Introduction
Cases of facial nerve palsy due to parotid gland pathology are usually associated with malignancy. In contrast, facial nerve palsy due to parotid gland abscess is very rare, with only eight previously reported cases.Reference Marioni, Rinaldi, de Filippis, Gaio and Staffieri1, Reference Noorizan, Chew, Khir and Brito-Mutunayagam2
Within one and a half months, two cases of facial nerve palsy secondary to parotid gland abscess were referred to the ENT department of Gentofte University Hospital, Copenhagen, Denmark. This hospital has a catchment area of approximately 900 000 patients. These two cases are described here.
Case one
A 22-year-old Filipino woman, who had recently returned from the Philippines, was referred by her general practitioner on suspicion of acute suppurative parotitis. The general practitioner had prescribed oral penicillin and dicloxacillin, with no apparent effect.
On physical examination, the patient had swollen, warm skin over the left parotid gland and was in slight pain. There was no fluctuation and no excretion of pus from Stenson's duct. Blood test results indicated neutrophilia (with a neutrophil count of 17.6 × 109/l) and a highly elevated C-reactive protein level (292 mg/l).
As the patient's general condition was good, she was discharged on continuing oral antibiotics.
However, after three days the patient was rehospitalised due to the onset of trismus and left facial nerve palsy of House–Brackmann grade IV. Antibiotic treatment was changed to intravenous benzylpenicillin, dicloxacillin and metronidazole.
A computed tomography (CT) scan showed a large abscess in the deep lobe of the parotid, and several smaller abscesses in the superficial lobe (Figure 1).
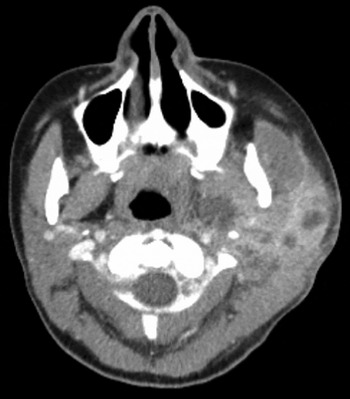
Fig. 1 Axial computed tomography scan for case one, showing abscess formation in the deep and superficial lobes of the left parotid gland.
Acute tonsillectomy was performed, and large quantities of foul-smelling pus were drained from the deep lobe of the parotid gland. The superficial abscesses were drained by ultrasound-guided puncture.
Despite this procedure, two days after surgery the patient's clinical condition had not improved.
Therefore, a second CT scan of the neck and thorax was performed. This showed recurrent, multiloculated abscess formation in the parotid gland, together with obstruction of the internal jugular vein and new infiltrates in the lungs, leading to suspicion of tuberculosis.
Ultrasound-guided drainage of the multi-loculated abscess was performed. The abscess pus was investigated for mycobacteria, via microbial culture, light microscopy and polymerase chain reaction.
The patient was transferred to the lung diseases department for anti-tuberculous therapy, despite a negative Quantiferon test (assessing interferon-γ quantity; QuantiFERON-TB Gold, Cellestis Inc., Valencia, CA 91355, USA).
Five days after surgery, methicillin-resistant Staphylococcus aureus was detected in the culture of the intra-operative specimen. Thus, oral clindamycin was prescribed for four weeks. There was no sign of mycobacteria in the culture.
The patient improved, and was discharged on day eight of admission.
One month after discharge, the patient's facial nerve palsy persisted, but there was no swelling of the neck or cheek, and no signs of infection on blood testing.
Case two
A 46-year-old Caucasian woman with a four-day history of right-sided cheek pain was referred to the ENT department on suspicion of acute suppurative parotitis. Prior to referral, she had been prescribed oral penicillin.
Ultrasound examination demonstrated no pathology in the parotid gland.
The patient was discharged and referred for Dental evaluation due to a suspected dental focus; this was disproved.
However, later that same day the patient was readmitted because of the acute onset of trismus and facial nerve palsy, with the influence of ramus marginalis. Blood test results showed neutrophilia (9.8 × 109/l) and a slightly elevated C-reactive protein level (48 mg/l). The physical examination showed no signs of abscess. A CT scan showed an abscess in the deep lobe of the right parotid gland, with communication to the parapharyngeal space.
Intravenous ceftriaxone and metronidazole were prescribed. Acute tonsillectomy was performed, including deep lobe incision of the parotid gland, which revealed a cystic, pus-filled cavity.
In the days following surgery, drainage was optimised via dilatation and flushing of the abscess cavity. The patient's facial nerve palsy diminished, and was absent at discharge, five days after surgery.
Microbial cultivation subsequently showed growth of Propionibacterium acnes. Peri-operative biopsies of the parotid gland and parapharynx showed no signs of malignancy.
Discussion
Facial nerve palsy secondary to parotid gland abscess is a rare condition, but is probably under-reported.
Parotid gland abscesses can develop following ascending infection up the parotid duct (Stenson's duct), secondary to bacteraemia, or via peri- and intraparotideal embedded lymph nodes. The infective agent is usually S aureus, Streptococcus pyogenes, Mycobacterium tuberculosis, anaerobic bacteria or pseudomonal species.Reference Tan and Goh3, Reference Smith and Hartig4
Propionibacterium acnes is part of the normal skin and oral flora. This bacterium is capable of infecting glands of the head and neck, and can produce abscesses.Reference Park, Na, Park, Moon, Cho and Park5, Reference Brook and Frazier6Propionibacterium acnes is thought to be a pathogen in acne vulgaris, endocarditis, arthritis, osteomyelitis, sepsis, endophthalmitis and lymphadenitis. To our best knowledge, P acnes has not previously been isolated from a parotid abscess. However, it is unclear whether this bacterium was the causative organism responsible for abscess formation, or a contaminant.
Our report also represents the first description of methicillin-resistant S aureus causing parotid gland abscess formation with facial nerve palsy as a complication.
Investigation of suspected parotid gland abscess should include assessment of infection parameters, ultrasonography of the gland, and CT scanning if complications are detected (e.g. facial nerve palsy).
• Parotid gland abscess is a rare cause of facial nerve palsy
• The abscess is treated with intravenous antibiotics
• Surgical treatment is required only if complications occur
• Both methicillin-resistant Staphylococcus aureus and Propionibacterium acnes can be involved
• Pre-operative ultrasonography and computed tomography are useful to assess the abscess location and size
Upon detection of an abscess, hospitalisation is recommended to facilitate intravenous treatment with broad-spectrum antibiotics that cover Gram-positive, Gram-negative and anaerobic bacteria.Reference Smith and Hartig4 In Denmark, cefuroxime is the first antibiotic of choice. Surgery is indicated if the facial nerve is affected, if the clinical condition does not improve despite antibiotic treatment for three to five days, or if the deep neck spaces are involved.Reference Smith and Hartig4 Computed tomography is useful for pre-operative evaluation.
According to the existing literature, facial nerve palsy due to parotid gland abscess has a good prognosis: eight of the 10 reported patients, including our two cases, had complete resolution.Reference Marioni, Rinaldi, de Filippis, Gaio and Staffieri1



