Introduction
Diabetic ketoacidosis (DKA) is a dangerous pathophysiological state requiring immediate and complicated intervention.Reference Dhatariya1,Reference Karslioglu French, Donihi and Korytkowski2 Early diagnosis and treatment may decrease morbidity and mortality.Reference Dhatariya1,Reference Karslioglu French, Donihi and Korytkowski2 Diabetic ketoacidosis occurs in the setting of hyperglycemia without an appropriate insulin response, leading to the breakdown of proteins resulting in the development of ketones and an acidotic state.Reference Dhatariya1,Reference Karslioglu French, Donihi and Korytkowski2 Classically, DKA is diagnosed through history and physical exam findings such as altered mental status and increased respiratory rate, as well as laboratory findings including hyperglycemia, decreased blood PH, and ketonuria.Reference Dhatariya1,Reference Karslioglu French, Donihi and Korytkowski2 However, blood gas and other laboratory abnormalities are time consuming and require invasive blood draws as well as hospital-based laboratory equipment.
Prehospital providers commonly obtain point-of-care blood glucose levels (BGLs), but elevated serum glucose may be found in many clinical settings.Reference Villani, Nanayakkara and Ranasinha3 Distinguishing between DKA and less physiologically relevant states could greatly improve care.Reference Holstein, Plaschke, Vogel and Egberts4,Reference Benoit, Kahn and Geller5 Prior studies have shown that exhaled end-tidal carbon dioxide (ETCO2) strongly correlates with acidosis in hospitalized diabetic patients, and may be used to rule out DKA in both adultReference Soleimanpour, Taghiadieh, Niafar, Rahmani, Golzari and Esfanjani6 and pediatricReference Fearon and Steele7,Reference Gilhotra and Porter8 emergency department (ED) populations. End-tidal carbon dioxide is fast, noninvasive, and can be performed easily outside of the hospital. In fact, prehospital ETCO2 has been shown to correlate with in-hospital serum bicarbonate (HCO3) levels and anion gap acidosis.Reference Hunter, Silvestri, Ralls, Bright and Papa9 The hypothesis of this study is that ETCO2 may be used as a predictive tool for DKA in hyperglycemic patients transported by Emergency Medical Services (EMS). Prehospital identification of these patients may reduce time to critical interventions.
Methods
Design and Setting
This is a retrospective cohort study of hyperglycemic patients transported by Orange County Fire Rescue (OCFR; Orlando, Florida USA) to Orlando Regional Medical Center (ORMC; Orlando, Florida USA). Orange County, Florida is an urban/suburban region with a population of approximately 1.2 million individuals. The OCFR is the largest EMS agency in the county, accounting for approximately 60,000 transports annually. The ORMC is a large, urban, tertiary receiving hospital with approximately 100,000 ED visits annually. Principle diagnosis of DKA was defined by discharge diagnosis via International Classification of Disease version 9 (ICD-9) code, rather than quantitative laboratory testing. The institutional review board at Orlando Health (Orlando, Florida USA) approved the study protocol “Relationship between prehospital end-tidal carbon dioxide and hospital outcomes,” protocol ID#11.084.08.
Inclusion criteria consisted of any adult (18 years old or greater) patient transported by OCFR to ORMC with a BGL >200mmol/L and a full set of prehospital vital signs including ETCO2. Vital signs documented by first arriving EMS personnel including respiratory rate, systolic blood pressure (SBP), diastolic blood pressure (DBP), pulse, oxygen saturation (SPO2), and ETCO2 were obtained utilizing LIFEPAK 15 (PhysioControl; Redmond, Washington USA) multi-parameter defibrillator/monitors. Prehospital measurement of ETCO2 is a standard practice in Orange County and is performed by paramedics following protocols; ETCO2 was measured via Microstream (Medtronic; Minneapolis, Minnesota USA) capnography using LIFEPAK 15 devices. Microstream capnography is an ETCO2 sampling method using molecular correlation spectroscopy applicable to non-intubated patients. End-tidal carbon dioxide was recorded when capnographic wave peaks were at a constant end-tidal for three to five respirations, as directed by protocol.
Exclusion criteria included pediatric patients (<18 years old) and patients without available prehospital or hospital records.
Data Collection
Chart review was conducted via a single abstractor trained by principal investigators using a data abstraction form developed for the purpose of the study. The abstractor was blinded to the hypothesis of the study. Prehospital charts were selected via the inclusion criteria above and data were manually linked to in-hospital outcomes identified by medical records. Patient gender, mortality, admission to hospital or intensive care unit (ICU), initial ED vital signs, HCO3 and anion gap levels, and principal diagnosis were obtained from the hospital chart by the blinded abstractor. Subjects with missing hospital data were excluded from the study. Due to the small size of the study and single abstractor, there was no official performance monitoring or interobserver reliability testing.
The primary outcome was the predictive value of prehospital ETCO2 for the diagnosis of DKA. Secondary outcomes included correlation between prehospital ETCO2 and HCO3 and anion gap measured in the ED, as well as the predictive value of other prehospital vital signs for the diagnoses of DKA. Mortality was also measured and patient disposition described as discharge, hospital admission, or ICU admission.
Analysis
Data were described using means and proportions with 95% confidence intervals (CI). Data were assessed for variance and distribution, and comparisons between groups were performed using Fisher’s Exact test and independent sample t-tests with pooled or separate variance, as appropriate. Receiver Operating Characteristics (ROC) curves were constructed to assess the performance of ETCO2 and traditional vital signs for predicting DKA. The correlation between levels of ETCO2, HCO3, and anion gap were conducted using Pearson’s correlation. Significance was set at 0.05. Data were analyzed using STATA (StataCorp; College Station, Texas USA).
Results
A total of 119 patients met the inclusion criteria, and one case was excluded due to missing hospital data. Among the included 118 patients, six (5%) were diagnosed with DKA. Fifty-six percent of the patients were male. Across the entire cohort, 91% were admitted to the hospital including 31% to the ICU, and there was 11% mortality. The mean overall ETCO2 was 34mmHg (95% CI, 32-37mmHg), mean BGL was 325mmol/L (95% CI, 294-356mmol/L), and mean HCO3 was 23.3mEq/L (95% CI, 22.3-24.3mEq/L). Patients diagnosed with DKA were more likely to be admitted to the ICU (100% versus 28%; P <.001), but there was no significant difference in mortality (17% versus 11%; P = .512; Table 1).
Table 1. Comparison of Characteristics of Patients without a Diagnosis of DKA versus those with a Diagnosis of DKA
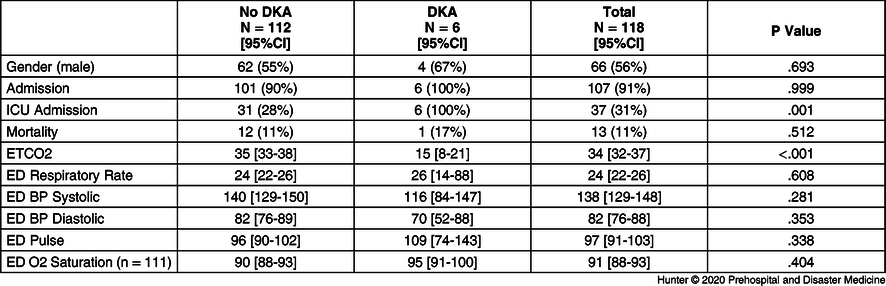
Abbreviations: BP, blood pressure; DKA, diabetic ketoacidosis; ED, emergency department; ETCO2, end-tidal carbon dioxide; ICU, intensive care unit; O2, oxygen.
The mean level of prehospital ETCO2 was significantly lower in patients diagnosed with DKA (15mmHg; 95% CI, 8-21mmHg) compared to those that were not (35mmHg; 95% CI, 33-38mmHg; P <.001; Table 1). There were no other significant differences in vital signs between the two groups (Table 1). The Area Under the ROC Curve (AUC) for ETCO2 identifying DKA was 0.96 (95% CI, 0.92-1.00; P <.001; Figure 1). The AUC of other prehospital vital signs to identify DKA yielded the following AUCs: SBP 0.71 (95% CI, 0.52-0.90); DBP 0.71 (95% CI, 0.55-0.87); SPO2 0.42 (95% CI, 0.24-0.60); respiratory rate 0.54 (95% CI, 0.27-0.80); and pulse rate 0.60 (95% CI, 0.37-0.82; P >.05 for each). In-patient laboratory testing showed the AUC for HCO3 identifying DKA was 0.96 (95% CI, 0.91-1.00). The AUC for anion gap identifying DKA was 0.92 (95% CI, 0.79-1.00). The correlation coefficient between ETCO2 and HCO3 was 0.436 (P <.001; Figure 2) and the correlation coefficient between ETCO2 and anion gap was -0.397 (P <.001).

Figure 1. The Area Under the ROC Curve (AUC) for ETCO2 and Identifying DKA (0.96; 0.92-1.00; P <.001).

Figure 2. The Correlation Between ETCO2 and HCO3 was 0.436 (P <.001).
Discussion
The current study suggests that low ETCO2 levels are indicative of DKA in prehospital patients with hyperglycemia. Among patients diagnosed with DKA, ETCO2 levels were significantly lower, and all of the patients diagnosed with DKA had ETCO2 levels less than 25mmHg. Prehospital ETCO2 correlated with in-hospital HCO3 levels, effectively predicting anion gap acidosis. This information may help guide transport destination, the need for prehospital interventions such as fluid resuscitation, and allow for pre-arrival notification of critically ill patients to the hospital.
Several prior reports have shown that ETCO2 correlates with HCO3 and predicts DKA in diabetic patients presenting to the ED.Reference Soleimanpour, Taghiadieh, Niafar, Rahmani, Golzari and Esfanjani6-Reference Hunter, Silvestri, Ralls, Bright and Papa9 Further studies have suggested continuous capnography is a reasonable strategy for monitoring acidosis in this population during resuscitation.Reference Agus, Alexander and Mantrell10,Reference Garcia, Abramo, Okada, Guzman, Reisch and Wiebe11 This study adds to that literature, suggesting ETCO2 may be an important triage tool in the setting of undifferentiated prehospital hyperglycemia. A further application may be to screen all out-of-hospital patients with known diabetes. Use of this information may help guide the need for Advanced Life Support intervention in two-tiered EMS systems, or for expedited critical care upon hospital arrival.
End-tidal carbon dioxide has been shown to predict lactic acidosis and mortality in sepsis,Reference Hunter, Silvestri, Ralls, Stone, Walker and Papa12,Reference Hunter, Silvestri, Dean, Falk and Papa13 trauma,Reference Childress, Arnold, Hunter, Ralls, Papa and Silvestri14 and shock.Reference Kheng and Rahman15 A correlation between exhaled ETCO2 and HCO3 has been reported in the setting of dehydrationReference Yang, Jeon, Min and Lee16 and DKA.Reference Soleimanpour, Taghiadieh, Niafar, Rahmani, Golzari and Esfanjani6-Reference Hunter, Silvestri, Ralls, Bright and Papa9 This correlation was also found in an undifferentiated prehospital population.Reference Hunter, Silvestri, Ralls, Bright and Papa9 End-tidal carbon dioxide is a mechanism of ventilation, perfusion, and metabolism. Extremely low levels are seen during severely acidotic and poorly perfused states. While it is possible that the lower levels reported in DKA are due to poor perfusion, there was no significant difference in blood pressure in the current study. The mechanism for low ETCO2 in DKA is likely secondary to the carbonic anhydrase buffering system being overwhelmed. Once HCO3 has been exhausted to lower levels, less carbon dioxide can be produced and exhaled. Thus, the predictive value of ETCO2 is likely due to functionality as a surrogate marker for metabolic acidosis.
Studies have shown high EMS utilization rates for diabetes-related illnesses and hyperglycemia,Reference Villani, Nanayakkara and Ranasinha3-Reference Benoit, Kahn and Geller5 suggesting an opportunity for clinical intervention. In fact, a comprehensive protocolized approach to prehospital diabetes care has been suggested to improve outcomes.Reference Villani, Nanayakkara and Ranasinha3 The ability to better differentiate between hyperglycemia and DKA could vastly change the approach to care in this arena. Caring for patients in DKA is complicated and nuanced, however intravenous fluid rehydration and insulin infusion are the mainstays of treatment. Fluid administration is common among many EMS systems, and the potential for insulin treatment exists for many others. Importantly, prehospital identification of DKA may also improve in-hospital care via pre-arrival notification.
Limitations
Limitations included the retrospective, observational nature of the study which may introduce selection bias, and relatively small sample size. Larger studies will be necessary to determine reliable cut-off points of ETCO2 levels for ruling out DKA in hyperglycemic patients. The study was performed at a single site using a single set of protocols and may not be generalizable to a broader population. However, the results are similar to prior in-hospital reports.
Conclusion
The current study suggests that low ETCO2 levels may predict DKA in prehospital patients with hyperglycemia. Given the critical nature of this disorder and the frequency with which EMS crews transport hyperglycemic patients, early identification of DKA may help guide transport destination and prehospital interventions.
Acknowledgements
This study is published in memory of Dr. Sal Silvestri.
Conflicts of interest
none





