Introduction
Tonsillectomy continues to be one of the most common procedures performed by otolaryngologists in recent years.Reference Timms and Temple1 All tonsillectomy techniques share the characteristic of producing an avulsion wound which exposes the underlying tissues to the environment of the oropharynx and which requires extensive healing by secondary intention.Reference Back, Paloheimo and Ylikoski2, Reference Volk, Wang, Pankratov, Perrault, Ingrams and Shapshay3 The open tonsillar fossae quickly become covered by inflammatory exudate, which will be gradually replaced by ingrowth of granulation tissue and mucosal creeping during the second week of recovery.Reference Wexler4
Such a healing pattern is often associated with post-operative morbidity, particularly pain and delayed haemorrhage. The pain is the result of disruption of mucosa and exposure of glossopharyngeal nerve endings, followed by inflammation and spasm of the pharyngeal muscles, which leads to ischaemia and a protracted cycle of pain.Reference Dempster5 Several reports identified the amount of tissue necrosis (associated with the surgical procedure) and the presence of post-operative infection as the principle factors affecting the healing outcome following tonsillectomy.Reference Telian, Handler, Fleisher, Baranak, Wetmore and Potsic6, Reference Gillis and Strong7
We undertook the current study in order to evaluate the potential correlation between pre-operatively diagnosed laryngopharyngeal reflux (LPR) and post-operative healing of the tonsillar fossae following tonsillectomy, based on subjective and objective findings.
Materials and methods
Patients and inclusion criteria
This study was constructed as a prospective, blinded, case–control study and included adult patients scheduled for tonsillectomy at the department of otorhinolaryngology – head and neck surgery, Alexandria University, between September 2003 and June 2005. All patients had a history of recurrent tonsillitis and/or evidence of obstructive tonsillar hypertrophy. Prior to enrolment, potential subjects underwent full routine pre-operative laboratory investigations, in order to exclude patients with concomitant medical problems which could affect healing (such as diabetes mellitus, anaemia or bleeding disorders). Patients with a prior history of peri-tonsillar abscess or those who had suffered an acute attack of tonsillitis within two weeks prior to the operation were also excluded.
The recruitment of subjects was conducted completely independently of any symptoms suggestive of LPR, in order to avoid selection bias. Patients who had received anti-reflux medication during the past three months were excluded from the study.
The nature of the study was explained to the patients, and written, informed consent was obtained from each patient prior to his/her enlistment.
Methods
pH monitoring
Ambulatory 24-hour pH monitoring was performed using the pH-response system (Medtronic, Xomed, Jacksonville, Florida, USA). Initially, the location of the lower and upper oesophageal sphincters was identified, either by oesophageal manometry or by direct endoscopic visualisation. The dual-site pH catheter, with two pH sensors spaced 10 cm apart, was calibrated in buffer solutions of pH 7 and pH 1 before each study.
A topical solution of adrenaline and xylocaine was applied intranasally before pH catheter placement. The distal probe was placed in the distal oesophagus 5 cm above the lower oesophageal sphincter. The proximal probe was positioned under flexible endoscopic guidance 1.5–2 cm above the upper oesophageal sphincter, just behind the laryngeal inlet. The catheter was then secured to the nose with adhesive tape, and the patient was instructed to continue their daily activities.
Carbonated and caffeinated beverages were restricted during the study, and patients documented on a diary card the starting and ending times of meals, sleep, supine periods, heartburn and regurgitation, and any other significant symptoms. The pH catheter was removed 24 hours after placement and the data from the DigitrapperTM were uploaded into a computer and analysed.
Laryngopharyngeal reflux events were defined as an abrupt proximal electrode pH drop to a nadir of less than pH 4. Patients were identified as having pathological LPR according to the criteria described by Vincent et al.;Reference Vincent, Garrett, Radionoff, Reussner and Stasney8 i.e. seven or more LPR events per 24-hour study period. From the results, patients were divided into two groups: those with LPR (group A, 30 patients) and an equal number of patients without LPR (group B) as a control group.
Surgical procedure
A standardised general anaesthetic technique was used in all patients. Tonsillectomy was initiated by an incision overlying the anterior tonsillar pillar. Blunt dissection proceeded along the tonsillar fossa in the peri-tonsillar plane, keeping as close to the tonsillar capsule as possible. Haemostasis was achieved by pressure packing, and any persistent bleeding was controlled using suture ligation without the use of electrocautery. Post-operatively, all patients stayed in the hospital for a few hours and were discharged on the same day. They were given routine post-tonsillectomy instructions regarding diet, activity, pain and fever. All patients were prescribed a standard regimen of oral amoxicillin–clavulanic acid (in a dose determined by the patient's weight) and coated paracetamol tablets every six hours. Patients allergic to penicillin were given an oral second generation cephalosporin.
Outcome measures
In order to assess post-operative pain, patients were asked to rate their pain severity on the seventh, 14th and 21st post-operative days, using a visual analogue score from zero to 10, with zero representing no pain and 10 representing the highest possible pain score. Patients were to mark their level of pain on the scale first thing each morning, before taking any pain medication or eating breakfast. Patients were also asked: (Reference Timms and Temple1) when did you resume your normal diet, and (Reference Back, Paloheimo and Ylikoski2) when did you resume your usual daily activities? Patients were instructed to consider a normal diet as one which included types and amounts of food such that another family member would not be able to recognise that the patient had undergone throat surgery. Similarly, usual activities were considered to be of the same type and duration as before surgery (even if still associated with fatigue).Reference Wexler4
In order to assess tonsillar fossae healing pattern, patients were seen on the seventh and 14th post-operative days by a single surgeon who was neither involved in the tonsillectomy procedures nor aware of the two studied groups. These dates were selected for time-serial comparison of the two groups, in order to evaluate the effect of LPR on the early inflammatory and the late proliferative phases of wound healing.Reference Witte and Barbul9 The size of the post-tonsillectomy slough was taken as an arbitrary indication of the rate of the healing process. As previously described by several authors,Reference Timms and Temple1, Reference Noordzij and Affleck10 five grades of healing were considered: 0, 25, 50, 75 and 100 per cent, according to the size of the slough in comparison with the aerial size of the original post-operative bed, where 0 per cent represented a bed completely covered with slough and 100 per cent represented a totally healed bed (Figure 1). The lower grade was selected in case of inequality between both sides. The two groups were compared and the correlation between the degree of LPR and the rate of post-operative healing was evaluated.
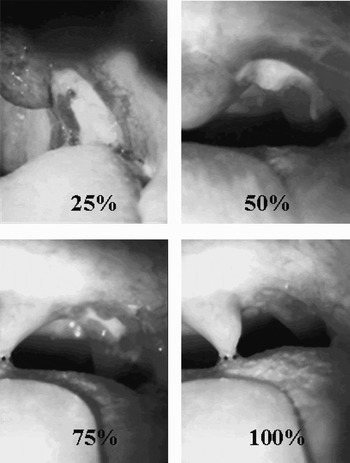
Fig. 1 Rate of healing, as determined by size of post-tonsillectomy slough. 25% = slough covers 75% of tonsillar bed; 50% = slough covers 50% of tonsillar bed; 75% = slough covers 25% of tonsillar bed; 100% = no slough (i.e. complete healing).
Ethical considerations
The study protocol was approved by the ethics committee of the medical faculty, Alexandria University, Alexandria, Egypt.
Results and analysis
Statistical analysis
All documented data were analysed using the Statistical Package for the Social Sciences software (SPSS Inc, Chicago, Illinois, USA). Categorical variables were analysed using the chi-square test or Fisher's exact test. Comparison of the mean age in the two groups was performed using the unpaired t-test. The difference between the two groups with respect to their post-operative pain scores was analysed using the Mann–Whitney U test, and that regarding time to resumption of normal diet and activity using the t-test. Pearson correlation analysis was employed to detect potential correlation between the degree of slough and the number of pharyngeal reflux episodes. A value of p < 0.05 was selected as the desired significance level.
Demographic data
Group A (i.e. LPR) included 21 males and nine females, with an age range of 16–29 years (mean 21.2 ± 3.27). Group B (i.e. no LPR) included 23 males and seven females, with an age range of 15–33 years (mean 21.8 ± 5.25). Both groups were well matched for age and sex (p = 0.62 and p = 0.56, respectively).
Surgical indications
In group A, the primary surgical indication was recurrent tonsillitis in 26 patients and obstructive tonsillar hypertrophy in four. Group B included 28 patients with recurrent tonsillitis and only two with obstructive tonsillar hypertrophy. The difference between the two groups was found to be statistically insignificant (p = 0.67).
Post-operative pain
The mean values and ranges of the post-operative pain scores for the two groups are shown in Table I. On the seventh and 14th post-operative days, group A had significantly higher pain scores compared with group B. Only three patients from group A continued to report mild pain (scored two to three) on the 21st post-operative day. The time taken to return to a normal eating routine was significantly less for those patients without LPR. However, there was no significant difference between the two groups in terms of mean number of days after operation before normal activities were resumed (Table II).
Table I Patients' pain scores on 7th and 14th post-operative days

* Statistically significant. Post-op = post-operative; SD = standard deviation
Table II Patients' time to resumption of normal diet and activities

* Statistically significant. SD = standard deviation
Healing rate
The grades of post-operative tonsillar fossa healing observed in both groups on the seventh and 14th post-operative days are shown in Table III. None of the patients showed total coverage of the tonsillar fossae with slough at the two evaluation appointments. Comparison of the two studied groups showed significantly slower healing among group A patients compared with group B patients, both on the seventh and 14th post-operative days (p = 0.016 and p = 0.029, respectively).
Table III Patients by grade of healing, on 7th and 14th post-operative days

* p = 0.016; †p = 0.029; both statistically significant. Both groups contained 30 subjects.
In group A patients, the mean number of LPR episodes below pH 4 was 25.5 ± 12.1 (range 9–53). Pearson correlation analysis revealed a significant correlation between the number of pharyngeal reflux episodes and the degree of post-operative slough on the seventh and 14th post-operative days (p = 0.0271 and p = 0.0139, respectively).
Discussion
Since the first contribution by Koufman,Reference Koufman11 laryngopharyngeal reflux has been increasingly implicated in the pathogenesis of several otolaryngological disorders, including chronic posterior laryngitis, vocal fold nodules, paroxysmal laryngospasm, Reinke's oedema, laryngeal ulcer and granuloma, as well as globus sensation.Reference Koufman, Amin and Panetti12, Reference Toohill and Kuhn13 To our knowledge, ours is the first study to address the potential correlation between the presence of LPR and the healing outcome of tonsillectomy surgery. In this study, we used ambulatory 24-hour pH monitoring, which is still considered the gold standard test for LPR, in order to identify patients with LPR. The results of the study clearly show that LPR was associated with significantly higher post-operative pain scores and delayed healing of the tonsillar fossae. This negative impact of LPR on wound healing was previously reported in patients undergoing endonasal sinus surgery and in experimental animals after inflicting posterior subglottic injury.Reference Kleemann, Nofz, Plank and Schlottmann14, Reference Roh, Lee and Park15
In contrast to the oesophageal mucosa when faced with gastroesophageal reflux, the pharyngeal, laryngeal and tracheo-bronchial mucosa are not suited to withstand even brief exposure to gastric refluxate, with its content of acid, pepsin, bile and pancreatic enzymes.Reference Koufman11 The susceptibility of these anatomical structures to reflux-induced injury has been recently attributed to the lack of intrinsic cellular mechanisms that protect against chemical injury.Reference Johnston, Bulmer, Gill, Panetti, Ross and Pearson16
In post-tonsillectomy patients, reconstitution of the tonsillar surface epithelium requires proliferation of undifferentiated epithelial precursors which migrate from the surgical margins onto the granulation tissue and gradually replace the post-operative slough covering the surgical bed.
The higher post-operative pain scores in post-tonsillectomy patients with LPR can be attributed to the irritative effect of the gastric contents on the exposed nerve endings. The delayed healing observed may be due to the proteolytic effect of the gastric refluxate. Pepsin, an acid-activated protease enzyme within the gastric juice, has been shown experimentally to synergise with acid and produce marked damage to oesophageal epithelium, through breaching the epithelial barrier function and thus increasing the tissue's vulnerability to further attack and damage during subsequent episodes of reflux.Reference Tobey, Hosseini, Caymaz-Bor, Wyatt, Orlando and Orlando17 The same principle can be applied to the post-tonsillectomy bed when exposed to gastric refluxate.
This hypothesis is further supported by previous studies using sucralfate as a post-operative medication in patients undergoing tonsillectomy and laser-assisted uvulopalatoplasty operations. Sucralfate proved to be effective in alleviating post-operative pain, through the formation of a protective coat on the surgical bed. It also enhanced epithelialisation through inhibition of pepsin activity, resulting in a cytoprotective effect.Reference Freeman and Markwell18, Reference Kyrmizakis, Papadakis, Bizakis, Velegrakis, Siafakas and Helidonis19
In addition to pain and delayed healing; there is also a risk of post-tonsillectomy haemorrhage in those patients with LPR, because of the proven anti-haemostatic effect of hydrochloric acid and pepsin.Reference Green, Kaplan, Curtis and Levine20
According to the current study, specific peri-operative measures should be planned in order to lessen the negative post-operative impact of LPR on wound healing and recovery from tonsillectomy. These may include dietary modifications, behavioural modifications, and suppression of acid production and activity through the use of drugs. Recommended dietary modifications include: avoidance of certain foods (e.g. fats, coffee, chocolate, alcoholic drinks and tomato products), avoidance of excessive eating during meals, and avoidance of intake of food or drink up to three hours before going to bed. Behavioural modifications comprise avoiding smoking, elevating the head of the bed and avoiding tight clothes around the waist.Reference Koufman11, Reference Moraes-Filho, Cecconello, Gama-Rodrigues, Castro, Henry and Meneghelli21 Drug therapy includes prokinetic agents to speed up oesophageal and gastric emptying, as well as a twice daily, high dose proton pump inhibitor to achieve maximal suppression of acid production.Reference Koufman11, Reference Park, Hicks, Khandwala, Richter, Abelson and Milstein22 The addition of H2 receptor antagonists before bedtime is also recommended in order to overcome nocturnal gastric acid breakthrough.Reference Sato23 These drugs should be commenced at least one week pre-operatively and continue for three months post-operatively, with subsequent clinical evaluation to assess the response to therapy and to determine the maintenance therapy required in order to prevent the development of chronic throat complaints.
• Laryngopharyngeal reflux (LPR) is a condition that is being increasingly recognised in otolaryngology practice
• A negative effect of LPR on wound healing has been recently reported following nasal and laryngeal surgery
• This study investigated a possible effect of LPR on wound healing after tonsillectomy, through a prospective case–control study performed on 60 patients divided into two equal groups, according to their pre-operative LPR status
• Laryngopharyngeal reflux had a significantly negative impact on wound healing after tonsillectomy, as assessed both by subjective patient pain severity self-assessment and by objective rating of the grade of post-operative tonsillar bed slough formation
• Findings suggest that recognition and appropriate management of LPR prior to tonsillectomy can have a positive effect on post-operative recovery
However, certain limitations should be recognised in this study. The outcome measures were based on subjective assessment of post-operative pain scores and on the use of a non-validated measurement of the tonsillar area that was either healed or covered by slough. Although these measures have been previously utilised by several authors to evaluate the different factors that influence post-tonsillectomy healing, a truly objective assessment of the effect of LPR on wound healing following tonsillectomy requires a well designed experimental animal model of tonsillectomy and simulated reflux episodes. Evaluation of the histopathological, immunological and biochemical events within the tonsillar bed following exposure to LPR episodes, and comparison with control specimens, may provide additional information that can confirm our preliminary clinical results.
Conclusion
Our study suggests that wound healing following tonsillectomy can be significantly negatively affected by laryngopharyngeal reflux. This implies that maximum control of reflux would seem desirable, in order to minimise the contamination of the surgical site by the highly inflammatory gastric refluxate.






