Introduction
The Eustachian tube has at least three physiological functions with respect to the middle ear: to protect it from secretions from the nasopharynx, to drain secretions produced within the middle ear into the nasopharynx, and to ventilate the middle ear to equalise it with atmospheric pressure.Reference Bluestone and Doyle1 The Eustachian tube is usually closed in the resting position, and dilates to the open position temporarily during swallowing, yawning, and other voluntary or involuntary actions.Reference Poe2 Tubal opening typically lasts for less than a half-second.Reference Mondain, Vidal, Bouhanna and Uziel3 Closure of the tube is maintained by a valve-like function of the opposing mucosal surfaces, submucosal tissue, fat, muscle and cartilage.Reference Poe2 The tubal valve measures approximately 5 mm in length, and lies within the cartilaginous portion of the Eustachian tube located about 10 mm into the tube distal from the nasopharyngeal orifice's posterior cushion or torus tubarius.Reference Poe, Metson and Kujawski4
A patulous Eustachian tube is defined as an abnormal opening of the Eustachian tube valve at rest, and results in symptoms of autophony, aural fullness and the hearing of self-generated breathing.Reference Grimmer and Poe5 The symptoms experienced by patients with a patulous Eustachian tube can vary in severity, ranging from being asymptomatic to having a severe disturbance in quality of life.Reference O'Connor and Shea6 However, patulous Eustachian tube is rare and in up to one-third of patulous Eustachian tube patients, no significant cause can be found.Reference Poe2 Various approaches for conservative medical management or surgical treatment may be considered for patients with a patulous Eustachian tube. No consensus regarding the treatment of choice has been reached because no option is clearly superior.
There are many possible risk factors associated with a patulous Eustachian tube, such as a loss of tissue within the cartilaginous portion of the Eustachian tube, acute weight loss, pregnancy, use of high-dose oral contraceptives, oestrogen therapy for prostate cancer, nasopharyngeal atrophy after adenoidectomy, radiation therapy, multiple sclerosis, and other neuromuscular diseases.Reference Poe2,Reference Bluestone7–Reference Adil and Poe9 However, in the majority of cases, no underlying precipitating event is evident. Principally, patulous Eustachian tube is thought to be caused by a concave defect in the tubal valve's anterolateral wall.Reference Poe2,Reference Takahashi, Honjo and Fujita10 However, not all patients diagnosed with a patulous Eustachian tube have such a defect (Figure 1b). Although the presence of a defect in the anterolateral wall of the tubal valve is considered clinically important in patulous Eustachian tube patients, it has seldom been described in the literature.
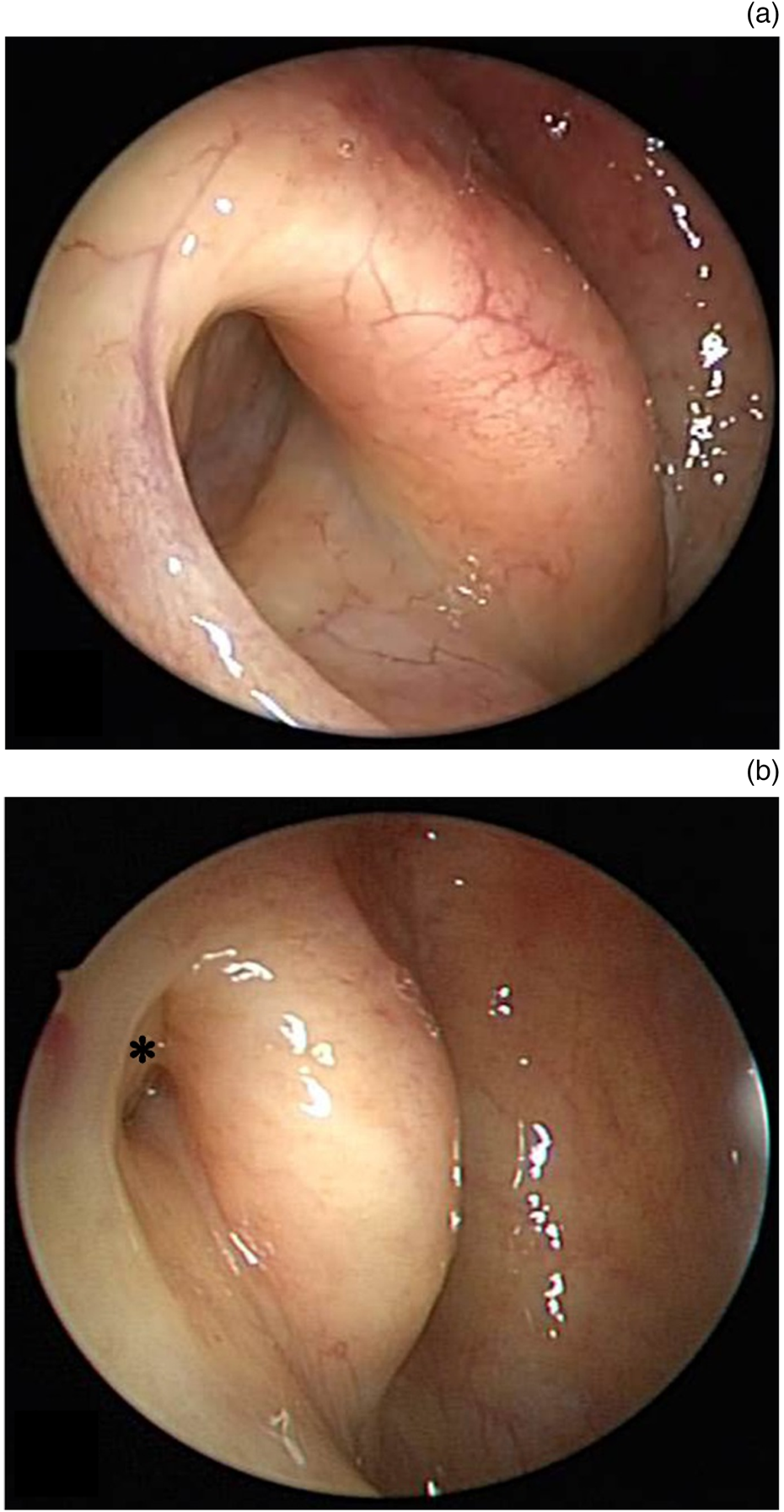
Fig. 1. Endoscopic views showing (a) the presence or (b) absence (asterisk) of a concave defect in the anterolateral wall of the right Eustachian tube orifice.
Therefore, in this study, we compared the clinical features of patulous Eustachian tube patients with or without a defect in the anterolateral wall of the tubal valve, to investigate how clinical symptoms and treatment methods differ according to the presence or absence of the defect.
Materials and methods
This study was based at a single tertiary academic referral centre. Sixty-six patients diagnosed with a patulous Eustachian tube who attended the otology out-patient clinic between March 2015 and February 2016 were enrolled in this study. The results were reviewed and analysed retrospectively. Medical records were reviewed with a minimum follow-up period of six months. The study was performed in accordance with the Helsinki Declaration and was approved by the Institutional Review Board (number: H-1901-004-074). In light of the retrospective study design, the need for written informed consent was waived by the review board.
In this study, we reviewed the data of a questionnaire used by our hospital for patients with Eustachian tube dysfunction. The questionnaire solicited the patients’ basic medical history, including age, sex, onset of symptoms, laterality of symptoms, presence of weight loss, height, body weight, medication history, type of symptoms, and symptom severity as judged by a visual analogue scale (VAS).
The questionnaire data were evaluated alongside specific endoscopic findings of the tympanic membrane, nasal cavity and Eustachian tube orifice obtained during physical examination performed by a single otologist (Figure 2). The anterolateral tubal valve of the nasopharyngeal end of the Eustachian tube was examined with a 30° nasal endoscope. Each ear diagnosed with a patulous Eustachian tube was categorised as positive or negative for a defect in the anterolateral wall of the tubal valve.
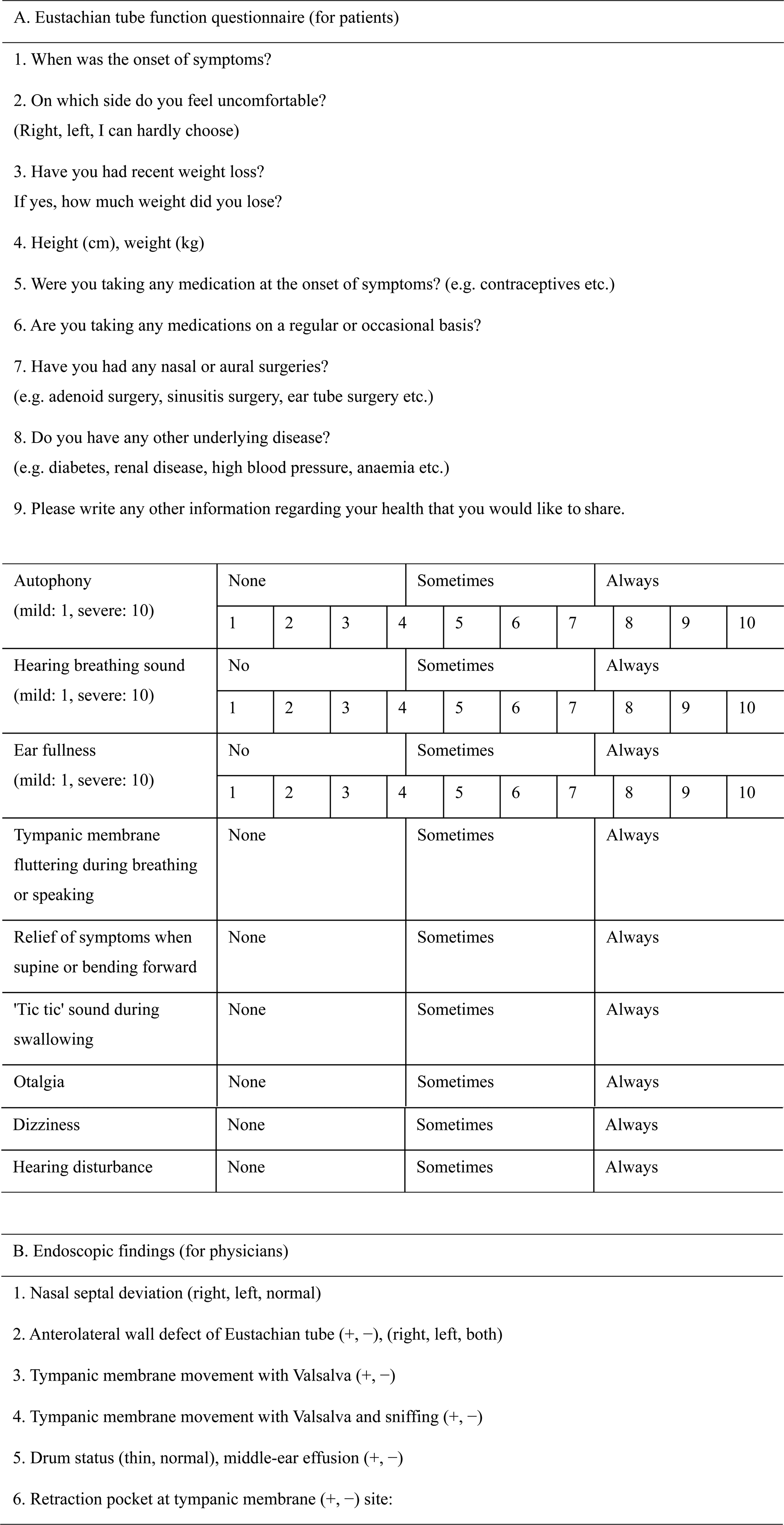
Fig. 2. Patulous Eustachian tube questionnaire.
In this study, a patulous Eustachian tube was diagnosed based on the presence of aural symptoms (autophony, hearing of self-generated breathing and ear fullness), and by visualisation of medial and lateral movement of the tympanic membrane coincident with forced breathing. If the typical tympanic membrane movement associated with a patulous Eustachian tube was not visualised, the patient was asked to perform the Valsalva manoeuvre followed by sniffing. Hearing of self-generated breathing was considered present if the sound was relieved by changes in posture, including lowering the head, lying supine and opening the mouth.
Conservative management, including providing reassurance and medical treatment, was administered to all patients with a patulous Eustachian tube initially. Patients were counselled regarding weight gain and the discontinuation of decongestants. Nasal saline irrigation with ipratropium bromide nasal spray (Rhinovent, Seoul, Korea), a topical anti-cholinergic, was used as medical treatment for two months. Patients refractory to conservative and medical management underwent transtympanic catheter insertion after two months.Reference Oh, Lee, Goh and Kong11,Reference Sato, Kawase, Yano, Suetake and Kobayashi12
SPSS software, version 25 (IBM, Armonk, New York, USA), was used for statistical analyses. For parametric variables, differences between patulous Eustachian tube patients with or without defects in the anterolateral wall of the tubal valve were evaluated using the independent two-sample t-test. Pearson's chi-square test was used for analysing the differences in the proportions of non-parametric variables. Statistical significance was defined as p < 0.05.
Results
Of the 132 ears analysed in 66 patients, 96 were diagnosed with a patulous Eustachian tube. The orifice of the Eustachian tube was observed by endoscopy through the nasal cavity. Each ear with a patulous Eustachian tube was categorised as positive or negative for a defect in the anterolateral wall of the tubal valve. Fifty-nine ears with a patulous Eustachian tube (61.5 per cent) were diagnosed with a defect in the anterolateral wall of the tubal valve and 37 were without such a defect (38.5 per cent). Of 36 normal ears not diagnosed with a patulous Eustachian tube, 5 ears were diagnosed with a defect in the anterolateral wall of the tubal valve and 31 were without this defect. Interestingly, all five ears with the defect were diagnosed with a similar defect on the opposite side.
Of the 66 patients, 30 patients (22 with a defect in the anterolateral wall of the tubal valve (73.3 per cent) and 8 without a defect (26.7 per cent)) were diagnosed with bilateral patulous Eustachian tube. The association between the presence of a defect in the anterolateral wall of the tubal valve and bilaterality was significant (chi-square (degrees of freedom = 1, n = 66) = 6.66, p = 0.013, odds ratio = 2.155, 95 per cent confidence interval (CI) = 1.129–4.116) (Table 1). In cases with the defect, patulous Eustachian tube was right-sided in 29 and left-sided in 30 cases. In cases without the defect, patulous Eustachian tube was right-sided in 23 and left-sided in 14 cases. There was no significant difference in laterality between the two groups (Table 1).
Table 1. Clinical features of patulous Eustachian tube patients

*P < 0.05. †Abnormal tympanic membrane status included retraction and middle-ear effusion. ‡Surgical treatment included transtympanic catheter insertion. ET = Eustachian tube; SD = standard deviation
Greater numbers of females than males were diagnosed with (35.6 per cent male, 64.4 per cent female) and without a defect in the anterolateral wall of the tubal valve (10.8 per cent male, 89.2 per cent female). However, the association between the presence of the defect and male sex was significant (chi-square (degrees of freedom = 1, n = 96) = 7.25, p = 0.007, odds ratio = 3.292, 95 per cent CI = 1.227–8.835).
There were no group differences in terms of tympanic membrane status or the presence of nasal septal deviation. For 45.8 per cent of patients with a defect in the anterolateral wall of the tubal valve and 24.3 per cent without such a defect, there was a history of weight loss in the previous six months. The association between the presence of the defect and recent weight loss was significant (chi-square (degrees of freedom = 1, n = 96) = 4.46, p = 0.035, odds ratio = 1.881, 95 per cent CI = 0.999–3.542). Interestingly, greater numbers of males than females were below the average body mass index (BMI) of the Korean general population, both in those with the defect (19 males (90.4 per cent) and 25 females (65.8 per cent)) and in those without the defect (3 males (75.0 per cent) and 23 females (69.7 per cent)). The Korean average BMI data for 2015 (24.1 kg/m2 for males, 22.6 kg/m2 for females) were obtained from the National Statistical Office. Additionally, the association between the presence of the defect and being refractory to conservative and medical management was significant (chi-square (degrees of freedom = 1, n = 96) = 4.34, p = 0.037, odds ratio = 1.960, 95 per cent CI = 0.991–3.875) (Table 1).
The accompanying symptoms were analysed, which included: autophony, the hearing of self-generated breathing, ear fullness, a sensation of tympanic membrane fluttering during breathing or speaking, relief of symptoms with postural change (i.e. supine or forward bending positions), hearing a ‘tic tic’ sound during swallowing, otalgia, dizziness, and hearing disturbances (Table 2). There was no significant difference in the incidence of accompanying symptoms between the two groups, except for the relief of symptoms when in a supine or forward bending position. The association between the presence of a defect in the anterolateral wall of the tubal valve and a relief of symptoms after these postural changes was significant (chi-square (degrees of freedom = 1, n = 96) = 4.03, p = 0.045, odds ratio = 2.449, 95 per cent CI = 1.011–5.932) (Table 2).
Table 2. Otological symptoms of patulous Eustachian tube patients

*P < 0.05. ET = Eustachian tube; VAS = visual analogue scale; SD = standard deviation
In addition, the presence of a defect in the anterolateral wall of the tubal valve of the Eustachian tube seemed to have a significant effect on the severity of symptoms. The severity of the three main symptoms of autophony, hearing of self-generated breathing and ear fullness was evaluated using a VAS. In the cases with the defect, the severity of autophony (mean (± standard deviation (SD)) score = 7.05 ± 2.04) and hearing of self-generated breathing (mean (± SD) score = 6.45 ± 3.24) was significantly greater than in those without such a defect (mean (± SD) scores = 5.28 ± 2.83 and 4.44 ± 2.86, respectively) (p < 0.05). However, there was no significant difference between cases with or without the defect in terms of the severity of ear fullness (mean (± SD) scores = 5.37 ± 3.01 and 5.38 ± 2.56, respectively) (Table 2 and Figure 3).
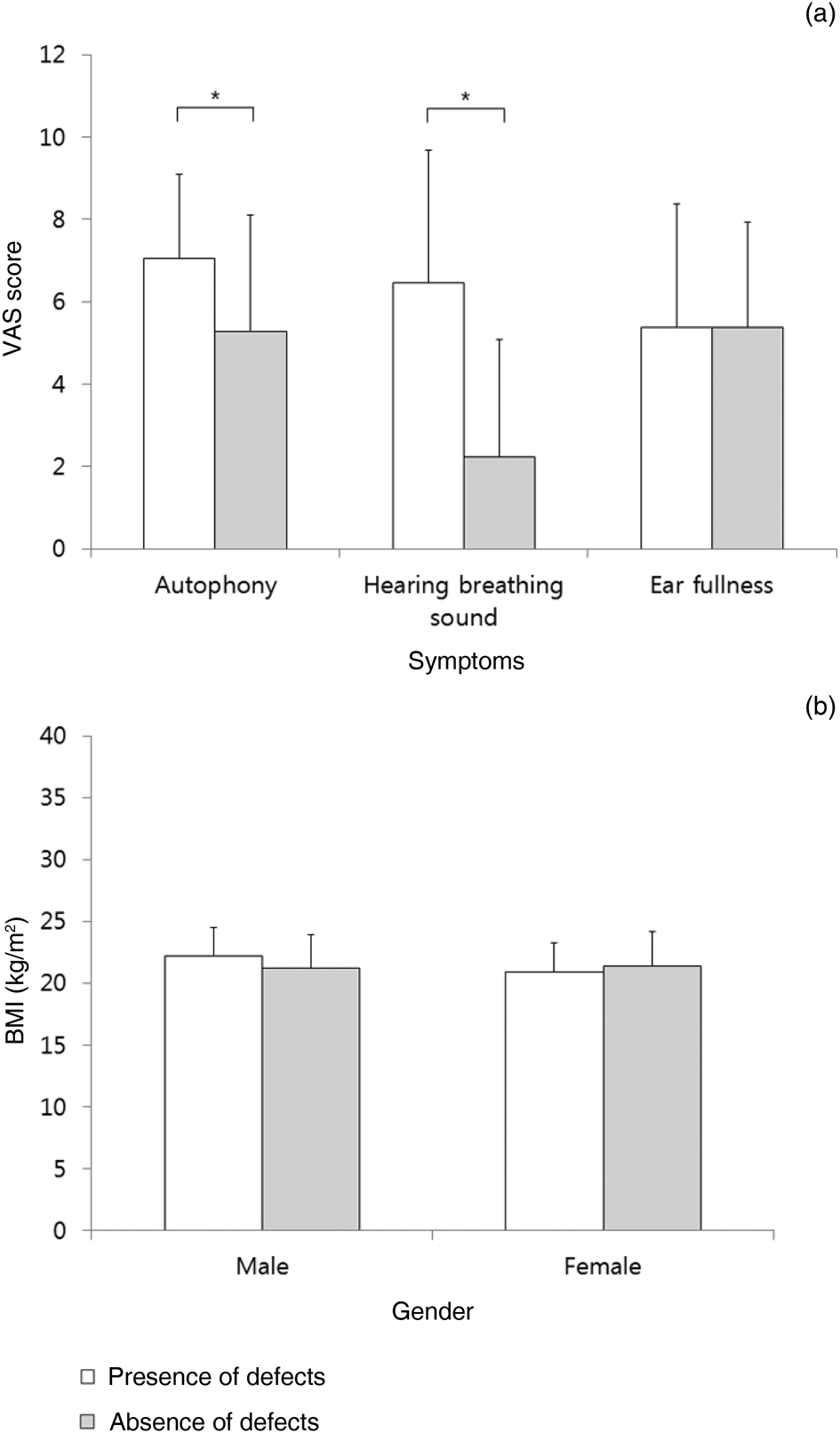
Fig. 3. Comparisons of: (a) Eustachian tube dysfunction symptom severity assessed by visual analogue scale (VAS) scores (*p < 0.05), and (b) body mass index (BMI) values in males and females with Eustachian tube dysfunction. ‘Defects’ refers to defects in anterolateral wall of tubal valve.
Sixteen patients with a patulous Eustachian tube had a history of using medications. Of the patients with a defect in the anterolateral wall of the tubal valve, nine had a history of using hormonal agents (five in the form of oestrogen and four in the form of oral contraceptives) and four patients had previously used aspirin. Only one patient without the defect had a positive medication history, in the form of oral contraceptives.
Discussion
Patulous Eustachian tube is caused by patulous dysfunction of the Eustachian tube (persistent opening or insufficient closure). Patulous dysfunction can result in various symptoms, with the three most common being voice autophony, breathing autophony and aural fullness.Reference Hussein, Adams and Turner13 Symptoms can generally be relieved by bending forward to place the head down or by lying supine for a period of time. Patulous Eustachian tube is treated differently from obstructive pathologies of the Eustachian tube, with a focus on augmentation or reconstructive procedures.Reference Poe2 Patulous dysfunctions of the Eustachian tube seem to be caused by a loss of tissue in the superior aspect of the anterolateral wall within the tubal valve.Reference Poe2 This lost tissue may be cartilage and/or soft tissue, but the exact mechanism of the loss is unclear. The anterolateral wall of the tubal valve is normally convex and bulges into the posteromedial wall to close the valve in the resting position. However, not all patients diagnosed with a patulous Eustachian tube have a concave defect in the anterolateral wall of the tubal valve.
In this study, only 61.5 per cent of patulous Eustachian tube patients had a defect in the anterolateral wall of the tubal valve. The present study aimed to evaluate the clinical features of these patulous Eustachian tube patients and compare them to those without the defect. We found that more females than males were diagnosed with a patulous Eustachian tube, both in those with and without the defect. These results are consistent with the findings of a previous study, in which the incidence and prevalence of patulous Eustachian tube in females was almost twice as high as that of males.Reference Choi, Kim, Lee, Oh, Lee and Goh14 However, it is interesting to note that we found a significant association between the presence of the tubal defect and male sex (p = 0.007). In addition, the association between the presence of the defect and patulous Eustachian tube bilaterality was significant (p = 0.013). To the best of our knowledge, these associations have not been previously reported. As patulous Eustachian tube is relatively rare, further prospective multicentre studies comparing the differences between males and females with the defect to those without this defect are necessary for conclusive evidence.
In this study, the association between a defect in the anterolateral wall of the tubal valve and weight loss within the previous six months was significant (p = 0.035). Most patulous Eustachian tube patients in our study had a BMI below the Korean general population average. Our results are consistent with a previous study which reported that patulous Eustachian tube may be caused by a number of possible factors, such as a loss of tissue within the cartilaginous portion of the Eustachian tube and acute weight loss.Reference Poe2 Although the only significant difference in terms of the incidence of symptoms in those with or without the tubal defect was the relief of symptoms with postural changes, the presence of the defect had a significant effect on the severity of autophony and the hearing of self-generated breathing (p < 0.05). In addition, we found a significant association between the presence of the defect and being refractory to conservative and medical management (p = 0.037). Together, these results indicate that acute weight loss might contribute to a defect in the anterolateral wall of the tubal valve of the Eustachian tube, and, with acute tissue loss, the symptoms of patulous Eustachian tube may increase in severity. This means that surgical treatment may be more important for patients with the defect than for those without such a defect.
Numerous medical and surgical approaches are currently used in the management of patulous Eustachian tube. Non-invasive management includes nasal saline irrigation and the use of topical anticholinergics, such as ipratropium bromide, which reduce Eustachian tube function by decreasing the amount and changing the composition of Eustachian tube secretions.Reference Tjernström, Andréasson, Groth, Ivarsson and Malm15,Reference DiBartolomeo and Henry16 For patients refractory to conservative and medical management, various surgical approaches may be considered, including Blu Tack® or cartilage plugging of the Eustachian tube, manipulation of the Eustachian tube musculature, and transtympanic catheter insertion.Reference Oh, Lee, Goh and Kong11,Reference Bartlett, Pennings, Ho, Kirkpatrick, van Wijhe and Bance17–Reference Rotenberg, Busato and Agrawal20 As patulous Eustachian tube patients with and without a defect in the anterolateral wall of the tubal valve share many similar clinical features, the authors suggest that for patients without the defect, it is reasonable to start with medical rather than surgical treatment, in light of the less severe symptoms associated with the absence of the defect compared to the presence of such a defect.
• Not all patients diagnosed with a patulous Eustachian tube have a concave defect in the anterolateral wall of the tubal valve
• Patulous Eustachian tube patients with and without a defect in the anterolateral wall of the tubal valve share similar clinical features
• Evaluating the presence of such a defect is important for decision-making regarding patulous Eustachian tube management
• There was a significant association between a defect in the anterolateral wall of the tubal valve and being refractory to conservative and medical management
• More patients without a defect in the anterolateral wall of the tubal valve can be treated non-surgically than those with the defect
There are a few limitations to this study. First, this research was based on a retrospective review of records from a single tertiary academic referral centre. Moreover, patients with relatively severe patulous Eustachian tube visit our hospital to seek treatment including transtympanic catheter insertion.Reference Oh, Lee, Goh and Kong11,Reference Sato, Kawase, Yano, Suetake and Kobayashi12 For these reasons, clinical characteristics could be distorted. Second, the relatively small sample size of our study might increase the possibility of bias. Given the low detection rate and high psychological distress caused by a patulous Eustachian tube, it is difficult to perform a prospective study on this condition at a single institution. These limitations suggest the need for a well-designed, prospective, case–control study. Furthermore, the mechanisms underlying these phenomena need to be studied in the future.
The present study investigated the clinical characteristics of patulous Eustachian tube patients with and without a defect in the anterolateral wall of the tubal valve. While the patients shared many clinical features, we suggest that it is important to determine the presence of the defect in order to assist in the appropriate management of the patulous Eustachian tube. Specifically, surgical treatment can be considered in patients with the defect and non-surgical treatment can be administered to those without the defect.
Competing interests
None declared







