This article is on a national framework for the sustainability of health knowledge translation (KT) initiatives in Uganda. It is consequently based on an evidence brief from the best available literature on the design and implementation of policies for the sustainability of KT initiatives in Uganda's health system. Several different terms are used in this study: “knowledge translation” refers to the dynamic and iterative process involving the synthesis, dissemination, exchange, and ethically sound application of knowledge to improve health, provide more effective health services and products, and strengthen healthcare systems (Reference Graham and Tetroe1). Similar terms used in related literature include “knowledge brokering”, “knowledge exchange”, and “knowledge mobilization”, refer to the same knowledge sharing activities (2). KT strategies are used in public health to promote Evidence-Informed Decision Making (EIDM).
In the context of this study, EIDM refers to the incorporation of the best available research evidence into public health policy and program decision making. The term “sustainability” is defined as the ability to maintain programming and its benefits over time at a certain rate and level. It involves the existence of structures and processes that allow a program to leverage resources to effectively implement and maintain evidence-based policies and activities. Sustainability includes organizational and systems dimensions (Reference Gruen, Elliott and Nolan3;Reference Schell, Luke and Schooley4). It also pertains to program sustainability, which is defined as the ability to maintain programming and its benefits over time (Reference Calhoun, Mainor, Moreland-Russell, Maier, Brossart and Luke5).
Current Healthcare Status and System in Uganda
The World Bank Report of 2017 indicates that Uganda is a low income country with income per capita of USD 653. Consequently, the Uganda Health Sector Development Plan 2015/16-19/20 points out that the average national literacy rate is at 73 percent, whereas the maternal and infant mortalities are at 336/100,000 and 43/1,000 live births, respectively. The health sector is pluralistic with 55 percent of the services provided by the government owned facilities and conversely 45 percent are privately owned. The services are decentralized with the central system being responsible for policy and referral care while the district system is responsible for implementation of healthcare services (6). A diagrammatic presentation of the Ugandan health system is in Figure 1.

Figure 1. Uganda health system.
The total health expenditure in Uganda is only USD 53 per capita, with households contributing 38 percent, donors 47 percent, government 15 percent, and health insurance less than 1 percent. Moreover, the contributions by households are largely out-of-pocket and are far above the maximum of 20 percent recommended by World Health Organization (WHO) for the households not to be pushed into impoverishment. The funding from donors is mostly off-budget (6). The World Bank points out that the hospital beds per 1,000 people in Uganda was last measured at 0.50 in 2010. Hospital beds include inpatient beds available in public, private, general, and specialized hospitals and rehabilitation centers. These include beds for both acute and chronic care (Reference Cordero7).
The Sector Development Plan further underscores the shortage of health workers as a major challenge in improving the health of the population with the doctor to population ratio is 1:18,000. In addition, the ratio of traditional medicine practitioners to population is between 1:200 and 1:400. Worse still, the health worker to population ratio in Uganda is 1.55 health workers per 1,000 persons compared with the WHO guideline of a minimum of 2.28 per 1000 persons (6). The public direct investment in health research is negligible despite the resolution by WHO. Accordingly, the proportion of the health sector budget earmarked for research is unknown but seemingly very low. The national share of expenditure on research and development as a percentage of GDP is 0.3 percent (8). Moreover, the level of research funding is not yet 2 percent of the MoH budget as per the Bamako Plan of Action by WHO. Worse still, government has failed to operationalize the Uganda National Health Research Organization; the only full time staff is the Director General (9).
The purpose of evidence informed policy making is to optimize patient and population health outcomes (Reference LaRocca, Yost and Dobbins10;Reference Lavis, Robertson and Woodside11) and the approach has the potential in low and middle income countries to reduce morbidity and mortality. Bridging the gap between “knowing” and “doing”, however, is undoubtedly a challenge (Reference Cordero7). A systematic review by Lavis et al. (2005), for instance, highlights the difficulties policy makers face in accessing and using research evidence for policy making (Reference Lavis, Oxman and Denis12). Translating the best available research evidence into programmatic change is a complex process (Reference Lavis, Robertson and Woodside11). Barriers to EIDM include a lack of financial incentives at different levels within healthcare systems; limited access to research evidence; and the lack of equipment needed for implementation in healthcare organizations. The required equipment includes tools and materials such as computers (including those with high capacity for data mining and manipulation) and internet servers. Furthermore, existing standards used by healthcare teams may not be in line with the recommended practice. Individual healthcare professionals may also lack the knowledge, attitudes, and skills needed to critically appraise and use evidence. Lack of time among health personnel and a resistance to change are also known barriers to EIDM (Reference LaRocca, Yost and Dobbins10;Reference Dobbins, Hanna and Ciliska13;Reference Straus, Brouwers and Johnson14).
In their study on healthcare technology transfer in Latin America, Coe and Banta (1992) observed that there is no link between the development of activities for generation of knowledge and evolution of technologies in developing countries. They attributed this to limited human, financial resources, and technological dependence on developed countries. Coe and Banta also elaborate that 97 percent of the Worlds’ expenditure for research and development was spent in developed countries and less than 1 percent in Central and South America. More so, 0.3 percent of the gross national product was spent on research and development compared with a global average of 2 percent. This study further recommended that to meet these challenges, there must be a strong commitment by institutions from different sectors such as Ministries of Health, Councils for Science and Technology, Schools of Medicine and Public Health, other national agencies, and international organizations (Reference Coe and Banta15).
This study focuses specifically on the issue of the sustainability of KT activities related to the health systems building blocks: health services delivery including health education, human resources for health (for example, issues such as health worker staffing) and commodities (such as equipment and medicines) in Uganda. Other health systems issues considered are the healthcare information system, the effective financing of health services, leadership, and governance.
METHODS
We searched for and reviewed evidence about KT sustainability issues in Uganda, the impacts of options, barriers to implementing these options, and implementation strategies to address such barriers. This entailed review of published documents relevant to the national framework for the sustainability of health knowledge translation initiatives in Uganda from 2010 to 2017. The year 2010 marked the beginning of some knowledge translation initiatives for supporting evidence informed health system policy making in Uganda (16–Reference Mutatina, Basaza, Obuku, Lavis and Sewankambo19). The 2005 Arksey and O'Malley methodological framework for scoping reviews was used to develop our research questions, identify relevant documents, screen and select the documents (Reference Arksey and O'Malley20).
In determining the research questions, the breadth of coverage and its defined relevant aspects were ensured. The research questions were: what are the relevant documents to the national framework for the sustainability of health knowledge translation initiatives so that KT can inform health policy, strategies, practices, public opinion, and social transformation? What is the available literature on advocacy on the importance and use of KT? How can KT be institutionalized? How can capacity be built for researchers and research users? The results of the document search process and screening are presented in Figure 2.

Figure 2. Results of document search and screening.
The review followed several steps: (i) Selection of Web sites of relevant government institutions, international and national nongovernmental organizations using Google. Given that different Web sites were organized differently, specific search strategies were devised for each Web site depending on its specific navigability. In addition, the following keywords were used in various combinations with Boolean operators (and, or): Uganda, knowledge translation, sustainability, national framework, initiatives, and health system (Reference Robb and Shellenbarger21). (ii) Identification and characterization of published documents relevant to the sustainability of health knowledge translation initiatives (Table 1). (iii) Checking of reference lists of selected documents to expand the list of documents included. More so, to minimize selection bias, two independent reviewers (A.K. and R.B.) screened all documents and selected the most appropriate to answer the research questions. Documents that were at the draft stage were excluded. Furthermore, two independent reviewers (R.B. and B.M.) carried out the final analysis.
Table 1. Institutions / Organizations Whose Web Sites Were Searched and When

Key informant interviews were conducted in mid-2013 and a policy dialogue was held in early 2014 and 2015. An expert working group guided this research. Additional information on how this policy brief was prepared is available as Supplementary Material.
THE PROBLEM
Uganda has no explicit sustainable system for KT activities that would ensure that KT can inform health policy, strategies, practices, public opinion, and social transformation. The Uganda National Health Research Organization which is responsible for health research sometimes plays a key role in KT activities—the Director General of Uganda National Health Research Organization (UNHRO), for example, is one of the investigators of the SURE project. However, in many other KT undertakings in Uganda, UNHRO is not involved (Reference Basaza, Nabudere and Sewankambo22).
Causes of the Problem
The stakeholder interviews and the Ugandan-based KT studies identified several causes for this problem (Reference Basaza, Nabudere and Sewankambo22;Reference Ssengooba, Atuyambe and Kiwanuka23). These are presented in this section, and the findings supplemented by material from additional published literature.
Lack of Advocacy and a Limited Capacity to Use Evidence:
The interviews conducted with stakeholders revealed that there is no specific unit in the Ugandan health sector with responsibility for coordinating and synthesizing research. The use of KT is not well established in the country. Furthermore, the connection between researchers and KT intermediaries on one hand, and decision makers on the other hand, is inadequate. Advocacy work for health research and KT in the health sector in Uganda is limited, and the communication of research findings is not well designed for the needs of particular audiences, particularly those of decision makers.
There are also limited opportunities for researchers, policy makers, practitioners and implementers to meet on common ground. KT is still in its infancy in Uganda and, therefore, not well understood or well received. Ugandan policy makers and practitioners, including top and mid-level health services managers, have received limited training in evidence-based decision making. Within Uganda's decentralized healthcare system, districts and municipalities make by-laws and other policies, but they do not have specific units that can address their KT needs (Reference Basaza, Nabudere and Sewankambo22;Reference Ssengooba, Atuyambe and Kiwanuka23).
A study of research, evidence and policy making in Uganda has noted the limited capacity among policy makers and practitioners in research processes, interpretation, synthesis, and application of evidence. This same study emphasized that policy makers, practitioners, and decision makers in Uganda are reluctant to use evidence. Other studies have echoed these findings, and stressed the importance of capacity building in KT among policy makers and practitioners to increase the uptake of evidence (Reference Bowen and Zwi24;Reference Lavis, Lomas, Hamid and Sewankambo25). In his assessment of provincial and national efforts to link research to action, Lavis (2006) points out that KT is still new and that there is need for skills-development programs for researchers to develop their capacity to execute evidence-informed KT strategies. Similarly, skills development programs are also needed for research users to enhance their capacity to acquire, assess, adopt and apply research to enhance the use of KT (Reference Lavis, Lomas, Hamid and Sewankambo25). It is likely that when the use of research evidence increases substantially, issues related to the sustainability of KT platforms will be given far greater attention (Reference Basaza, Nabudere and Sewankambo22).
Lack of a Framework for KT:
Currently, the country frameworks and platforms for KT lack both a sustainability mechanism and a system mechanism to ensure the sustained coordination of existing national health KT platforms. Instead, multiple players continue to work within their own domains (Reference Basaza, Nabudere and Sewankambo22). In their research on examining the knowledge infrastructure of healthcare systems, Ellen et al. (2011) and Lavis (2013) argue that a framework should include the broad domains of research production, and activities linking research to action and evaluation (Reference Ellen, Lavis and Ouimet26;Reference Lavis27). Jacobson et al. (2003), in contrast, propose going further, and argue that a framework should consist of five domains: the user groups, the issue, the research, the knowledge translation relationship, and the dissemination strategies (Reference Jacobson, Butterill and Goering28).
Funding and Other Resources for KT
The current scattered KT efforts in Uganda are largely donor funded; no KT efforts receive earmarked government funding (Reference Basaza, Nabudere and Sewankambo22). This means that, at present, there is no stable funding or capacity to expand and sustain the current/past level of capacity or current priority setting and governance, or the defined relationships between the Ministry of Health and other stakeholders (Reference Robb and Shellenbarger21). However, this finding is not unique to Uganda; similar situations prevail in the six SURE project countries. Government funding for KT is limited but Lavis (2013) notes that institutions involved in KT could raise money through peer-reviewed grant competitions such as those held by the McMaster Health Forum in Canada. McMaster Health Forum is a research institution operating at regional/provincial levels and at national level that harnesses information, convenes stakeholders and prepares action-oriented leaders to meet pressing health issues creatively (Reference Jacobson, Butterill and Goering28).
Holmes et al. (2012) further suggest that organizations involved in KT could use current resources while at the same time developing the internal and external resources and partnerships needed to develop and implement KT (Reference Holmes, Scarrow and Schellenberg29). Health programs dependent on international funding are hard to sustain because of the complexities of sustaining resource flow, and this increases the difficulty of aligning health programs and the powerful stakeholders involved (Reference Gruen, Elliott and Nolan3). Research funders might seek to promote KT directly by developing their own knowledge translation strategies, and disseminating information about funded and completed research. This could include involving end users in the prioritization of research topics (i.e., commissioned research), and funding implementation research, that is, the scientific study of methods to promote the use of research findings in practice (Reference Arksey and O'Malley20). This may be a useful approach given that national agencies may be more motivated to engage in local KT activities than international funding agencies which may not be familiar with the realities of specific KT-related issues at the country-level (Reference Cordero7).
POLICY OPTIONS
In this section, we present three policy options. These are based on the findings of our problem analysis, our interviews with stakeholders and the results of Ugandan-based KT studies (Reference Basaza, Nabudere and Sewankambo22;Reference Ssengooba, Atuyambe and Kiwanuka23), supplemented by findings from additional literature and the issues raised in a deliberative policy dialogue. The three options presented are complementary, with the primary aim of ensuring the optimal use of research evidence as a vital input in policy making, policy process evidence, informed decision making, and, ultimately, more efficient and effective care. These options, we suggest, could be considered by policy makers, practitioners, and other stakeholders as they develop a national strategy for the sustainability of KT initiatives in Uganda. It should be noted that only a minimal amount of published research evidence was found that related to these options, including their feasibility and impacts. Material from our key informant interviews and the deliberative policy dialogue were, therefore, significant elements in the process of selecting and describing these policy options.
Policy Option 1: Advocacy on the Importance and Use of KT
The UNHRO could work closely with people across the health sector to identify potentially useful KT champions. The champion could carry out advocacy work or dissemination or the promotion of KT evidence. Currently, the country lacks a clearly identified champion for the promotion of KT sustainability. Gruen et al. (2008), in their systematic review of an integrated approach for the sustainability of health program planning, cite evidence from several studies indicating that one of the main factors negatively affecting the sustainability of programs is the absence of a KT champion (Reference Gruen, Elliott and Nolan3). They suggest that it is strategically advantageous to have such champions from the upper or middle management of an organization. One type of KT champion, for example, could be a politician who has expertise in the health sector and who recognizes the value of using research evidence.
Information needs to be disseminated on what KT can provide to the President of Uganda, the Ugandan Cabinet, Parliament, and to politicians in general, policy makers, practitioners, and implementers. The sector could solicit a political commitment to request evidence in the health sector and the media sector could also be involved. Knowledge brokers could hold regular media conferences about KT. Clear, simple language should be used in communications from researchers, knowledge brokers, social media, and Web-based communication channels should be considered. One of the key elements of this policy option could be exploring of the linkages between KT in the health sector and KT in other sectors. The linkages could be building points for a framework for inter-sectoral cooperation for the delivery of holistic health services and possible benefits of comprehensive and efficient services. The health sector could also rally support from health professionals and civil society organizations to mobilize resources for KT (Reference Basaza, Nabudere and Sewankambo22).
Policy Option 2: Institutionalize KT
An operational framework could be put in place to institutionalize KT. UNHRO and the entire sector could explore different governance and financial arrangements, outputs, and activities and evaluate how these can be delivered. This policy option could also involve the development of a KT framework which could be a platform for a clearing house or a coordination structure/unit or both. The government structure for handling KT activities could either be UNHRO itself or a public university. The Uganda National Health Research Organization Strategic Plan 2010–2014 provides for the establishment of a national KT platform for health research evidence and application. Large units in the health sector, such as the Mulago National Referral Hospital, should be provided with their own KT units. UNHRO could work in conjunction with the Uganda National Academy of Sciences, the Uganda National Council of Science and Technology and other institutions that are involved in KT (Reference Basaza, Nabudere and Sewankambo22).
The government could also budget for KT using consolidated funds—an approach which would be in keeping with the Algiers declaration that called for narrowing the knowledge gap to improve health development and health equity in the African region (30). The health sector could also explore the use of a business model for funding KT services in institutions in need of services from an established KT unit. This business model approach is already successfully used, for example, by the National Institute for Health and Care Excellence of Department of Health in the United Kingdom that is responsible for providing national guidance and advice to improve health and social care (31).
Policy Option 3: Capacity Building for Researchers and Research Users
In this third policy option, the sector could carry out orientation in research and KT (especially for politicians), and facilitate stakeholder involvement. This option would involve working out the modalities of appointing a team with the right skills and expertise in KT. The team could be mentored, and provided with tailored leadership skills training about the use and sustainability of KT. Partnerships between researchers, policy makers and practitioners, decision makers, and other stakeholders should be established. Those in the health sector could conduct training for researchers, policy makers, and decision makers in KT, focusing particularly on the training of mid-level managers, especially among District Health Teams. Attention should also be given to building the capacity of researchers to write policy briefs and to communicate the messages in them. A strategy outlining how KT could benefit frontline workers should be developed. The involvement of committees from the inception of KT activities could be important as a way of encouraging the use of research evidence and could also help to identify key lessons for enabling KT sustainability (Reference Basaza, Nabudere and Sewankambo22).
IMPLEMENTATION CONSIDERATIONS
There is little detailed published evidence available about the three policy options described here. Published evidence about the potential barriers to KT implementation, and other related implementation considerations is similarly scarce. Despite these limitations, in Figure 3 we have presented the key factors identified in our analysis related to the development of policy options for KT sustainability. This is a modification of Gruen et al. (2008) model developed as part of their study of the sustainability of health program planning (Reference Gruen, Elliott and Nolan3) and has been adapted both to the specific Ugandan context and to the topic of KT sustainability. The modified model takes into consideration both the context of the KT as well as the resources available, and the stakeholders involved (including the above-mentioned KT “champion”).
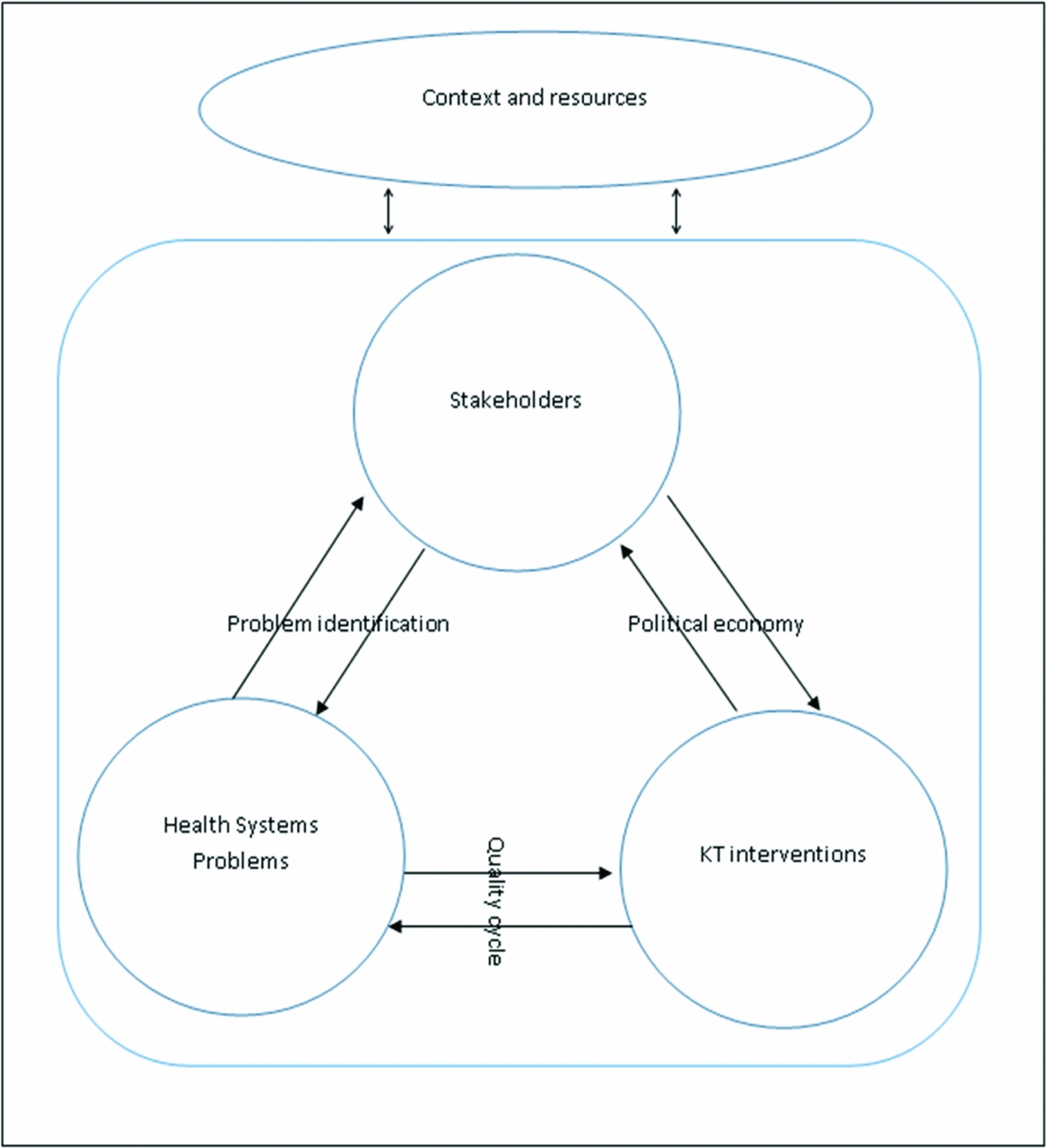
Figure 3. A proposed system for KT sustainability.
The sustainability of KT activities in Uganda will depend on prevailing national and international socio-cultural, political, economic, and geographical, Uganda's policy contexts, and environmental issues, as well as issues related to partnerships. Health system concerns related to national and international research policy will also affect KT sustainability in Uganda. Exactly how UNHRO will implement Uganda's national health research policy and strategic plan will also affect KT activities within the country.
Furthermore, the availability of resources for KT will impact on issues of sustainability and feasibility. Other key interventions that could be considered are those related to KT advocacy, communication and program design. Stakeholders involved in the sustainability of KT in Uganda could include funders (especially donors and the government of Uganda), the managers and staff of current KT initiatives, and policy and evidence informed decision makers. Other stakeholders could include communities and community leaders affected by such policies and decisions. The key donors in the field of KT in Uganda have been the European Union, and bilateral development agencies and research organizations from Norway and Canada. Thus, so far, the government of Uganda has not directly funded KT (Reference Basaza, Nabudere and Sewankambo22).
Furthermore, the sustainability of KT will be influenced by the way leaders in the health sector in Uganda understand and appreciate the value of evidence in informing decisions. In addition, donor funds are affected by the broader political economy and its impacts on donor governments and multilateral institutions such as The World Bank, the European Union, and other partnering organizations involved in implementation. Gruen et al. (2008) point out that the demonstration of positive effects (or otherwise) from KT interventions will also affect resource mobilization for KT (Reference Gruen, Elliott and Nolan3).
KT advocacy or communication interventions, the training of stakeholders, and program monitoring and evaluation are also likely to impact on the sustainability of KT in Uganda. Stakeholders, KT interventions, and health system concerns impact upon each other. An understanding of health system concerns necessarily informs which KT interventions are chosen and modifies the understanding and responses of stakeholders. The health system problems inform KT interventions and well conducted KT in turn modifies the health system problem. The perceptions of health system problems depend on how policies and decisions are perceived. In the same vein, the definition of the health system problem is subjective, depends on the stakeholder and is complex and bidirectional (Reference Gruen, Elliott and Nolan3).
This study has outlined 3 policy options for the use of KT, KT sustainability, and further KT research. These can be applied within the Ugandan health sector as well as other countries with similar settings.
NATIONAL POLICY DIALOGUE
This policy for evidence was discussed as a background document at a policy dialogue meeting held in Kampala, Uganda, in early 2014. Participants at this meeting included technical staff from the World Health Organization country office in Uganda, the Ugandan Ministry of Health, members of the Parliament of Uganda, and academics. The participants came from diverse professions, and included economists, sociologists, physicians, policy analysts, and health planners. The objectives of the dialogue meeting included reviewing this brief and deciding on a way forward. At the meeting, it was observed that the concept of KT was new to many participants attending the policy dialogue, and a brief summary about KT was requested by them. The purpose of KT, as explained, was to use research findings to inform policy.
It should be noted that a disconnect between researchers and policy makers may occur in Uganda if researchers in our country are guided by their research agendas without regard to the needs of policy makers, especially those in the Ugandan Ministry of Health (MoH). Researchers should consult with the MoH at the design stage of their research projects to ensure a better uptake of their research evidence. At the dialogue meeting, participants proposed that a KT desk be established under the control of the Policy Analysis Unit at the MoH. This was recommended because the unit interfaces with the Ugandan Parliament and has links to the MoH and other decision makers.
Some participants suggested that searching for an individual KT “champion” carries potential risks if, for example, the individual is a politician who might later leave their position. It was suggested, therefore, that consideration might be given instead to establishing and supporting a KT office or a wider supportive institutional framework. It was also noted that to sustain KT in Uganda, the Ugandan government should provide money for health research in the national budget. This money could also be supplemented by donors.
CONCLUSION
Uganda and several developing countries with similar settings have no explicit sustainable system of KT activities that would ensure that KT informs health policy, strategies, practices, public opinion, and social transformation. More so, there is no mechanism to coordinate the existing national health KT platforms. The problems identified with the Ugandan KT system were: the absence of a specific unit within the health sector to coordinate and synthesize research; lack of familiarity with KT activities and, rare use of it. These findings apply to the entire healthcare system in Uganda and cut across the central and lower levels. The sustainability of KT will be influenced by the prevailing context and concerns within healthcare both in Uganda and internationally. Lastly, the availability of resources for KT advocacy, communication and program design will impact on the sustainability of Uganda's KT activities.
SUPPLEMENTARY MATERIAL
Supplementary Material 1: https://doi.org/10.1017/S0266462317004482
CONFLICTS OF INTEREST
The authors’ institution received funding from the European Commission's 7th Framework Program. Dr. Basaza reports grants from European Union, during the conduct of the study. Dr. Kinegyere has nothing to disclose. Mr. Mutatina reports grants from European Union, outside the submitted work.






