There is growing evidence that children are at an increased risk of developing pressure injuries.Reference Kiss and Heiler 1 – Reference Visscher, King and Nie 3 The National Pressure Ulcer Advisory Panel, which serves as the expert voice in the United States of America regarding pressure injuries, recently updated the name from pressure ulcer to pressure injury, including adding an expanded definition of this phenomenon. 4 Pressure injury is defined as
localized damage to the skin and/or underlying soft tissue usually over a bony prominence or related to a medical or other device. The injury can present as intact skin or an open ulcer and may be painful. The injury occurs as a result of intense and/or prolonged pressure or pressure in combination with shear. The tolerance of soft tissue for pressure and shear may also be affected by micro-climate, nutrition, perfusion, co-morbidities, and condition of the soft tissue. 4
Pressure injury can lead to pain and suffering for patients and families, add additional morbidity, alter body image, increase the complexity of care, or potentially evolve into a life-threatening infection-related complication.Reference Allman, Goode, Burst, Bartolucci and Thomas 5 , Reference Reddy, Gill and Rochon 6 The incidence of pressure injuries in children in paediatric ICUs has been reported from 0.8 to 27%.Reference Schindler, Mikhailov and Kuhn 2 , Reference Curley, Razmus, Roberts and Wypij 7 In a nationwide study of multiple paediatric ICUs, the aggregate rate of pressure injury by volume was 24.35 per 1000 patient days, ranging from 2.47 to 57.10 by site.Reference Schindler, Mikhailov and Kuhn 2 However, little is known about pressure injury development in hospitalised infants and children with CHD, resulting in little evidence to guide practice.
Background
CHD is the number one birth defect in the United States of America, affecting nearly 40,000 births annually. 8 CHD is the leading cause of infant illness and death associated with birth defects. 8 Many children today with CHDs are living longer into adulthood owing to ongoing medical, surgical, nursing, and technological advancements. One study using 2010 United States of America census data estimated that approximately one million children and approximately 1.4 million adults are living in the United States of America with CHD.Reference Gilboa, Devine and Kucik 9 Many children with CHD require life-long medical or surgical follow-up, and some require frequent or prolonged hospitalisations for diagnostic or interventional procedures, cardiac surgery, or other therapeutic management.
The adult population with CHD who continue to be cared for in paediatric hospitals is growing.Reference Hickey, Gauvreau, Tong, Schiffer and Connor 10 Paediatric speciality procedure areas and inpatient units, including cardiac intensive care and cardiac inpatient units, are caring for an increasingly multi-age, complex cardiac population. In hospitalised adults, patients in ICUs, undergoing surgery, history of cardiac disease, spinal cord injury, or prolonged immobility, are at an increased risk of developing pressure injuries.Reference Black, Edsberg and Baharestani 11 – Reference Swafford, Culpepper and Dunn 14 Surgical patients have an increased risk of developing pressure injuries related to prolonged periods of immobility under anaesthesia and time in the operating room.Reference Aronovitch 15 Surgical procedures lasting more than four hours increase the risk of pressure-related tissue injury.Reference Schoonhoven, Defloor, van der Tweet, Buskens and Grypdonck 13 , Reference O’Connell 16
Adult patients requiring cardiac surgery present unique care challenges related to therapeutic interventions. During cardiac surgery, many patients undergo varying periods of cardiopulmonary bypass and hypothermia, which may affect tissue perfusion and oxygenation. Other common interventions in the operating room for cardiac surgical patients include general anaesthesia, administration of vasoactive medications, and the use of multiple medical devices for patient monitoring and therapeutic care that put the patient at risk for pressure injury development.Reference Rao, Preston, Strauss, Stamm and Zalman 17 For consistency, the new terminology of pressure injury will be utilised in this paper.
Little is known about paediatric cardiac surgical patients and the development of pressure injury. Paediatric cardiac surgical patients may be vulnerable to similar risk factors as adult cardiac surgical patients, including exposure to prolonged periods of immobility during complex surgical procedures.Reference Ahern and Hickey 18 , Reference Galvin and Curley 19 Prolonged periods of immobility may occur during other invasive diagnostic or interventional procedures such as cardiac catheterisation or in the ICU postoperatively.Reference Kiss and Heiler 1 In the cardiac ICU, some patients may need escalating medical interventions requiring advanced technology such as high-frequency oscillatory ventilation, extracorporeal membrane oxygenation, or ventricular assist devices, all limiting the patient’s mobility. Moreover, paediatric cardiac surgical patients are exposed to multiple medical devices that are attached to, or cross over, the skin and are required for their care.
With the growing focus on quality care, patient safety, and reporting quality care metrics to regulatory agencies, there is a need to understand the development of hospital-acquired pressure injury and prevention strategies across patient populations. The Centers for Medicare and Medicaid Services defined the development of Stage 3 and Stage 4 pressure injuries as adverse patient safety events or “never events” that are reasonably preventable by implementing evidence-based prevention guidelines. 20 Some states mandate acute care hospitals, including paediatric hospitals, to report never events to the State Department of Public Health within 7 days. 21 Prevention of pressure injuries may lead to improved patient outcomes and potentially reduce resource utilisation by these complex patients and families that have been shown to use a disproportionately high share of hospital resources.Reference Connor, Gauvreau and Jenkins 22 , Reference Hickey, Gauvreau, Jenkins, Fawcett and Hayman 23
The problem
In the summer of 2009, despite ongoing pressure injury prevention strategies in the paediatric cardiac ICU, there was a spike in serious peri-sacral pressure injuries in postoperative patients, particularly in preteen to teenage patients. As a quality improvement initiative, an interdisciplinary Cardiovascular Pressure Ulcer Workgroup was re-established to review and refocus pressure injury prevention efforts. Strategies that utilise a comprehensive preventative approach can reduce the prevalence and incidence of pressure injuries.Reference Swafford, Culpepper and Dunn 14 , Reference Schindler, Mikhailov, Cashin, Malin, Christensen and Winters 24
Moreover, ongoing quality metric pressure injury surveillance data for the cardiac ICU in 2010 revealed 46 pressure injuries for cardiac surgical patients, with 70% (32/46) being medical-device-related and 30% (14/46) related to immobility. The overall pressure injury rate was 6.0/1000 patient days. The immobility-related rate was 1.8/1000 patient days, and the rate related to medical devices was 4.2/1000 patient days. Pressure injuries were staged using the National Pressure Ulcer Advisory Panel Staging Guidelines at the time. 25 When identified, pressure injuries were Stage 1 (26%), Stage 2 (30%), mucosal membrane injury (15%) related to medical devices, suspected deep tissue injury (15%), and unstageable (11%).
Relevant literature
Most pressure injury prevention interventions in paediatrics have been extrapolated from adult studies.Reference Baharestani and Ratliff 26 There is little available evidence about the development of pressure injury in children with CHD. Patients with CHD have been specifically excluded from study, as there was uncertainty about the effects of chronic hypoxaemia on the development of pressure injury.Reference Curley, Razmus, Roberts and Wypij 7 The impact of chronic hypoxaemia on the development of pressure injury in patients with CHD remains unclear today. Limited available evidence suggests that the incidence of pressure injury in children with CHD ranges from 16.9 to 25%.Reference Kiss and Heiler 1 , Reference Neidig, Kleiber and Oppliger 27
An innovative approach
In response to the challenges of caring for patients with CHD, an innovative strategy for examining relevant clinical data to improve patient outcomes and reduce unnecessary resource utilisation within an improvement science framework was developed. Standard Clinical Assessment and Management Plans (SCAMPs™) are a novel quality improvement initiative conceived in the Cardiovascular Program, now known as the Heart Center, by the paediatric cardiologists and colleagues at a free-standing paediatric hospital in the northeast.Reference Rathod, Farias and Friedman 28 For the purposes of this manuscript, we will be referring to these types of assessment and management plans as SCAMPs™. The initial SCAMPs™ were physician-driven and outpatient focused.
Impressed by the initial outcomes of the cardiology SCAMPs™ and the concern regarding the lack of evidence about pressure injury development in patients with CHD, the cardiovascular nurses applied the SCAMP™ methodology. Our goal was to gain a better understanding of the development of pressure injury in hospitalised infants and children with CHD and examine prevention strategies. Although all of the previous SCAMPs™ had been “treatment” focused, the pressure ulcer prevention SCAMP™ was the first with a “prevention” focus. The pressure ulcer prevention SCAMP™ is a standard pressure injury prevention plan to reduce practice variability among nurses initiated on patient admission. Owing to the lack of evidence in the literature and the Braden Q paediatric pressure ulcer risk assessment tool not validated in the paediatric cardiac population when this quality improvement initiative was undertaken, a preventative pressure injury approach was initiated upon patient entry to the Heart Center. The pressure ulcer prevention SCAMP™ was developed specifically for the prevention of pressure injury in postoperative cardiac surgical patients across the programme from the preoperative cardiology clinic through the inpatient cardiac units.
Strategy of the SCAMP™
The strategy of the pressure ulcer prevention SCAMP™ was to use existing knowledge about pressure injury development and prevention strategies to create a standard prevention plan to reduce practice variation across the Heart Center. According to Rathod et al’s process,Reference Rathod, Farias and Friedman 28 patients are assessed and managed in a standardised way using an algorithm to reflect sound practice. The SCAMP™ allows the clinical variability of the patient population to evolve, allowing for diversions from the standard plan to occur. These diversions are recorded to learn through analysis how the care of some patients may need to be modified in a safe and effective way.Reference Rathod, Farias and Friedman 28 Using the SCAMP™ approach, there was an opportunity to gain a better understanding of the decision-making process of the bedside nurse in providing pressure injury prevention care.
The SCAMP™ is re-evaluated at a predetermined point – for example, in 6–12 months – and may be changed based on a combination of best clinical judgement, evidence-based knowledge, and analysis of new data.Reference Rathod, Farias and Friedman 28 The SCAMP™ methodology offered an opportunity to better understand pressure injury development in paediatric cardiac surgical patients and to help build the foundational evidence for this vulnerable population.
Objective
The objective of this quality improvement project was to develop a standardized clinical assessment and management plan to describe the development of pressure injury in paediatric cardiac surgical patients and evaluate prevention strategies.
Materials and methods
SCAMP™ development
The pressure ulcer prevention SCAMP™ quality improvement effort was considered exempt by the organisation’s Institutional Review Board. In October 2010, an expert panel of 13 nurses was convened, including clinical nurse leaders, expert staff, and nurse scientists from across the Heart Center, to develop this important programme-wide collaborative initiative. This effort also received support from SCAMP™ managers, administrative staff, and biostatisticians. Using a consensus model, the expert panel developed key components of this first nursing SCAMP™ including a background paperReference Ahern and Hickey 18 to establish the state of the evidence about the paediatric cardiac population and the identification of 12 targeted data statements. Other forms developed as part of the process included an enrolment form to identify inclusion and exclusion criteria, the pressure ulcer prevention SCAMP™ algorithm (©2010 Boston Children’s Hospital. All rights reserved), and the data collection form.
Targeted data statements, which were initially called plausible outcomes, are similar to hypotheses, which are explored by the SCAMP™ but do not require the same level of study in development as needed for a randomised clinical trial.Reference Rathod, Farias and Friedman 28 The targeted data statements, as described in Table 1, are a critical step in the development process as they help identify specific clinical statements to support evaluation of the SCAMP™.Reference Rathod, Farias and Friedman 28
Table 1 Targeted data statements.
PUP=pressure ulcer prevention; SCAMP™=Standard Clinical Assessment and Management Plans
The initial component of the SCAMP™ algorithm© used in the cardiac ICU and cardiac inpatient unit was the Standardized Pressure Ulcer Prevention Plan, as described in Table 2. This prevention plan was built on the limited evidence available and our previous prevention experience in the Heart Center including the Cardiovascular Program Pressure Injury Prevention Guidelines already in place.Reference Ahern and Hickey 18 , Reference Curley and Hickey 29 Pressure injury prevention interventions have been reported by organisations for adults. 25 , 30 , 31 The Institute of Healthcare Improvement 32 published a How-to-Guide supplement for paediatrics, including six essential elements for pressure injury prevention: on admission, perform both a skin and risk assessment; re-assess patient risk; daily skin assessment; manage moisture; optimise nutrition and hydration; and minimise pressure through repositioning and use of pressure re-distribution surfaces. Moreover, through our monthly review of our patient safety reports, we had seen a trend of pressure injury related to medical devices, so prevention strategies were included in the pressure ulcer prevention SCAMP™ to address specific medical devices. These interventions were bundled together and became the Standard Pressure Injury Prevention Plan covering both immobility and medical-device-related pressure injuries.
Table 2 Cardiac ICU Standard Pressure Injury Prevention Plan.

Includes recommendations used and modified with permission from Ahern and HickeyReference Ahern and Hickey 18 and Institute for Healthcare Improvement 32
SCAMP™ process
The pressure ulcer prevention SCAMP™ process started in the preoperative clinic to identify whether the patient had a previous history or existing pressure injury. A pre-procedure skin assessment was to be performed in the cardiac catheterisation lab or operating room to identify evidence of current skin injury. Perioperative pressure injury risk and intervention tools were developed and implemented in the cardiac operating room.Reference Galvin and Curley 19 A post-procedure skin reassessment was completed, and, if an area of skin concern was identified, this information was included during the handoff when the patient arrived to the inpatient units.
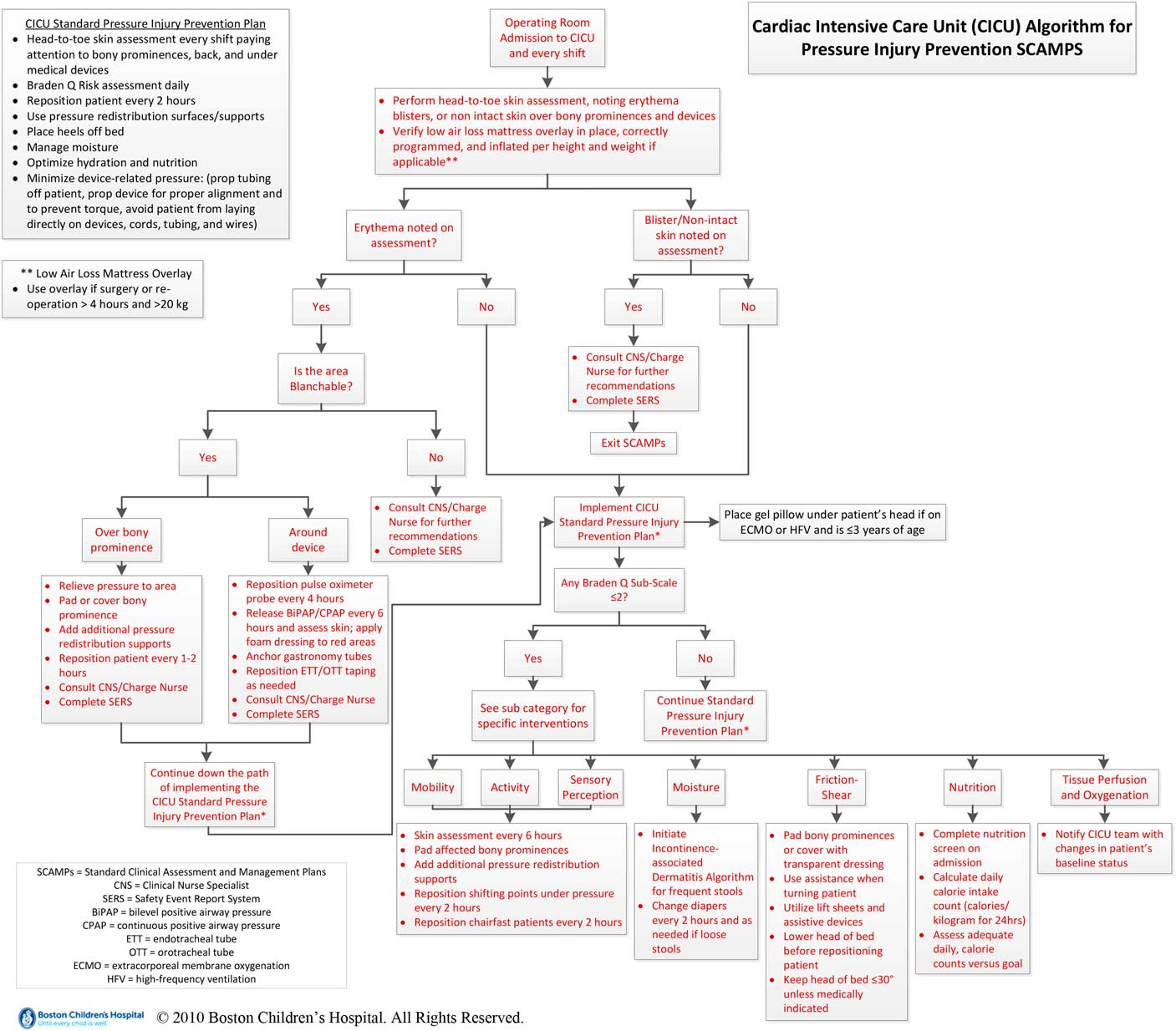
The inpatient pressure ulcer prevention SCAMP™ algorithm© (see Fig 1) started with a head-to-toe skin assessment upon admission from the cardiac operating room to the cardiac ICU, and further skin assessments were performed and documented every shift by nurses. On the basis of these skin assessment findings, additional targeted interventions were recommended by the pressure ulcer prevention SCAMP™ in addition to the Standard Pressure Injury Prevention Plan. Skin assessments included looking at the patient’s skin for physical signs such as the presence of erythema or evidence of non-intact skin or blister, over a bony prominence or around a medical device.

Figure 1 Inpatient pressure ulcer prevention SCAMP™ Algorithm©. A decision tree depicts the clinical management algorithm for patients admitted to the cardiac ICU based on clinical symptoms such as erythema, blistering, and non-intact skin. Separate boxes to the left of the decision tree summarise the key elements of the pressure ulcer prevention plan and appropriate mattress use.
As part of the pressure ulcer prevention SCAMP™, the patient’s risk for pressure injury development was assessed using the Braden Q Pressure Ulcer Risk Assessment ScaleReference Curley, Razmus, Roberts and Wypij 7 (see Fig 2) on admission and then daily. The Braden Q total score ranges from 7 to 28, with a score⩽16 identifying children “at risk” of developing pressure injuries. The SCAMP™ went beyond looking at the total score and included the strategy of looking at the seven subscales scored as 1 or 2 (higher risk) to respond to individual patient risk by implementing additional select interventions. If the individual subscale scores were assessed at higher risk, targeted additional interventions were recommended according to the pressure ulcer prevention SCAMP™ algorithm© for each subscale in addition to the Standard Pressure Injury Prevention Plan.

Figure 2 Braden Q Scale. The Braden Q Scale is a paediatric risk assessment tool used to predict pressure injury in children. Each subscale is scored from 1 to 4, with a score of 1 (highest risk) to a score of 4 (lowest risk). The seven subscales are totalled with possible score ranges of 7–28. Patients with scores⩽16 are considered to be at risk of developing pressure injury.
Inclusion and exclusion criteria
Inclusion criteria for this quality improvement process were patients undergoing congenital cardiac surgery or cardiac transplantation, ages of 37 weeks up to 21 years old, and without pre-existing evidence of a pressure injury on preoperative assessment screening. Postoperative care must be provided in the cardiac ICU or the cardiac inpatient unit with an expected stay greater than 23 hours. Exclusion criteria included non-congenital cardiac surgery patients, cardiac medical patients, infants less than 37 weeks gestation, adults greater than 21 years old, and patients with a pre-existing pressure injury. Postoperative patients who met the inclusion criteria received the Standard Pressure Injury Prevention Plan with further preventative care assessed and managed according to the pressure ulcer prevention SCAMP™ algorithm©.
Data collection
Data collection was initiated postoperatively on admission from the operating room by either the cardiac ICU or cardiac inpatient unit nurses. As the majority of cardiac surgical patients are directly admitted to the cardiac ICU, the majority of the data forms were initiated in the cardiac ICU. The data collection process was continued by the cardiac inpatient unit nurses when the patient transferred out of the cardiac ICU. Nurses self-reported data on admission and then daily on assessments and their decisions regarding the pressure ulcer prevention SCAMP™. As the recommended assessments and interventions was an all or none process to be considered on the pressure ulcer prevention SCAMP™, diversions from the pressure ulcer prevention SCAMP™ were expected. Diversions were recorded on the data form so that we could learn about care variability and nursing staff decision-making. The form included a short list of possible reasons for diversions, which included the following: patient/parent refusal, not medically able per doctors’ orders, too busy during shift, objection to SCAMP™ recommendations, and other. The other option provided a space where nurses could write in their reasons. Patients continued on the pressure ulcer prevention SCAMP™ until hospital discharge, the patient was transferred out of the Heart Center, or a pressure injury developed.
Clinical Nurse Specialists with additional pressure injury education, including a Certified Wound Ostomy nurse or Certified Wound Ostomy Continence nurse in both the cardiac ICU and the cardiac inpatient unit, followed the National Pressure Ulcer Advisory Panel and European Pressure Ulcer Advisory Panel Clinical Practice Guideline 25 for staging if a pressure injury was identified. The pressure injury stages available at the time of this initiative included Stage 1 through Stage 4, unstageable, or suspected deep tissue injury. Pressure injuries found on mucous membranes related to medical devices were staged as mucosal pressure injury as per the National Pressure Ulcer Advisory Panel position statement. 33 Staff nurses were asked to notify the unit Clinical Nurse Specialists or certified wound nurses if they noted an area of erythema, blister, or concern of skin injury over a bony prominence or under a medical device to confirm whether a pressure injury developed. The unit-level wound experts staged the pressure injuries according to the staging guideline, using a consensus-based approach if there was any disagreement regarding staging.
The development and pilot of the cardiovascular nursing pressure ulcer prevention SCAMP™ occurred from October, 2010 to June, 2011. The pressure ulcer prevention SCAMP™ was rolled out across the Heart Center on 1 July, 2011, as described in Figure 3. Nursing education about the pressure ulcer prevention SCAMP™ was provided to nursing staff across the Heart Center before the rollout. After 6 months of implementation of the pressure ulcer prevention SCAMP™, an interim analysis informed several modifications of the algorithm©. These changes included changing the frequency of position changes to every 2 hours and padding of “affected” bony prominences. The revised pressure ulcer prevention SCAMP™ began on 21 February, 2012. Data collection for analysis ended on 30 June, 2012.

Figure 3 Timeline of pressure ulcer prevention Standard Clinical Assessment and Management Plans (PUP SCAMP™) development, rollout, and data collection. Blue blocks arranged chronologically from left to right denote the different phases and time frame for PUP SCAMP™ development, rollout, and data collection. Development started in October, 2010 and data collection ended in June, 2012.
Statistical methods
Descriptive statistics were used to summarise demographic and clinical characteristics, hospital encounters, and pressure injuries. In the case of non-normally distributed continuous data, median (minimum, maximum) was reported. The rates of pressure injury and corresponding 95% confidence intervals were estimated assuming a Poisson distribution. The associations between pressure injury development and potential risk factors were evaluated with t-tests and χ2 tests or Fisher’s exact test as appropriate. All analyses were performed using SAS v9.3 (SAS Institute Inc., Cary, North Carolina). Statistical significance was achieved with a two-sided p-value <0.05.
Results
Patient characteristics
A total of 674 children meeting inclusion criteria were available for review as described in Table 3. Among the 674 patients, there were some patients requiring more than one hospitalisation, resulting in 697 hospital encounters and 5918 patient days. Among the 674 patients, 117 were identified with oxygen saturations⩽90 and 557 with oxygen saturations>90. The median combined length of stay in the cardiac ICU and cardiac inpatient unit was 7 days (range: 1–143). For patients in the cardiac ICU, the median length of stay was 4 days (range: 1–71). In the cardiac inpatient unit, the median was 3 days (range: 0–74). A total number of 4603 skin assessments were documented between the cardiac ICU and the cardiac inpatient unit nurses, representing 77% of the expected assessments. The total Braden Q pressure injury risk assessment score (mean ± SD) for the cardiac ICU was 20.9 (±3.6) and for the cardiac inpatient unit it was 25.3 (±1.7).
Table 3 Admission and assessment summary.

Results per targeted data statements
Targeted data statement 1: The implementation of a preventative pressure ulcer PUP SCAMP™ or practice bundle for patients will decrease the incidence and severity of pressure injury development.
Targeted data statement 2: The use of standard positioning and assessment guidelines will reduce the incidence of skin and/or device-related pressure injury in the patient.
Targeted data statement 3: Applying standard skin care bundle for patients with a score of 1 or 2 for any Braden Q sub-scale will decrease pressure injury.
In total, 29 patients developed 30 pressure injuries, as one patient developed a pressure injury in two separate admissions during the data collection period. The majority (70%, 21/30) of the pressure injuries were related to a medical device, whereas 30% (9/30) of the pressure injuries were immobility-related, as described in Table 4.
Table 4 Pressure injury characteristics and Braden Q Scoring (total pressure injuries N=30).

CI=confidence interval; PI=pressure injury
Any subscale ⩽2 category is multi-selection
* Rounding may affect totals
Before pressure ulcer prevention SCAMPTM implementation, the overall pressure injury rate was 6.0/1000 patient days. The immobility-related rate was 1.8/1000 patient days, and the rate related to medical devices was 4.2/1000 patient days. The overall pressure injury rate while using the pressure ulcer prevention SCAMP™ was 5.1/1000 patient days (95% confidence interval (CI): 3.5, 7.3). The rate for immobility-related pressure injury was 1.5/1000 patient days (95% CI: 0.8, 2.9), whereas the rate for medical-device-related injury was 3.5/1000 patient days (95% CI: 2.3, 5.4). The overall incidence of both immobility and device-related pressure injuries in this sample was 4.4%. The incidence of immobility-related pressure injury was 1.3%, and the incidence of medical-device-related pressure injuries was 3.1%.
Overall, 12 (40%) pressure injuries were Stage I and eight (26.7%) were Stage 2 when identified. Two pressure injuries (6.7%) were staged as suspected deep tissue injuries, and eight (26.7%) were staged as mucosal membrane injury as they were on mucous membranes and medical-device-related. These findings of reduced pressure injury severity as compared with previous surveillance data suggest support for targeted data statement 1.
Of the nine pressure injuries that were immobility-related, almost half (44.4%, 4/9) were located on the occiput, 22.2% (2/9) on the back/spine, 22.2% (2/9) on the buttocks, and 11.1% (1/9) on the coccyx. Most (62%) of the medical devices associated with pressure injury were oral endotracheal tubes (9/21) and nasal endotracheal tubes (4/21). Other medical devices associated with pressure injury were peripheral vascular access hubs (3/21), oxygen saturation probes (2/21), foley hub (1/21), nasogastric tube (1/21), and continuous positive airway pressure facial mask (1/21).
Overall, 80% of the pressure injuries occurred within 7 days of the cardiac surgery, with 90% of the pressure injuries identified in the cardiac ICU.
Targeted data statement 4: The use of a perioperative risk assessment tool will reduce the incidence of pressure injury occurring in the postoperative period.
Patients (N=673) were assessed for pressure injury risk using a Perioperative Risk Assessment Scale. The majority (77.9%, 524/673) of the patients were assessed as at risk for pressure injury, with 4.4% (n=23) patients actually developing a pressure injury postoperatively. Some patients (22.1%, 149/673) were assessed as not at risk using the Perioperative Risk Scale, but 4% of these patients (n=6) did develop pressure injury during the postoperative period. The use of this tool was not found to be statistically significant (see Table 5) and did not support targeted data statement 4.
Targeted data statement 5: The intraoperative use of a Dolphin Pad™ on patients over 15 kg will reduce the incidence of pressure injury in patients during surgical procedures.
Table 5 Association between patient factors and pressure injury development.

Includes only patients (hospital admission level) with Any Braden Q Subscale ⩽2=Yes/No
If a patient ever had Any Braden Q Subscale⩽2 then the patient is in the Yes group
One patient with pressure injury was excluded because the patient had no Braden Q score information
One patient developed pressure injury in two separate hospital admissions. Both times had Braden Q score⩽2 and developed pressure injury
Include only patients (hospital admission level) with O2 saturation <90=Yes/No
One patient with pressure injury was excluded because the patient had no O2 saturation information
Inasmuch the Dolphin Pad™ (Biologics Inc., Clearwater, Florida, United States of America) is a key component of the cardiac operating room pressure injury prevention plan, this quality improvement initiative could not determine the individual impact of this intervention and provide specific data regarding targeted data statement 5.
Targeted data statement 6: A Braden Q score of 1 or 2 within any subscale will relate to pressure injury development for patients.
In all, 6% (27/448) of paediatric cardiac surgical patients who had at least one Braden Q subscale scored 1 or 2 developed a pressure injury compared with 1.3% (3/226) of patients with all subscales>2. This difference was statistically significant (p=0.005) and suggests support for this targeted data statement requiring further study. The Braden Q subscales that were more frequently scored as 1 or 2 in patients who developed pressure injuries were mobility, activity, sensory perception, and nutrition.
Targeted data statement 7: Children with a history of one or more pressure injuries are at increased risk to develop subsequent pressure injury.
Five patients had a previous history of pressure injuries, but only one patient (20%) with a previous history developed a pressure injury in this sample. This was not significantly different from the rate in patients without a history of pressure injury (4.2%, p=0.20). These findings did not support this targeted data statement, but the number of children with a history of pressure injury was small and warrants further study.
Targeted data statement 8: Patients with oxygen saturations of <90% are at increased incidence of pressure injuries.
Patients with oxygen (O2) saturations of <90% (n=117) were more likely to develop a pressure injury (p<0.0001) in this initiative. These findings are in support of this targeted data statement and warrant further study.
Targeted data statement 9: The postoperative use of a low air loss mattress overlay for cardiac surgical patients>20 kg with procedures>4 hours will decrease the incidence of pressure injury.
In total, 23 patients were on the standard hospital pressure re-distribution mattress and did not use the low air loss mattress overlay and none had pressure injury identified. Of the 45 patients who were on the low air loss mattress overlay, only one (2.2%) developed a pressure injury. There is not enough data to evaluate this targeted data statement.
Targeted data statement 10: The standardized use of gel pads under the heads of patients⩽3 years of age on advanced technological support such as extracorporeal membrane oxygenation or high-frequency ventilation will prevent occipital pressure injury.
In total, 10 patients on extracorporeal membrane oxygenation were started on the pressure ulcer prevention SCAMP™. Of these 10 patients, most (9/10) were reported to have gel pads placed under the head, with 22.2% (2/9) developing an occipital pressure injury. There is not enough data to evaluate this targeted data statement.
Targeted data statement 11: After implementation of the PUP SCAMP™ across the cardiovascular care continuum there will not be a decrease in the risk adjusted length of stay.
The bedside data collection did not support answering this targeted data statement regarding the implementation of the pressure ulcer prevention SCAMP™ and the risk-adjusted length of stay. Further study and analysis would be needed to address this targeted data statement.
Targeted data statement 12: After implementation of the pressure ulcer prevention SCAMP™ across the cardiovascular care continuum there will not be an increase in adverse events associated with pressure injury prevention strategies.
There was no baseline data for comparison with the pressure ulcer prevention SCAMP™ data to address this targeted data statement.
Diversions from pressure ulcer prevention SCAMP™
Skin assessments
In the cardiac ICU, the nurses self-reported performing a complete skin assessment 86.6% of the time. In the cardiac inpatient unit, the nurses self-reported completing skin assessments 81% of the time. A complete skin assessment included assessing the patient from head-to-toe, including both the anterior and posterior aspects. The most common reasons cited by nurses for not performing a complete skin assessment were patient-related factors of “patient too unstable” and “patient on extracorporeal membrane oxygenation”.
Prevention strategies
The frequency of nursing diversions from the pressure ulcer prevention SCAMP™ recommendations varied between the cardiac ICU and the cardiac inpatient unit nurses. In the cardiac ICU, the nurses reported diverting from the pressure ulcer prevention SCAMP™ 43% of the time. Over half (57.3%) of the diversions occurred when targeted interventions were recommended in addition to the Standard Pressure Injury Prevention Plan for any Braden Q subscale that was scored 1 or 2 and considered subscales at higher risk. The cardiac inpatient unit reported 20 diversions from the pressure ulcer prevention SCAMP™, which was less than 1% of the time. The cardiac inpatient unit nurses primarily reported following the Standard Pressure Injury Prevention Plan.
Nurses were asked to document the diversions from the pressure ulcer prevention SCAMP™. In both the cardiac ICU and the cardiac inpatient unit, the primary diversion documented were the nurses’ objection to the SCAMP™ recommendations. As shown in Table 6, the most frequent objections documented were owing to the patient not being turned hourly (n=774) or a lack of pads over a bony prominence (n=730). These recommendations were part of the additional targeted interventions if patients had a Braden Q immobility subscale score of 1 or 2, reflecting higher risk. The most common recorded diversion if the nutrition subscale was scored at higher risk was not performing daily calorie counts (n=121).
Table 6 Diversions from pressure ulcer prevention Standard Clinical Assessment and Management Plans recommendations.

The next largest diversion was noted as “Other” where the nurses were able to write in a specific reason for the diversion. As the nurses were encouraged to write in their diversions, data were collated as documented and then organised by themes. Many reasons for the diversions recorded by the nurses under “Other” were patient-related. The most common patient-related reasons were the patient was a fresh postoperative/fresh operating room case, the patient was on extracorporeal membrane oxygenation, and the patient was too unstable.
Discussion
The SCAMP™ methodology is an innovative quality improvement approach used where evidence is limited to guide care and decision-making for varying patient populations.Reference Rathod, Farias and Friedman 28 Application of the pressure ulcer prevention SCAMP™ is a nurse-driven approach to prevent pressure injury among paediatric congenital cardiac surgical patients across the Heart Center care continuum. To the authors’ knowledge, this is the largest sample (N=674) of paediatric congenital cardiac surgical patients to describe pressure injury development and prevention strategies for this vulnerable population where evidence is limited.
A total of 29 patients developed 30 pressure injuries. The majority (70%) of the pressure injuries were related to the use of a medical device, with 30% related to immobility. The overall incidence of pressure injury in paediatric cardiac surgical patients in this quality improvement initiative was 4.4%. The incidence of medical-device-related pressure injury was 3.1% and 1.3% for immobility-related pressure injuries. These data represent a decrease from the pre-pressure ulcer prevention SCAMP™ 2010 cardiac ICU incidence of 6%. The overall pressure injury rate by volume while using the pressure ulcer prevention SCAMP™ was 5.1/1000 patient days. The rate for immobility-related pressure injury was 1.5/1000 patient days, whereas the rate for medical-device-related injury was 3.5/1000 patient days. These data represent a decrease in the overall pressure injury rate before pressure ulcer prevention SCAMP™ of 6.0 to 5.1 per 1000 patient days. Immobility-related pressure injury decreased from 1.8 to 1.5 per 1000 patient days, and device-related injury decreased from 4.2 to 3.5 per 1000 patient days. These findings are consistent with other authors describing successful prevention strategies in decreasing the incidence of pressure injury in paediatric critical care patients.Reference Kiss and Heiler 1 , Reference Visscher, King and Nie 3 , Reference Schindler, Mikhailov, Cashin, Malin, Christensen and Winters 24
The majority (70%) of the hospital-acquired pressure injuries found in this initiative were medical-device-related. The pressure ulcer prevention SCAMP™ data were consistent with previous cardiac ICU surveillance, in that the majority of pressure injuries in the cardiac ICU were related to the use of medical devices. This finding was consistent with other authors who have reported that hospitalised infants and children are at risk for iatrogenic injury related to medical devices used for therapeutic interventions.Reference Schindler, Mikhailov, Cashin, Malin, Christensen and Winters 24 , Reference Fischer, Bertelle, Hohlfeld, Forcada-Guex, Stadelmann-Diaw and Tolsa 34 Medical-device-related pressure injury was found primarily on mucous membranes related to airway devices. Updated pressure injury definitions include both medical-device-related pressure injury resulting from devices designed and used for diagnostic or therapeutic indications and mucosal membrane pressure injury located on a mucous membrane where previously a medical device was in place. 4
On the basis of the pressure ulcer prevention SCAMP™ findings, nursing education and prevention efforts were revised to include skin care prevention strategies such as recommended skin assessments and need for padding under certain medical devices. As a result of this initiative, the cardiovascular nursing pressure injury prevention guidelines were modified to include the prevention strategies for medical device usage.
The severity of most of the pressure injuries identified during the SCAMP™ process was considered minor and staged as Stage 1 (40%) or Stage 2 (26.7%). Two (6.9%) potentially more serious injuries, staged as suspected deep tissue injury, were identified and additional prevention strategies and treatment were initiated to minimise further skin injury. Using the pressure ulcer prevention SCAMP™ strategy, the severity of the identified pressure injuries decreased as compared with the pre-pressure ulcer prevention SCAMP™ surveillance.
The most frequent diversion from the initial version of the pressure ulcer prevention SCAMP™ by the bedside nurse was not turning the patient hourly and lack of padding of bony prominences. Hourly position changes for patients may have been too idealistic as an intervention for many nurses to support even if the patient was scored at higher risk. On the initial version of the pressure ulcer prevention SCAMP™, a generalised statement to pad bony prominences was also used and again could not be supported by the nursing staff, as bony prominences in a child with CHD is commonly seen. The pressure ulcer prevention SCAMP™ was modified after 6 months of implementation from repositioning of patients every hour to every 2 hours and pad bony prominences with evidence of erythema or concern. Both changes increased adherence to the pressure ulcer prevention SCAMP.
Another frequent nursing diversion was a lack of a documented patient calorie count. If the patient scored at higher risk on the nutrition subscale, the pressure ulcer prevention SCAMP™ recommended a calculation of the patient’s caloric intake. This diversion reinforced the need to identify the barriers related to achieving daily calorie count calculations and identify potential resources for the nursing staff.
Many nurses recorded diversions regarding skin assessments or turning the patient. Both related to their concerns of the patient's early postoperative status, patient instability, or the patient was on extracorporeal membrane oxygenation. These recorded diversions were important to capture the clinical judgement and decisions of the bedside nurses to limit repositioning of patients related to perceived concerns regarding patient safety or instability. Some nurses’ clinical decisions may have included that the patient may not tolerate the position change or skin assessment and become haemodynamically unstable. These concerns related to patient instability and the use of some pressure injury interventions are consistent with reports by others.Reference Black, Edsberg and Baharestani 11 These nursing concerns help support the need to develop strategies for nurses to be able to readily access pressure injury prevention resources including appropriate pressure re-distribution mattresses and overlays, other pressure re-distribution support aides or surfaces, and materials such as dressings for padding bony prominences, especially for patients with limited mobility and haemodynamic instability.
On the basis of the targeted data statements, two statistically significant risk factors for the development of pressure injuries in this group of patients were any oxygen saturation less than 90%; and any Braden Q subscale scored as 1 or 2. Both of these factors need further study to help understand whether these are potential risk factors associated with pressure injury development in patients with CHD.
Limitations
A limitation of this quality improvement initiative was that the data relied on self-report from the bedside nurses, a potential for bias related to under-reporting. These data were recorded on paper, adding an additional data burden to an already busy workload for the cardiac nurses, leading to missing data. Not all patients who met inclusion criteria were included or forms were not returned, as 77% of the expected forms were returned for review and analysis. Owing to the data burden, not all of the proposed targeted data statements could be addressed in this initiative requiring further study. Another potential limitation is that an “all or none” approach was used to evaluate whether nursing staff followed the pressure ulcer prevention SCAMP™. This approach probably decreased the calculated nursing compliance rate but helped us learn from the diversions recorded by the nurses. In addition, there may have been a halo effect during the SCAMP™ implementation and data collection period, where nursing staff were aware that data were being collected about compliance, which may have affected their actions.
Next steps/future implications
Using the data from this quality improvement initiative, we have modified the current Heart Center Pressure Injury Prevention Guidelines to include the Standard Pressure Injury Prevention Plan implemented for all patients admitted to the cardiac ICU. This Heart Center Pressure Injury Prevention Guideline is linked to other hospital guidelines so that the nurses can link to other documents to select interventions to manage individual patient risk. Assessments and interventions aimed at preventing medical-device-related pressure injury have been expanded in our updated guidelines. Documentation in the electronic medical record of prevention interventions utilised for patient care has been emphasised to staff. Ongoing vigilance and surveillance of pressure injury outcomes are needed with the sharing of findings with staff important to promote positive patient outcomes and high-quality care.
Conclusions
A nurse-driven pressure injury prevention SCAMP™ supported successful evaluation of nursing practice and patient outcomes across the care continuum where evidence in the literature is limited. This programme-wide approach, along with ongoing surveillance of patient outcomes, was an important strategy to decrease the incidence and severity of pressure injuries in postoperative paediatric cardiac surgical patients. This quality improvement process yielded important data in both pressure injury development in this vulnerable population and nursing feedback regarding pressure injury prevention strategies. Identification and analysis of diversions were key, providing valuable insights regarding bedside nurses’ challenges or barriers in following a Standardized Pressure Injury Prevention Plan and additional targeted interventions, particularly in the cardiac ICU. Review of nursing practices highlighted opportunities to standardise and focus pressure injury prevention interventions as well as ensure communication of patient vulnerabilities. As a result, the Heart Center Pressure Injury Prevention Guidelines were modified, incorporating staff feedback. Continuing vigilance and surveillance of pressure injury outcomes are needed in this vulnerable paediatric population.
Acknowledgements
The authors would like to recognise the 13 members of the expert panel who developed the first nursing SCAMPTM and laid the groundwork that made this project possible. They also thank the staff nurses of the cardiac ICU and cardiac inpatient unit for their assistance with the data collection required to conduct this important project.
Financial Support
This project received no specific grant from any funding agency or from commercial or not-for-profit sectors.
Conflicts of Interest
None.
Ethical Standards
The pressure ulcer prevention SCAMP was considered exempt by the organisation’s Institutional Review Board as it was deemed quality improvement.