditation should be contraindicated in people suffering from psychiatric illnesses such as psychosis (Shapiro, Reference Shapiro1994). However, looking at the evidence, one could find that meditation combined with yoga has been shown to have positive effects on negative symptoms of schizophrenia (Visceglia & Lewis, Reference Visceglia and Lewis2011). A meta-analysis of 13 studies (n = 468) has shown mindfulness-based practices to be moderately beneficial in treating negative symptoms and could be used as an adjunct for pharmacotherapy (Khoury et al. Reference Khoury, Lecomte, Gaudiano and Paquin2013). Similarly, studies also support that mindfulness-based intervention techniques are helpful in decreasing anxiety in patients with psychosis (Davis & Hayes, Reference Davis and Hayes2011). The practices that have a positive effect in different spheres of psychosis involve mindfulness meditation which is a practice in which one would accept and anchor his/her concentration in the present moment while attending to the natural flow of breathing (Shonin et al. Reference Shonin, Van Gordon and Griffiths2013). This is different from the meditation practiced by most of the cases where patients would be engrossed in chanting ‘mantras’ and trying to get into the altered state of mind, indicating that transcendental meditation could be more psychosis-prone as compared with mindfulness-based practice (Sharma et al. Reference Sharma, Singh, Gnanavel and Kumar2016). Hence, there is a clear need to delineate between traditional meditation practices and therapist guided meditation-based interventions practiced in a clinical setting in order to explore their role on the trajectories of outcome in patients suffering from psychosis.
Most of the patients described in this review who experienced psychotic episode precipitated by meditation attended intensive meditation retreats rather than practicing brief mindfulness interventions. Some of the patients also had previous history of psychiatric illness which could have contributed to their risk of developing psychosis. Adverse effects of meditation are confounded by factors such as sensory deprivation, loss of sleep, and fasting, all of which may serve as precipitants for a psychotic episode. Various other factors which could have played a confounding role such as history of substance use, family history of psychosis, traumatic life events in the past, presence of neurological illness such as seizure disorder, and use of medicines known to precipitate psychosis have not been taken into account in these reports. Another possibility is that the behavioral changes, such as meditation in somebody who has no prior history of doing so, could be considered a manifestation of psychosis at risk state when accompanied by other attenuated symptoms in a person who subsequently develops a psychotic illness. Retrospective nature of the case reports is subject to recall bias. Thus, it is difficult to interpret the direct nature of the relationship between meditation and adverse outcomes based on the studies mentioned in our review. The data analyzed in this paper have been collected from the case reports and case studies which are insufficient to establish a causal association between a specific type of meditative practice and development of psychosis. Lack of longitudinal follow-up, marked heterogeneity in the type of meditation used, and patient profile further limit their comparability.
Regarding conducting research in this area, the greatest limitation lies in the sheer impracticability of directly and systematically investigating meditation-induced harm. Few published reviews have compiled studies employing different methods (viz., case descriptions, cross-sectional interviews, online survey) to study the ill effects associated with meditation (Van Gordon et al. Reference Van Gordon, Shonin and Garcia-Campayo2017; Baer et al. Reference Baer, Crane, Miller and Kuyken2019). A close look at these studies clearly reveals the lack of robust methodology used and hence limits the conclusions one can draw from them.
A cautious approach to using meditation in research is warranted in the face of limited and preliminary nature of the current evidence to maximize participant safety. Some of the general guidelines for patients with psychosis practicing mindfulness-based meditation include engaging only in brief sessions, avoiding deep concentration, and guided sessions using a soft voice or audio tapes, involvement of experienced facilitators, small groups with possibility of one-to-one discussion avoiding explicitly analytical/insight-based (i.e. Vipassana) meditation techniques, etc. (Pérez-Alvarez et al. Reference Pérez-Alvarez, García-Montes, Perona-Garcelán and Vallina-Fernández2008; Shonin et al. Reference Shonin, Van Gordon and Griffiths2013). Apart from this, other non-meditative mindfulness-based techniques have been shown to be effective in depressive symptoms among patients with schizophrenia (Moritz et al. Reference Moritz, Cludius, Hottenrott, Schneider, Saathoff, Kuelz and Gallinat2015). Mindfulness involves intentionally bringing one’s attention to the internal and external experiences occurring in the present moment and is often taught through a variety of exercises (Baer, Reference Baer2003). Although, mindfulness originated from eastern meditative practices, western researchers and clinicians who have introduced mindfulness practice into mental health treatment programs usually teach these skills independent of meditative states as described in religious and cultural traditions of their origins (Kabat-Zinn, Reference Kabat-Zinn1982). A systematic review (Aust & Bradshaw, Reference Aust and Bradshaw2017) of mindfulness interventions for psychosis has shown that they can be safely used by patients with some therapeutic benefits compared to routine care. However, it also highlighted the limitations due to heterogeneity in the designs, interventions, and outcome measures used in the studies included. There is evidence that group-based mindfulness training is feasible and can improve clinical functioning as per the study done in 22 participants (Chadwick et al. Reference Chadwick, Hughes, Russell, Russell and Dagnan2009). Similarly, a study that examined the relationship between schizotypy and mindfulness concluded that mindfulness practice is not associated with an overall increase in schizotypal traits (Antonova et al. Reference Antonova, Amaratunga, Wright, Ettinger and Kumari2016). The pattern in the participants suggested that mindfulness meditation may help to reduce suspiciousness and excessive social anxiety via emphasis on awareness, non-judgment, and non-reactivity while meditating. Mindfulness practices may reduce the distress associated with psychotic symptoms such as voices, images, and intrusive thoughts by helping patients learn alternative ways of relating to their troubling experiences. The evidence from small data sets concludes that patients with active psychotic symptoms can tolerate short sitting meditations, reflect on these experiences, and relate these to experiences in their everyday lives (Jacobsen et al. Reference Jacobsen, Morris, Johns and Hodkinson2011). The studies that show the benefits of meditation in psychosis have only implicated mindfulness-based meditation and with small sample sizes. There is no literature base for benefits of other types of meditation techniques like Qigong, Transcendental, Zen, etc. in psychosis. A conclusion can be made from the findings that mindfulness-based and other meditation interventions tailored to a clinical setting are generally safe in depression and anxiety patients. A meta-analysis by Khoury et al. (Reference Khoury, Lecomte, Gaudiano and Paquin2013) found brief mindfulness interventions to be safe in patients with psychosis. However, there is a need to tailor the meditation practice to the individual patient, for example, determining the duration of meditation intervention. Hence, future research should investigate the most effective format for its delivery (e.g. number of weeks, open v. closed groups, running mixed staff/participant groups) using standardized measures, as well as mechanisms of change and connections to cognitive theory, and systematically record adverse events relating to the intervention.
Conclusion
There is a good level of evidence that mindfulness-based interventions are beneficial for some symptoms of psychosis; however, some of these interventions do not have good quality evidence relating to the frequency or nature of associated adverse events. It is possible that meditation may be harmful to vulnerable individuals, for example, those with predisposing factors for psychosis. It is necessary to distinguish between clinical and non-clinical samples when considering research subjects in view of the varying risk factors in these two populations. Currently, there are several limitations in the existing literature that make it difficult to draw firm conclusions as to any causal relationship between meditative practice and psychosis. Future research in this area should consider longitudinal follow-up studies or naturalistic studies to further explore a potentially causal role of meditation in the development of psychosis. Since meditative practices are deeply intertwined with various socio-cultural, religious, and transcultural factors, therefore, they should also be taken in consideration when considering research in this area. Since heterogeneity is one of the most important factors which limit the interpretation of current evidence, there is a need for specific operational criteria defining particular meditative practices at the very outset. Similarly, there is a need for interventions based on meditative practice to report more consistently on associated adverse events and to apply careful patient selection criteria. Ultimately, the decision to offer a meditation-based intervention should be based upon careful weighing of the potential risks and benefits of that intervention on an individual basis.
Supplementary Materials
For supplementary material for this article, please visit https://doi.org/10.1017/ipm.2019.47
Financial Support
This research received no specific grant from any funding agency, commercial, or not-for-profit sectors.
Conflicts of Interest
None.
Ethical Standards
The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional committee on human experimentation with the Helsinki Declaration of 1975, as revised in 2008. The authors assert that ethical approval for publication of this review was not required by our local Research Ethics Committee (REC).



